A comparison of the functional health of children with Costello syndrome in 1999 and in 2015
Abstract
Costello Syndrome is a rare congenital condition characterized by failure-to-thrive, cardiac abnormalities, distinctive facial features, predisposition to malignant tumors, and developmental delay. In 1999, we analyzed the functional health in a cohort of 18 patients. Since then, a mutation in the HRAS gene has been found to be causative, medical management has been refined, and the level of awareness has increased. The purpose of this study is to compare the functional health outcomes from the 1999 cohort with data prospectively collected from a comparable cohort in 2015. The Pediatric Outcome Data Collection Instrument (PODCI) was administered to parents of children with Costello syndrome during the 2015 International Costello Syndrome Conference. The same instrument and setting were used in the 1999 study. We compared functional health scores from the two groups. A total of 21 participants were included in the 2015 cohort; 15 females (71%) and 6 males (29%). Average age was 5.8 years (range 2–16). When comparing functional health outcomes, we found that the 2015 cohort scored slightly higher in Upper Extremity and Physical Function (57 vs. 54) and Comfort scales (86 vs. 82). However, there was no significant difference in any of the PODCI scales between the two groups. When compared with normative scores, both groups scored significantly lower in every scale except for happiness (p = 0.2952). Despite recent advancements, functional health outcomes in 2015 were similar to those measured in a different cohort in 1999.
1 INTRODUCTION
Costello syndrome (CS) is a multisystem disorder characterized by failure to thrive in infancy, intellectual impairment, characteristic coarse facial features with full lips and a large mouth, curly sparse hair, structural and functional heart abnormalities, a predisposition to malignant tumors, short stature, and an array of musculoskeletal anomalies that adversely affect functional performance (Gripp & Lin, 2012a; Kerr, Gripp, & Lin, 2010).
CS is an autosomal dominant disorder caused by a germ line missense mutation in the HRAS gene; the only gene known to be associated with Costello Syndrome. This gene encodes for proteins in the RAS/mitogen activated protein kinase (MAPK) pathway. Other syndromes also caused by germ-line mutations that alter the RAS/MAPK pathway (and collectively known as RASopathies), include Cardiofaciocutaneous Syndrome (CFCS) and Noonan Syndrome, both of which have overlapping clinical features with CS (Aoki et al., 2005; Gripp et al., 2006; Zampino et al., 2007).
HRAS gene mutations that results in overproduction of HRAS proteins create an increased risk of benign and malignant tumors. Benign facial and peri-anal papillomas and malignant rhabdomyosarcoma are reported in children with CS and transitional cell carcinoma in CS adults. (Gripp, 2005; Kratz, Rapisuwon, Reed, Hasle, & Rosenberg, 2011).
Since its first description in 1971, the syndrome has been increasingly recognized with approximately 200–300 individuals reported worldwide. (Genetics Home Reference, 2012; Gripp & Lin, 2012b). Musculoskeletal manifestations are frequent and include a curious combination of hypotonia and ligamentous laxity along with upper and lower extremity joint contractures. In addition, ulnar deviations of wrists and fingers, congenital vertical talus, spine deformities (kyphosis, scoliosis), positional foot deformity with progressive tightness of the Achilles tendon, and decreased bone mineral density have been noted.(Gripp et al., 2006; Leoni, Stevenson, & Martini, 2014; Reinker, Stevenson, & Tsung, 2011; Yassir, Grottkau, & Goldberg, 2003).
The functional health of children with CS has been incompletely studied. All children are ambulatory. In 1999, we analyzed the orthopaedic manifestations and functional health of patients with CS and found their functional health to be significantly lower than the normative population. (Yassir et al., 2003). In 2015, Johnson et al. (2015) compared the physical function of patients with CS with those with CFCS and found that both conditions have similar functional limitations and severity of disability. With discovery of the causative gene, with increased awareness of the syndrome, and with medical management refined we sought to reassess the functional health of a group of children with CS and compare these outcomes with those of 1999. We hypothesize that children with CS now have better functional health than 16 years previously.
2 METHODS
After obtaining IRB approval, we participated in the 2015 International Costello Syndrome Conference in Seattle, WA. We prospectively administered the Pediatric Outcome Data Collection Instrument (PODCI) (Daltroy, Liang, Fossel, & Goldberg, 1998) to parents of all children participating in the study. The Pediatric PODCI is a parent reported questionnaire designed to assess pediatric patients overall health, pain, and ability to participate in normal daily activities, as well as in more vigorous activities associated with young people. It measures six domains: upper extremity and physical function, transfer and basic mobility, sports and physical functioning, pain/comfort, happiness and global functioning. The same instrument and same setting were used in the 1999 study. We also collected demographic data and whether children had surgeries, tumors, or were undergoing growth hormone therapy. We compared functional health scores from the two cohorts using a Wilcoxon rank–sum test. Differences between PODCI scores and normative values (Hunsaker, Cioffi, Amadio, Wright, & Caughlin, 2002) were evaluated with a one-sample t-test. Statistical significance was set at p ≤ 0.05 and all confidence intervals at 95%.
