Speech and language development in children with 49,XXXXY syndrome
Funding information: Focus Foundation
Abstract
49,XXXXY is the rarest X and Y chromosomal variation and is frequently characterized by expressive and receptive language dysfunction, low muscle tonus, and intellectual deficits. Due to the low incidence of this disorder, comprehensive studies analyzing the specific aspects of the speech and language phenotype in these boys have been uncommon. This is the first in-depth investigation of the speech and language profiles in a large cohort of boys with 49,XXXXY. Based on the clinical judgment of speech and language pathologists, there was an increased incidence (91.8%) of Childhood Apraxia of Speech (CAS), which has not been previously described in this disorder. In preschool boys, some significant differences were demonstrated between boys who received early hormonal treatment (n = 16) and untreated boys (n = 4) on the language scales (p = .047) on the Bayley Scales of Infants and Toddlers, as well as significant differences between treated (n = 13) and untreated boys (n = 8) on the Expressive One Word Picture Vocabulary Test (p = .008). No significant differences between treatment groups were found in school age children, however, treated groups demonstrated less discrepancies between expressive and receptive language. More research and larger samples are needed to determine the extent of the impact of testosterone treatment on boys with 49,XXXXY. This study identifies CAS as a potential explanation for the significant expressive language dysfunction and subsequent behavioral dysfunction. These findings may assist in facilitating more targeted treatment and improved outcomes for boys with 49,XXXXY.
1 INTRODUCTION
49,XXXXY is currently estimated to occur in 1:85,000 to 1:100,000 live male births (Kleczkowska, Fryns, & Berghe, 1988; Linden, Bender, & Robinson, 1995; Peet, Weaver, & Vance, 1998). Although the speech and language profile and cognitive capabilities of 49,XXXXY have not been well characterized in the research literature, limited or no expressive speech with better receptive language development is commonly described. Since its earliest description more than 50 years ago, the severely delayed expressive skills, uneven and irregular rate of speech acquisition, and reduced intelligibility in comparison to comprehension skills and intellectual ability have been perplexing and not well understood (Burgemeister et al., 2019; Curfs, Schreppers-Tijdink, Wiegers, Borghgraef, & Fryns, 1990; Lomelino & Reiss, 1991). Curfs et al. examined five boys with 49,XXXXY, all of whom had articulatory dysfunction. While one of the boys had no noted delay of their expressive language capabilities, two cases utilized only incomplete or limited sentences and the other two boys were only able to produce simple sounds. The specifics of the articulatory features were not detailed in this investigation. Another case study of two school-aged males with 49,XXXXY and one child with 48,XXXY/49,XXXXY mosaicism indicated that receptive language was within normal limits, while expressive language remained significantly below average (Lomelino & Reiss, 1991). Standard scores for both boys on the Vineland demonstrated statistically significant weaknesses in communication when compared to overall developmental performance. Patient one scored in the mild deficit range and patient two was in the moderate deficit range with documented misarticulations. Significant delays have also been noted in spoken language with the age of spoken first words ranging from 15 months to 3 years of age (Burgemeister et al., 2019). Reduced expressive language skills may influence peer interaction and social development as the children mature (Linden et al., 1995) and may be accompanied by behavioral frustration and externalizing behaviors.
Due to the well-documented testosterone deficiency, receiving testosterone at the onset of puberty has been common practice in 47,XXY and its variations, such as 49,XXXXY. Although not standard of care, hormonal treatment using testosterone has been associated with significant improvements in neurodevelopmental and behavioral outcomes in males with 47,XXY as well as 49,XXXXY for over 25 years (Galasso, Arpino, Fabbri, & Curatolo, 2003; Linden et al., 1995; Mazzilli et al., 2016; Patwardhan, Eliez, Bender, Linden, & Reiss, 2000). Studies in recent years have begun to investigate the possible benefits of testosterone treatment at younger ages in these disorders as well, including early hormonal treatment in infancy (Samango-Sprouse et al., 2013, 2015, 2020) and hormonal booster therapy in later childhood (Samango-Sprouse et al., 2018; Samango-Sprouse, Lasutschinkow, Powell, Sadeghin, & Gropman, 2019; Tran, Samango-Sprouse, Sadeghin, Powell, & Gropman, 2019).
