Cognitive, adaptive, and behavioral features in Joubert syndrome
Abstract
Joubert syndrome (JS) is a recessive neurodevelopmental disorder characterized by a distinctive cerebellar and brainstem malformation recognizable on brain imaging, the so-called molar tooth sign. The full spectrum of cognitive and behavioral phenotypes typical of JS is still far from being elucidated. The aim of this multicentric study was to define the clinical phenotype and neurobehavioral features of a large cohort of subjects with a neuroradiologically confirmed diagnosis of JS. Fifty-four patients aged 10 months to 29 years were enrolled. Each patient underwent a neurological evaluation as well as psychiatric and neuropsychological assessments. Global cognitive functioning was remarkably variable with Full IQ/General Quotient ranging from 32 to 129. Communication skills appeared relatively preserved with respect to both Daily Living and Socialization abilities. The motor domain was the area of greatest vulnerability, with a negative impact on personal care, social, and academic skills. Most children did not show maladaptive behaviors consistent with a psychiatric diagnosis but approximately 40% of them presented emotional and behavioral problems. We conclude that intellectual disability remains a hallmark but cannot be considered a mandatory diagnostic criterion of JS. Despite the high variability in the phenotypic spectrum and the extent of multiorgan involvement, nearly one quarter of JS patients had a favorable long-term outcome with borderline cognitive deficit or even normal cognition. Most of JS population also showed relatively preserved communication skills and overall discrete behavioral functioning in everyday life, independently from the presence and/or level of intellectual disability. © 2016 Wiley Periodicals, Inc.
INTRODUCTION
Joubert syndrome (JS) is a congenital non-progressive cerebellar ataxia with autosomal recessive or X-linked inheritance, whose diagnostic hallmark is a distinctive cerebellar and brainstem malformation recognizable on brain imaging, the so-called molar tooth sign [Romani et al., 2013]. This complex defect is characterized by variable degree of cerebellar vermian hypodysplasia of, associated to a deepened interpeduncular fossa and thickened, elongated, and mal-oriented superior cerebellar peduncles, appearing as a “molar tooth” on axial brain MRI sections [Maria et al., 1997]. The absence of decussation of the superior cerebellar peduncles as well as the corticospinal tract at the medullary pyramids are other typical findings.
JS is characterized by marked clinical and genetic heterogeneity. The core neurological phenotype presents hypotonia, ataxia, developmental delay often associated with intellectual disability, altered respiratory pattern during the neonatal period, abnormal ocular movements, and distinctive facial features. These neurological signs can be associated to variable multiorgan involvement, mainly of the retina, kidney, liver, and skeleton. About thirty JS-associated genes have been identified until now [Bachmann-Gagescu et al., 2015]. Interestingly, all genes encode for proteins of the primary cilium, making JS part of the expanding family of ciliopathies, a group of heterogeneous conditions sharing both clinical features and genetic determinants [Romani et al., 2013].
Mild to severe intellectual disability is common in patients with JS. Borderline [Steinlin et al., 1997; Fennell et al., 1999; Tavano and Borgatti, 2010] or even normal cognitive functioning [Gunay-Aygun et al., 2009; Poretti et al., 2009; Romani et al., 2014] in subjects with JS are exceptions. Discordant cognitive development has also been reported between affected sibilings [Steinlin et al., 1997; Poretti et al., 2009], giving further confirmation of the complexity in predicting outcome in infants.
Steinlin et al. [1997] provided the first long-term study of 19 children with JS and reported three different developmental courses and outcomes: three infants died before the age of 3, nine had a mild developmental delay with quotients ranging from 60 to 85, while four had a developmental quotient of 30 or less and severe visual and motor problems.
Fennell et al. [1999] reported a variety of deficits in cognition, verbal memory, visuomotor integration, fine motor control, and language-related tasks in 10 assessable children. Parents’ reports revealed temperament, hyperactivity, aggressiveness, and dependence problems, as well as impairments in physical development and personal care. Only three out of 40 were functioning within the borderline range, the rest falling in the severely impaired one.
Tavano and Borgatti [2010] compared the neurocognitive and emotional profiles of four JS subjects with those of seven patients with other malformations of the cerebellar vermis with or without involvement of the hemispheres. Neuropsychological assessment indicated that this latter group had significantly atypical emotional skills and executive functioning compared to patients with JS, while the opposite was found for verbal memory and expressive language, thus confirming the presence of a selective difficulty in the use of communicative language in JS.