3 RESULTS
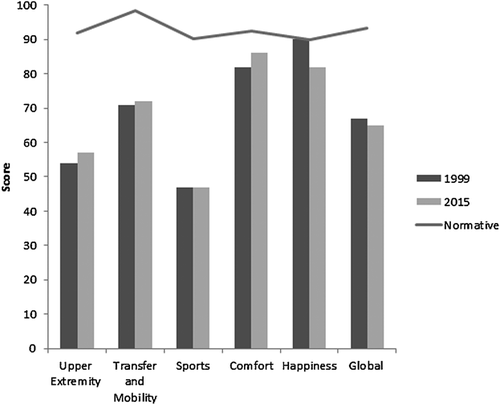
A total of 21 participants were included in the 2015 cohort; 15 females (71%) and 6 males (29%). Average age was 5.8 years (range 2–16). Twenty patients (95%) had surgery in their lifetime, with an average of four surgeries per patient. The most common types of surgeries were G-tube placement, tonsillectomy, and adenoidectomy. None of the patients reported tumors and 3 (15%) were undergoing growth hormone therapy. In the 1999 cohort, 18 children were included in the study; 9 males (50%) and 9 females (50%). Average age was 8.3 (range 3–23). The groups were not statistically different in age (p = 7947). The average PODCI scores for the 2015 cohort were slightly higher in Upper Extremity and Physical Function (57 vs. 54; p = 0.7915) and Comfort (86 vs. 82; p = 0.7440). However, the 2015 cohort scored slightly lower in Transfer and Mobility (71 vs. 72; p = 0.6919); Happiness (82 vs. 90; p = 0.2208) and Global functioning (65 vs. 67; p = 0.6477). Average scores were the same for the Sports domain (47; p = 0.8853). We found no significant difference in any of the PODCI subscales between the two groups. (Table 1) When compared with normative scores, both groups scored significantly lower in every scale except for happiness (p = 0.2952) (Figure 1).
| Upper extremity mean (SD) | Transfer and mobility mean (SD) | Sports and physical function mean (SD) | Pain mean (SD) | Happiness mean (SD) | Global mean (SD) | |
|---|---|---|---|---|---|---|
| 1999 | 54.27 (25.06) | 71.70 (25.34) | 46.82 (20.47) | 82.35 (24.2) | 90.25 (15.46) | 67.13 (16.59) |
| 2015 | 57.06 (16.85) | 71.47 (20.85) | 46.62 (18.05) | 85.61 (18.69) | 81.92 (20.06) | 64.87 (15.58) |
4 DISCUSSION
In the 16 years between our two studies, the gene responsible for Costello Syndrome has been identified; the diverse, multisystem clinical manifestations delineated; and anticipatory care and health management recommendations made. (Axelrad, Schwartz, Katzenstein, Hopkins, & Gripp, 2011; Gomez-Ospina et al., 2016; Gripp et al., 2006; Gripp & Lin, 2012a,2012b; Kratz et al., 2011; Lin et al., 2011; Rauen, 2007; Yassir et al., 2003) With this in mind, we hypothesized that children with CS would have better functional health than they had 16 years ago. Our study indicates that despite recent advancements, parents do not report an improvement in their children's overall functional health. In 2015, Johnson et al. (2015) compared the functional heath of children with CS and CFCS and found that both groups have similar levels of disability. The functional health of children with CS has been measured with the same instrument in 1999, 2013, and 2015 and the three studies yielded consistent results. Upper extremity function, transfer and mobility, sports, and global function are the most compromised compared to the normative population. Hand and wrist deformity, ligamentous laxity, and restricted elbow motion, might explain their upper extremity impairments, while lower extremity contractures, rigid foot deformities, and spine deformity might account for their limitations in basic mobility and sports. In all three cohorts parents have reported high comfort scores (i.e., little pain), with average scores close to normative values. Happiness scores remain consistently high which may represent the often engaging personality of children with CS. Nonetheless, persistence of overall poor musculoskeletal function suggests that progress has not been made to improve performance, an outcome that is important to patients and families.
There are several limitations in this study. We compared children with CS from two different cohorts; one before the identification of the gene mutation and the institution of an array of screening protocols and clinical interventions; and the other after. Even though our cohorts were comparable in age and size, we recognize that a longitudinal analysis of the same children may have yielded additional results. Further, we did not collect data on the number of surgeries and whether patients had tumors in the 1999 cohort and therefore, we do not know whether children are now undergoing more surgical procedures or not. Finally, the small sample size does not allow for stratification by age, sex, or intervention. It can be argued that the small sample size prevented us from finding a significant difference between the cohorts. However, sample size is a challenge in the study of all rare diseases. The purpose of this study was to assess functional performance of a population, of children teens, and young adults with Costello syndrome as perceived by their parent. We performed neither a detailed physical examination nor a thorough medical record review, and thus did not collect data that would allow us to compare severity of musculoskeletal manifestations in individual children, nor the effectiveness of the interventions prescribed.
When a child presents with an array of developmental and structural abnormalities, the naming of a syndrome and identification of the mutated genetic pathway may raise false expectations that the cure is not far behind. If not a cure, certainly improvement in function, which on a day to day basis is what families are seeking. Enhancing performance through participation and assistive technology should be a research priority.
In summary, substantial advances have been made in understanding the HRAS gene pathway, the clinical manifestations, and suggested management of Costello syndrome. Nonetheless, functional health and performance of those with CS, as measured by a validated parental questionnaire, has not improved in the 16 years since our original study.
ACKNOWLEDGMENTS
The authors would like to thank the families who participated in the study and the Costello Syndrome Family Network for its support in this project.
CONFLICTS OF INTEREST
The authors have indicated they have no financial relationships or conflict of interests relevant to this article to disclose.