While many studies on the impact of testosterone have been completed on 47,XXY, studies on 49,XXXXY have been mostly limited to case studies, incidental reports, and small sample sizes. Several case studies report that boys who received testosterone replacement exhibited improvements in overall wellbeing and mood, as well as changes in multiple domains of development, including language and behavior (Galasso et al., 2003; Mazzilli et al., 2016). Linden et al. (1995) conducted a case study of three patients with 49,XXXXY in which all three boys presented with externalizing behaviors associated with reduced expressive language abilities (Linden et al., 1995). With testosterone treatment, researchers reported improvements in social expression. The implementation of testosterone replacement therapy has also been associated with a beneficial impact on the language deficits associated with 49,XXXXY, however existing studies have not investigated its affect on speech skills or reported on the incidence of motor speech disorders in this population (Mazzilli et al., 2016; Samango-Sprouse et al., 2011). In a study of 22 infants and toddlers with 49,XXXXY, Samango-Sprouse et al. found that boys who had received early hormonal treatment had significantly higher scores on the Preschool Language Scale, fourth Edition in both auditory comprehension and verbal ability in addition to higher expressive and receptive capabilities on the Expressive and Receptive One Word Picture Vocabulary Test—Revised. Further studies are necessary to investigate whether the impact demonstrated in this study is also seen in older children with 49,XXXXY and whether repeated dosages have similar positive effects to those that have been documented in 47,XXY. In addition, these studies only described the articulation deficits and expressive language delays seen in 49,XXXXY and did not investigate the possible etiologies of these deficits.
Although 50 years of case study research have reported the delayed and deficient speech typically present in boys with 49,XXXXY, the etiology of these deficits remains elusive. Additional investigation is warranted to fully comprehend the speech and language phenotype associated with 49,XXXXY. With a greater understanding of the etiology of the speech and language profile, well designed, targeted treatment may be crafted for males with this disorder. This study investigates the early speech and language phenotype of boys with 49,XXXXY based on the cross-sectional, multidisciplinary research completed in a large, international cohort.
2 METHODS
2.1 Study subjects
Eighty-five boys with 49,XXXXY were seen by a multidisciplinary team of specialists as part of an annual conference for children and families hosted by the Focus Foundation in collaboration with the Neurodevelopmental Diagnostic Center for Children. The diagnosis of 49,XXXXY was confirmed by chromosomal analysis via prenatal diagnostic testing, or chromosomal microarray or karyotype postnatally. Participants were from multiple countries, including the United States, Canada, UK, the Netherlands, Italy, Puerto Rico, and Belgium.
Due to availability, compliance, and individual capabilities of the child, not all assessments were completed by each child and not all children were in attendance each year. In order to better elucidate natural history, the examination of children with multiple visits was utilized in the appropriate age category based on their chronological age at the time of their visit.
These multidisciplinary evaluations were conducted in a variety of private clinic settings over the last 16 years. The primary sites were located in Annapolis, Maryland and Crofton, Maryland, however in the last 6 years, the conference has also been available at clinic sites in the UK and Italy. The two-day conference includes 1 day of talks and presentations which discuss the current research in 49,XXXXY and 1 day in which the specialists meet with the children and their families in order to complete the research investigations and observations on the children.
The speech and language team included two pediatric speech and language pathologists, a motor based pediatric speech and language pathologist, a neurodevelopmentalist, and a pediatric neurologist/clinical geneticist. The clinic in Italy included an additional Italian speech and language pathologist who evaluated the primarily Italian speaking participants for the presence of Childhood Apraxia of Speech and flaccid dysarthria. Due to a lack of access to assessments that were standardized for primarily Italian speakers at the time of the conference, the language of these children was not formally assessed or included in any results.