To our knowledge, no study has yet adopted standardized instruments to assess intelligence, adaptive functioning, and behavior in a large cohort of children, adolescents, and young adults with JS. Our prospective, multi-center trial thus aims to deepen our knowledge of the syndrome's cognitive and neurobehavioral phenotype, to facilitate more focused epidemiologic and therapeutic-oriented research and to improve patients’ management and rehabilitation.
METHODS
Participants
Fifty-four patients (35 males, 19 females; age range: 10 months to 29 years; median age: 8 y 5 m; mean age: 9 y 11 m; standard deviation: 6 y 6 m) including one pair of twins, four pairs and one trio of siblings, were selected between 2007 and 2010 by Italian Scientific Institutes and Universities specialized in diagnosis and management of subjects with JS. Table I shows maternal education and parental job according to the coding system of Italy's National Statistics Institute for all subjects [ISTAT, 1991].
| N | % | |
|---|---|---|
| Male | 35 | 64.8 |
| Multiorgan involvement | ||
| Retinal dystrophy | 22 | 40.7 |
| Coloboma | 7 | 12.9 |
| Renal disease | 9 | 16.7 |
| Liver fibrosis | 4 | 7.4 |
| Polydactyly (hands or feet) | 10 | 18.5 |
| Maternal education | ||
| Primary school | 2 | 4.3 |
| Secondary school | 14 | 29.8 |
| High school | 20 | 42.5 |
| University | 11 | 23.4 |
| Parental job | ||
| Labourers | 8 | 17 |
| Employees | 15 | 32 |
| Managers | 4 | 8.5 |
| Businessmen/freelance professionals | 6 | 25.5 |
| Self-employed | 12 | 12.8 |
| Teachers | 1 | 2.1 |
| Unemployed | 1 | 2.1 |
MRIs were reviewed by neuroradiologists experts in cerebellar malformations, including members of the Italian Joubert syndrome group, and the “molar tooth sign” was confirmed in all subjects. A pathognomonic combination of imaging findings on axial MRI was found in all patients, that is, cerebellar vermis hypoplasia, thickened and horizontally oriented superiori cerebellar peduncles, and a deep interpeduncular fossa (the molar tooth sign) [Poretti et al., 2014]. Other CNS anomalies were present in two subjects (one corpus callosum abnormality and one polymicrogyria).
Further clinical and instrumental details were obtained through the referring clinicians using a standardized questionnaire, that allowed classifying patients into six clinical subgroups [Romani et al., 2013]: pure JS (n = 20), JS plus retinal disease (n = 18), JS plus renal disease (n = 5), JS plus retinal and renal disease (n = 1), JS plus liver disease (n = 5), and oro-facio-digital syndrome type VI (n = 5). The developmental data and clinical signs are outlined in Supplementary Table SI.
Organ involvement was assessed by clinical examinations and instrumental testing as appropriate, including inspection of fundus oculi, visual evoked potentials, electroretinogram, abdominal ultrasound, routine renal parameters, urinary specific gravity, urinary concentration test after desmopressin stimulation, and liver biopsy. All patients underwent next generation sequencing-based target resequencing of the 26 JS causative genes known at the time of the experiment (as part of a panel of 120 ciliary genes) on a Solid 5500xL platform. Thirty-two patients were found to carry homozygous or compound heterozygous pathogenic mutations in the following genes: TMEM67 (9), CC2D2A (4), INPP5E (4), AHI1 (4), RPGRIP1L (2), NPHP1 (1), CEP290 (2), KIAA0586 (1), TMEM237 (1), TMEM216 (2), TMEM17 (2). In 23 patients, biallelic pathogenic mutations could not be detected in any of the tested genes. Nine of them were found to carry a single heterozygous mutation in a JS-causative gene (CEP41, C5Orf42, KIAA0586, CC2D2A, INPP5E, NPHP1, TCTN1, ARL13B) whose significance remains to be established.