Testosterone treatment status was dependent on the physical examination and recommendation of the child's individual pediatric endocrinologist. Based upon treatment status at the time of evaluation, participants were segregated for analysis. Early hormonal treatment (EHT) is defined as three 25 mg intramuscular injections of testosterone enanthate received between birth and 24 months of age. Hormonal booster treatment (HBT) is defined as three 50 mg intramuscular injections of testosterone enanthate typically received between the ages of 5 and 8 years of life. Children who received both EHT and HBT were segregated into a third group, E&B.
2.2 Editorial policies and ethical considerations
Informed consent was obtained from each parent of all participants under the study protocol approved by the Western IRB (#20081226).
2.3 Clinical assessment
Of the 93 children seen in the multidisciplinary clinic, 67 completed age-matched standardized clinical assessments.
The Bayley Scales of Infant and Toddler Development were utilized to assess speech and language development in children from birth to 42 months of age (Bayley, 1993; Bayley, 2005).
The Preschool Language Scales (PLS) for patients from birth to 7 years, 11 months were used to determine auditory comprehension and expressive communication development (Zimmerman, Steiner, & Evatt Pond, 2002; Zimmerman, Steiner, & Evatt Pond, 2011).
The Expressive One-Word Picture Vocabulary Test (EOWPVT) and Receptive One-Word Picture Vocabulary Test (ROWPVT) evaluate expressive and receptive vocabulary skills in children over 2 years of age (Brownell, 2000a; Brownell, 2000b; Martin & Brownell, 2011a; Martin & Brownell, 2011b).
The Early Language Milestones Scale-2 (ELM-2) evaluated speech and language skills from birth to 3 years of age (Coplan, 1993).
Each of the standardized assessments are age-normed tests for primarily English speaking individuals and results reported are all standard scores. Of the 68 children who completed the standardized assessments, 91% were primarily English speaking and 9% spoke English as a second language. A standard score of 100 is considered average (50th percentile), with a typical standard deviation of 15. Scores between 85 and 115 are considered within normal limits, with 85 on the low-end and 115 on the high-end of average. Any scores above 115 are considered above average. Scores between 70 and 85 are considered below average and borderline impaired. Scores between 55 and 70 are considered mildly impaired and scores below 55 are considered moderately impaired.
2.4 Speech diagnosis evaluation
Sixty-nine boys underwent a speech diagnosis evaluation to determine the presence of Childhood Apraxia of Speech (CAS) and, of those, 21 were able to be assessed for that presence of flaccid dysarthria.
Childhood Apraxia of Speech is a speech and motor planning disorder that is characterized by a severe speech delay with inconsistent distortions, misarticulations, and omissions of sounds (Davis, Jakielski, & Marquardt, 1998; Shriberg, Aram, & Kwiatkowski, 1997; Strand, Shriberg, & Campbell, 2003). CAS is often accompanied with developmental dyspraxia and is associated with delayed speech milestones and a limitation in the number of spoken words due to a difficulty in moving smoothly between sounds.
Flaccid dysarthria is a motor speech disorder that can affect phonation, articulation, and respiration. It is characterized by a slurring and slowing of one's speech and can also include hyponasality. Low oral musculature is often recognized in individuals presenting with flaccid dysarthria.
Each child received an oral motor and speech evaluation tailored to their age and completed by a licensed pediatric speech and language pathologist (SLP) experienced in motor-based speech disorders. The SLPs followed the official American Speech-Language = Hearing Association (ASHA) consensus criteria for the purpose of diagnosis in this study in addition to utilizing the Mayo 10 Clinical Signs for Childhood Apraxia of Speech. ASHA has reported that, while there are no specific standardized assessments or list of exact diagnostic features to diagnose the presence of Childhood Apraxia of Speech, there are three main characteristics of CAS based on their consensus criteria (ASHA, 2007) that should be utilized by a speech and language pathologist when determining a diagnosis. These features include inappropriate prosody, disrupted co-articulatory transitions, and inconsistent errors in speech during repetition of words. ASHA also lists multiple errors in speech sounds, unintelligibility, disfluency, and reduced phonetic inventories as additional features seen in individuals diagnosed with CAS (ASHA, 2007). There is no specific number of features needed to make a diagnosis in either the clinical or research domain at this time. However, for the purpose of this research, an adaptation of the Mayo 10 Clinical Signs for Childhood Apraxia of Speech was used to identify the presence of CAS (Shriberg et al., 2017). Using this classification system, a diagnosis of CAS was made if four or more of the following characteristics of CAS were demonstrated during the evaluation: vowel distortions, distorted substitutions, difficulty with initial or transitionary articulatory configurations, lexical/phrases stress errors, syllable/word segregation, groping, intrusive schwa, voicing errors, slow speech rate or slow DDK, increased difficulty with multi-syllabic words, and inconsistency on repeated trials of words/utterances. Based upon this evaluation, in addition to the results of the clinical speech assessments and an in-depth developmental history provided by the family, specialists determined the presence or absence of motor-based speech disorders including CAS and flaccid dysarthria.