Developmental/Neurological and Neuropsychological, Adaptive, and Behavioral Assessment
- developmental and neurological evaluation in order to define prominent neurological signs (hypotonia, ataxia, dysarthria, eye movement abnormalities, etc.); the main developmental milestones, in particular neuromotor and linguistic ones, were obtained by means of a thorough review of the clinical records of each patient;
-
intelligence evaluation using standardized tests, according to age and to clinical conditions:
-
Wechsler intelligence scales in different age versions [Wechsler, 1993, 1996, 1997]: verbal, performance and full IQ, verbal and performances sub-tests standardized scores were calculated;
- visualization and reasoning battery of the Leiter International performance scale-revised (Leiter-R) [Roid and Miller, 1997] for patients between 2 and 21 years old with significant attention and communication difficulties. We decided to use the brief IQ which is calculated by administering the following subtests: figure ground, form completion, sequential order, and repeated patterns;
- Griffiths mental developmental scales [Griffiths, 1996, 2006] for children under 5 years old or with severe developmental delay. The test is composed of five sub-scales (locomotor, personal-social, language, eye–hand coordination, and performance) and its raw scores can be converted to subQs, which allows to calculate the general quotient (GQ);
-
-
behavioral evaluation using the child behavior check list (CBCL) version 1.5-5 [Achenbach, 2000] and 4-18 [Achenbach, 1991]. The preschool form is made up of seven syndrome scales (emotionally reactive, anxious/depressed, somatic complaints, withdrawn, attention problems, aggressive behavior, and sleep problems), while the CBCL 4-18 is made up of eight syndrome scales (anxious/depressed, depressed, somatic complaints, social problems, thought problems, attention problems, rule-breaking behavior, and aggressive behavior). These syndrome scales are clustered into two higher order factors, that is, internalizing and externalizing, and a total CBCL score.
A standard clinical psychiatric assessment was carried out and, if necessary, the criteria of the DSM-V were used to formulate a diagnosis of psychiatric disorder;
- adaptive functioning by means of the expanded form of the Vineland adaptive behavior scales (VABS) [Sparrow et al., 1984; Balboni and Pedrabissi, 2004] through a semi-structured interview with the caregiver. Adaptive behavior is grouped into four broad domains, that is, communication, daily living skills, socialization, and motor skills. The adaptive behavior composite (ABC) was calculated as the sum of communication (133 items); daily living skills (201 items); socialization (134 items). The 72 items of motor skills evaluate gross and fine motor skills up to 6 years of developmental age.
Statistical Analysis
SPSS 10.0 for Windows was used to analyze all data.
The Wechsler intelligence scales, the Leiter or Griffiths mental development scales were used to determine the intelligence quotient (IQ) or general quotient (GQ) scores. Raw scores in adaptive scales were converted to age-equivalent scores and then to ratio Quotient (rQ) scores, so that performances on different tests in the same subjects and between groups of subjects could be compared. The rQs were calculated by averaging the equivalent ages on all subtests to obtain mental age, then dividing it by chronological age and multiplying it by 100.
All statistical tests were two-tailed and P-values of 0.05 or lower were considered significant.
A repeated measures ANOVA was used to analyze the intelligence/developmental scales, the CBCL, and the VABS to detect significant difference among the means. Bonferroni corrected post hoc tests were performed to discover which specific means significantly differed between pairs of tests.
The t-test was used to compare the scores of two groups (independent sample) or two performances within the same sample (paired sample).
Pearson correlation test was performed to analyze the relationship between cognitive and behavioral scores, as well as between the cognitive-behavioral scores and chronological or equivalent age.
RESULTS
Developmental and Clinical Features
A global developmental delay was found in 44 (81%) patients. This is a condition of significant delay in developmental milestones at expected ages in two or more of the following domains: gross/fine motor, speech/language, cognition, social/personal, and daily life activities in children younger than 5 years old [Shevell et al., 2003].
Thirty-six (about 66%) subjects learned to walk independently well-enough to get around outside their home, but all developed ataxia with a broad-based, unsteady gait, and had difficulties in running or climbing stairs. Acquisition of independent walking was delayed from 15 months to 9 years (Mdn: 24 months). At testing, eight subjects did not walk independently (three were still younger than 2 years old), three were only able to take a few steps autonomously, five walked with caregivers’ support (three have a severe visual deficit), and two required assistive equipment for mobility (walker and wheel chairs, respectively). Forty-five subjects were verbal. The first words of the verbal subjects were uttered between 10 months and 10 years (Mdn: 24 months), and seven had not yet achieved the ability to associate words (two were younger than 3 years old). Word association was achieved between 15 months and 7 years 4 months (Mdn: 36 months) in 25 patients. Further information is displayed in Supplementary Table SII.