While this method was utilized in order to determine the presence of CAS, it was not until recently that the research specialists began noting which specific characteristics were present in each of the participants. Further efforts are underway to collect these specific occurrences of characteristics to better understand which, if any, be more apparent than another in children with 49,XXXXY.
2.5 Oral motor evaluations
While in-depth oral motor evaluations have been utilized each year in order to diagnose CAS and flaccid dysarthria, our specialists have recently begun documenting the specific oral movements of each child during the evaluations in order to further investigate the speech and language phenotype of boys with 49,XXXXY. Oral motor planning capacities were assessed and reported on in 26 boys by evaluating muscle tonus in the oral facial area and imitative capacities of the tongue movements such as elevation, protrusion, lateral movements, and puckering and pursing of lips. Articulation capacities and speech intelligibility also were assessed.
2.6 Statistical analysis
The subjects were bifurcated by age: preschool (birth to 5 years of age) and school-aged (5–11 years of age). In the preschool-aged group, the Mann Whitney U Test compared testosterone and Non-T groups on the Bayley, the EOWPVT and ROWPVT, the ELM and the PLS. In the school-aged group, the Mann Whitney U Test compared testosterone and Non-T groups on the PLS. Statistical analysis using the Kruskal-Wallis one-way analysis of variance was conducted to understand differences between Non-T, EHT, and EHT & Booster groups in school-aged children on the EOWPVT and the ROWPVT.
3 RESULTS
3.1 Demographics
Seventy-nine (92.94%) participants received a postnatal diagnosis of 49,XXXXY, with only six participants diagnosed prenatally. The majority of patients were products of a full term pregnancy. Eight subjects (9.41%) were born preterm and all less than 35 weeks gestation. The demographics of the study population is presented in Table 1. Based upon parental report, 97.78% of boys with 49,XXXXY exhibited feeding difficulties (Table 2).
| Participant characteristics | n | Mean | Median | Range |
|---|---|---|---|---|
| Age at first evaluation (months) | 85 | 48.76 | 43 | 3–129 (10 years) |
| Birth weight (kg) | 81 | 2.53 | 2.55 | 1.4–3.71 |
| Participant demographicsa | n | Mean | Median | Range |
| Maternal age (years) | 75 | 30.66 | 31 | 20–38.5 |
| Paternal age (years) | 73 | 32.92 | 33 | 21–46 |
| Ethnicity | 71 | Percent of total population | ||
| Caucasian | 55 | 77.46 | ||
| Hispanic | 3 | 4.23 | ||
| African American | 4 | 5.63 | ||
| Other | 9 | 12.68 | ||
| Delivery method | 54 | |||
| Cesarean | 30 | 55.56 | ||
| Vaginal | 24 | 44.44 | ||
- a No significant differences exist in participant characteristics between groups.
| Participant milestones | n | Mean | SD | Range |
|---|---|---|---|---|
| Smiled (months) | 42 | 2.89 | 1.76 | 0.5–8 |
| First word (months) | 46 | 19.63 | 12.9 | 5–78 |
| Two-word combinations (months) | 35 | 37.09 | 20.34 | 12–102 |
| Domain | Present | n | Percentage | |
| Feeding difficulties | 44 | 45 | 97.78 |
- Note: Milestones are based upon parental report.
3.2 Clinical assessment
3.2.1 Preschool
On the language domain of the BSID-III, statistically significant differences were documented between the EHT group (M = 83.7) and the Non-T group (M = 68.3) (U = 15, p = .0465) (Table 3). While all boys in the Non-T group on the BSID-III had standard scores that were below average or mildly impaired, 37.5% of the EHT group fell within normal limits (Figure 1).
| No testosterone | Testosterone | ||||||
|---|---|---|---|---|---|---|---|
| Assessment | n | Median | Range | n | Median | Range | p value |
| Bayley language | 4 | 69 | 56–79 | 16 | 81 | 65–112 | 0.047* |
| ELM | |||||||
| Expressive | 7 | 69 | 69–87 | 21 | 81 | 69–106 | 0.131 |
| Receptive | 7 | 87 | 69–96 | 21 | 94 | 69–131 | 0.183 |
| EOWPVT | 8 | 60.5 | 55–64 | 13 | 70 | 55–103 | 0.008* |
| ROWPVT | 9 | 77 | 59–102 | 22 | 79 | 59–103 | 1.000 |
| PLS | |||||||
| Auditory comprehension | 10 | 81.5 | 50–102 | 31 | 84 | 67–127 | 0.810 |
| Expressive communication | 9 | 71 | 50–87 | 31 | 69 | 50–106 | 0.535 |
- * Significant differences between groups at p < .05.
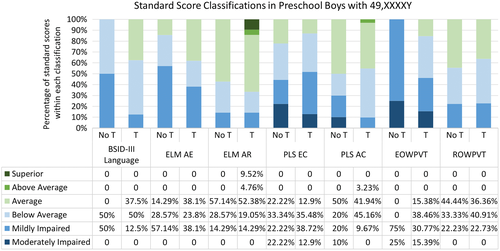
On the EOWPVT, the EHT group (n = 13) had significantly higher standard scores than the non-T group (U = 15.5, p = .008) (Table 3). All boys in the non-T group were mildly or moderately impaired on the EOWPVT, while the EHT group had scores that ranged from average to moderately impaired. The non-T group demonstrated significantly depressed scores on the EOWPVT (M = 59.6) in comparison to scores on the ROWPVT (M = 80.7) (U = 5.5, p = .003) (Table 3). In the EHT group, scores on the EOWPVT (M = 72.1) and ROWPVT (M = 80.2) were higher than the untreated group of boys with 49,XXXXY. Additionally, the boys in the treated group had no significant discrepancy between expressive and receptive vocabulary assessments. No significant differences were found between groups on the ELM or PLS. On the receptive task on the ELM, 52.38% of the EHT group had standard scores within normal limits and 9.52% had superior scores (Figure 1).
3.2.2 School-aged
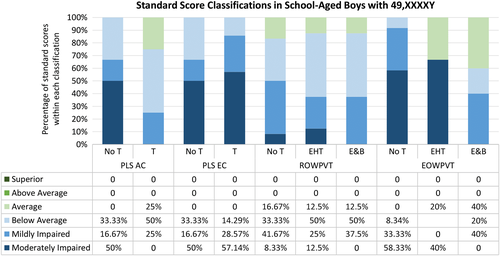
Twelve school-aged participants without testosterone treatment completed the EOWPVT and 14 completed the ROWPVT. Non-T boys had significantly higher scores on the ROWPVT (M = 70.1) in comparison to scores on the EOWPVT (M = 59.4) (U = 15, p = .005) (Table 4). In both the EHT and EHT & Booster groups, mean scores on EOWPVT and ROWPVT were within normal limits and no significant discrepancies were seen between the two domains (Table 4). On the EOWPVT, 20% of the EHT group and 40% of the E&B group had standard scores within normal limits (Figure 2). While none of the boys in either group had standard scores within normal limits on the expressive communication subtest of the PLS, 25% of the EHT group had average scores on the auditory comprehensive subtest.