Although variable in severity, dysarthria was found in 40 of the 45 verbal subjects; only five subjects showed good speech articulation.
Additional neurological signs were hypotonia (42.6%), ataxia (87%), and eye movement abnormalities, including nystagmus, strabismus, and ocular motor apraxia (74%). Seizures were rarely noted (3.7%). Altered respiratory patterns characterised by short alternate episodes of apnoea and tachypnoea or episodic tachypnoea alone were found in 31.5%.
Associated clinical features included ocular signs (retinal dystrophy 40.7%; colobomas 13.0%), renal signs (kidney dysplasia 7.4%; nephronophthisis 11.1%), liver signs (liver fibrosis 7.4%; high transaminases 12.9%). Facial dysmorphisms, including prominent forehead, ptosis, prognathia, arched eyebrows, lower lip eversion with trapezoid-shaped mouth, and tongue protrusion were noted in 68.5% and polydactyly (hands or feet) in 18.5%. Table I summarizes the occurrence of multiorgan involvement, and Supplementary Table SI shows clinical data for each subject.
Cognitive, Adaptive, and Behavioral Results
Intelligence
Cognitive functioning was assessed in 49 subjects using formal instruments. Full IQ or GQ ranged from 15 to 129 (mean 58 SD 26). Six (11%) patients had normal, three (6%) below average, and six (11%) borderline intellectual functioning; the remaining had intellectual disability, that is, 8 (15%) mild, 12 (22%) moderate, and 14 (26%) severe. Five patients (9.3%) were so profoundly impaired that only an assessment of adaptive functioning and/or questionnaires on behavior could be carried out. The Wechsler scales were administered to 28 subjects, the Leiter-R was used in 13 patients with severe delay or language/speech disorders; and the Griffiths Mental Development Scales were used in eight subjects with chronological or mental age below 4 years old.
Table II summarizes the sample mean score of the intellectual and developmental scales. The Supplementary Table SII outlines Full IQ or GQ and the instrument used for each patient.
| N | Mean | SD | Range | ||
|---|---|---|---|---|---|
| Wechsler intelligence scales | |||||
| IQs | |||||
| Full IQ | 25 | 57.84 | 20.80 | 32 | 110 |
| Performance IQ | 26 | 59.04 | 20.83 | 36 | 116 |
| Verbal IQ | 26 | 66.54 | 18.54 | 40 | 103 |
| Subtest | |||||
| Information | 27 | 5.44 | 3.63 | 1 | 13 |
| Similarities | 27 | 5.59 | 3.26 | 1 | 12 |
| Arithmetic | 27 | 3.96 | 2.92 | 1 | 12 |
| Vocabulary | 27 | 4.85 | 3.09 | 1 | 11 |
| Comprehension | 27 | 4.00 | 2.75 | 1 | 10 |
| Digit span | 21 | 5.28 | 3.01 | 1 | 12 |
| Picture completion | 27 | 5.00 | 3.77 | 1 | 15 |
| Coding | 27 | 2.76 | 1.86 | 1 | 7 |
| Picture arrangement | 23 | 3.30 | 2.57 | 1 | 8 |
| Block design | 27 | 4.37 | 3.16 | 1 | 10 |
| Object assembly | 23 | 3.17 | 2.87 | 1 | 11 |
| Leiter-R | |||||
| Brief IQ | 13 | 69.15 | 33.86 | 33 | 129 |
| Subtest | |||||
| Figure ground | 13 | 6.08 | 5.05 | 1 | 15 |
| Form completion | 13 | 6.83 | 5.51 | 1 | 18 |
| Sequential order | 13 | 5.08 | 4.36 | 1 | 13 |
| Repeated patterns | 13 | 6.08 | 4.93 | 1 | 13 |
| Griffiths mental development scales | |||||
| General quotient | 8 | 42.13 | 16.42 | 15 | 62 |
| SubQs | |||||
| A Locomotor | 8 | 38.65 | 15.33 | 21 | 65 |
| B personal-social | 8 | 48.91 | 20.25 | 16 | 76 |
| C language | 8 | 42.00 | 20.16 | 21 | 79 |
| D eye and hand co-ordination | 8 | 43.75 | 19.34 | 11 | 65 |
| E performance | 8 | 42.70 | 22.01 | 5 | 66 |
- IQ and subQs have mean = 100 and SD = 15, while subtest have mean = 10 and SD = 3.