| Assessment | No testosterone | EHT | EHT and booster | ||||||
|---|---|---|---|---|---|---|---|---|---|
| n | Median | Range | n | Median | Range | n | Median | Range | |
| EOWPVT | 12 | 55 | 55–72 | 5 | 70 | 55–88 | 5 | 62 | 59–90 |
| ROWVPT | 12 | 70.5 | 55–89 | 8 | 76 | 55–85 | 8 | 74 | 59–90 |
| PLS | n | Median | Range | n | Median | Range | p valuea | ||
| Auditory comprehension | 6 | 57 | 50–73 | 8 | 63.5 | 50–97 | 0.562 | ||
| Expressive communication | 6 | 51 | 50–73 | 7 | 50 | 50–72 | 0.889 | ||
- a No significant differences between groups.
3.3 Speech diagnosis evaluation
Of the 61 boys who completed a speech diagnosis evaluation, 56 (91.8%) presented with Childhood Apraxia of Speech (CAS) according to the SPLs' clinical judgment when following ASHA and Mayo criteria. Additionally, 17 of 21 boys evaluated (80.95%) presented with flaccid dysarthria at the time of evaluation.
3.4 Oral motor evaluations
3.4.1 Preschool
Multiple oral motor planning skills were deficient in the preschool group. Approximately 56% of participants could not produce raspberry sounds, and 60% were unable to elevate their tongues (Table 5). In addition, 67% of participants were unable to puff their cheeks, and 44.4% could not blow out candles. Over 80% of participants presented with decreased phoneme production. Seventy-five percent of boys indicated increased omissions and substitutions in their existing speech sounds.
| Abilities absent | Under 5 years | 5–11 years | ||||
|---|---|---|---|---|---|---|
| n | Absent | Percent | n | Absent | Percent | |
| Cough | 8 | 4 | 50 | 6 | 0 | 0 |
| Produces raspberries | 9 | 5 | 55.6 | 5 | 1 | 20 |
| Protrudes tongue | 10 | 4 | 40 | 7 | 1 | 14.29 |
| Wiggles tongue | 10 | 4 | 40 | 5 | 1 | 20 |
| Lateralizes tongue | 12 | 5 | 41.7 | 7 | 2 | 28.57 |
| Elevates tongue | 10 | 6 | 60 | 7 | 0 | 0 |
| Groping movement of tongue | 10 | 3 | 30 | 8 | 3 | 37.5 |
| Puffs cheeks | 9 | 7 | 67 | 6 | 4 | 66.67 |
| Blows out candle | 9 | 4 | 44.4 | 5 | 1 | 20 |
| Transition of syllables | 11 | 5 | 45.5 | 12 | 2 | 16.7 |
| Difficulties present | n | Present | Percent | N | Present | Percent |
| Decreased phonemes | 13 | 11 | 84.62 | 12 | 9 | 75 |
| Omissions and substitutions | 8 | 6 | 75 | 11 | 9 | 81.82 |
3.4.2 School-aged
Eighty percent of school-aged boys produced raspberries in imitation (Table 5). Over half of the boys were unable to perform refined imitative movements of their tongue resulting in groping movements of the tongue, and two-thirds could not puff their cheeks. Seventy-five percent of boys presented with decreased phonemes and 86.7% exhibited omissions and substitutions upon speech evaluation.
4 DISCUSSION
This is the largest investigation to date of the speech and language profiles of a well characterized cohort of boys with 49,XXXXY. This study demonstrates the variability of the phenotype in speech and language development from infancy through adolescence as well as provides further support to the potential benefits of early testosterone treatment on language skills in boys with 49,XXXXY. In addition, there were several novel findings associated with this comprehensive study, including documenting the presence of Childhood Apraxia of Speech (CAS) and flaccid dysarthria.
CAS is often associated with oral movement dysfunction characterized by limited sound production, difficulty imitating simple oral motor movements, and reduced phoneme production (Davis et al., 1998; Shriberg et al., 1997; Strand et al., 2003). In our investigation, only 44.4% of preschool-aged boys with 49,XXXXY imitated raspberry sounds, 33% were able to puff their cheeks, and 40% were able to elevate their tongue, further indicating oral motor weakness and reduced strength in the oral facial musculature. In older boys with 49,XXXXY there was persistent oral motor dysfunction, as well as deficits in phoneme production, omissions, and substitutions of speech sounds.
The diagnosis of CAS was indicated in 92.1% of this cohort, which is increased in comparison to the general population (0.1–0.2%) (Shriberg et al., 1997). CAS was diagnosed based on the current ASHA and Mayo criteria guidelines for the disorder due to there being no standardized assessment that can diagnose CAS. Thus, diagnosis was made by trained SLPs' judgment, consistent with how clinical diagnoses are made in the field at present. This lack of standardized assessment is a limitation of this research and is an area that requires further research in this population and others. In addition, this study does not report on all of the specific characteristics of CAS noted in subjects in this study and further efforts are underway to collect this data in order to better understand which specific speech characteristics are most impacted in boys with 49,XXXXY.
The increased incidence of CAS, as evidenced by consistent and impactful oral motor planning deficits, severe speech deficiencies, and inconsistent speech sounds, provides an explanation for the severe expressive language deficits associated with 49,XXXXY that have been described for more than 50 years (Borghgraef, Fryns, Smeets, Marien, & Berghe, 1988; Gropman et al., 2010; Burgemeister et al., 2019).
In addition, our cohort exhibited significant discrepancies between expressive and receptive language skills, which support previous findings of this profile in boys with males with 49,XXXXY (Burgemeister et al., 2019; Galasso et al., 2003; Lomelino & Reiss, 1991). Untreated preschool and school-aged boys demonstrated higher scores in receptive language when compared to their expressive language skills. However, in both expressive and receptive language, participants who received testosterone exhibited increased scores when compared to their untreated counterparts.
Recent research publications have documented the impact of testosterone replacement therapy on the neurodevelopmental profile of boys diagnosed with 49,XXXXY, including language development (Linden et al., 1995; Mazzilli et al., 2016; Samango-Sprouse et al., 2011). Early hormonal treatment had a positive impact on boys with 49,XXXXY, demonstrated by significantly increased expressive language development as infants and toddlers. Our study results also demonstrate that testosterone-treated populations of preschool and school-aged boys had more normalized profiles in language, with more commensurate scores in expressive and receptive language skills. In both expressive and receptive language, participants who received testosterone exhibited increased scores when compared to their untreated counterparts. In addition, treated boys with 49,XXXXY demonstrated wider variability, with scores from moderately impaired to superior, while untreated boys only ranged from moderately impaired to within normal limits. These findings provide additional evidence to the positive impact of hormonal replacement therapy on the language deficits observed in boys with X and Y chromosomal abnormalities.
Our results provide further evidence to the phenotypic profile of the boy with 49,XXXXY with the increased incidence of expressive and receptive language discrepancies from infancy to early childhood in males with 49,XXXXY, particularly in the untreated population. In addition, this investigation documents that Childhood Apraxia of Speech (CAS) and associated oral motor planning deficits are pervasive in boys with 49,XXXXY and serves as an explanation for the speech and language discrepancies and deficiencies reported in this population. Future research is needed to formally collect speech characteristic data such as fluency, intelligibility, and articulation in this disorder in addition to analyzing the possible impact of testosterone treatment on these capabilities. With no standardized assessment for CAS, evaluating the possible impact of testosterone on the presence of CAS in a population may not be possible at this time. However, further research could evaluate the incidences of specific speech deficits characteristic of CAS in both untreated and treated populations in an effort to determine whether testosterone treatment has an impact on these characteristics.
The variability and complexity of the speech and language profile presented in this study, as well as the impact of biological treatment, indicate the importance of consistent and comprehensive assessment from infancy or time of diagnosis in order to support neurodevelopmental needs and achieve optimal outcomes in males with 49,XXXXY.
ACKNOWLEDGEMENTS
We would like to express our deep gratitude to all our participants and their families. We would like to thank the Focus Foundation for their continued funding of our investigative studies.
CONFLICT OF INTEREST
None declared.
Open Research
DATA AVAILABILITY STATEMENT
The data that support the findings of this study are available from the corresponding author upon reasonable request.