The Full IQ could not be calculated in three cases: in the first, the raw score was below the WAIS lower limit; the second had only the Verbal IQ due to severe visual deficit (retinal dystrophy); the last had only the performance IQ due to severe dysarthria.
Regarding the Wechsler scales, full IQ ranged from 32 to 110, performance IQ from 36 to 116, and verbal IQ from 40 to 103. A repeated measures ANOVA with a Greenhouse-Geisser correction uncovered a main effect for both the Verbal (F = 5.887, P < 0.01) and performance scales (F = 3.655, P < 0.05). Post hoc tests using the Bonferroni correction revealed that verbal reasoning and concept formation (similarities) was better than arithmetic skills (P < 0.05) and social comprehension (P < 0.01). With regard to the performance subtests, the coding was only lower than the completion test (P < 0.05). The arithmetic and coding scores correlated with digit span (respectively, r = 0.588, P < 0.001 and coding: r = 0.606, P < 0.001) while the coding score was not related with the VABS’ motor rQs.
Thirteen patients were assessed using the visualization and reasoning battery of the Leiter-R and the IQ ranged from 33 to 129 (mean 69 SD 34). According to the repeated measures ANOVA with a Greenhouse-Geisser correction, the mean subtest scores did not differ significantly (F = 1.757, P = 0.202).
The range of Wechsler performance and the Leiter-R IQs partially overlapped (respectively, 36–116 and 33–129), with the mean performance Wechsler IQ, resulting slightly but not significantly lower than Leiter IQ (mean 59, standard deviation 21 vs. mean 69, standard deviation 34; independent samples t-test, t = 0.969, P = 0.346). Both Wechsler performance and the Leiter-R IQs evaluate visual-spatial abilities and visual-perceptual reasoning, and seem to confirm that non verbal functioning is relatively preserved in JS population without visual impairment.
The eight subjects assessed with the Griffiths mental development scales had a mean GQ of 42 (standard deviation 16, range 15–62). The locomotor quotient appeared relatively lower, but not significantly lower than the other subscales.
Adaptive behavior
The VABS was administered to 39 patients. The ABC and cognitive quotients were not significantly different (ABC mean 55 SD 23 and GQ/full IQ mean 55 SD 22, P = 0.966). Table III outlines the mean rQ for communication, daily living, socialization, and motor skills domains. A repeated measures ANOVA with a Greenhouse-Geisser correction uncovered a significant difference between the three rQs (F = 16.44, P < .001). Bonferroni corrected post hoc tests revealed that communication was better than daily living (P < 0.01) and socialization skills (P < 0.001).
| VABS | N | Mean | SD | Range | |
|---|---|---|---|---|---|
| Adaptive behavior compositea | 39 | 52.49 | 23.18 | 15 | 125 |
| Communication | 39 | 61.02 | 30.10 | 15 | 153 |
| Daily living | 39 | 49.42 | 23.51 | 14 | 129 |
| Socialization | 39 | 47.11 | 20.44 | 15 | 94 |
| Motor skills | 32 | 36.39 | 21.10 | 9 | 81 |
| CBCL | |||||
| Internalizing scale | 40 | 60.40 | 13.70 | 37 | 96 |
| Externalizing scale | 40 | 50.55 | 6.59 | 39 | 68 |
| Emotionally reactive | 9 | 55.89 | 6.31 | 50 | 69 |
| Anxious/depressed | 40 | 58.30 | 8.41 | 50 | 81 |
| Somatic complaints | 40 | 60.23 | 7.65 | 50 | 82 |
| Withdrawn | 40 | 58.57 | 10.11 | 50 | 82 |
| Sleep problems | 9 | 58.33 | 5.39 | 50 | 67 |
| Attention problems | 40 | 57.87 | 6.31 | 50 | 70 |
| Aggressive behavior | 40 | 52.43 | 4.17 | 50 | 68 |
| Social problems | 30 | 62.40 | 6.26 | 50 | 77 |
| Thought problems | 31 | 55.03 | 8.01 | 50 | 79 |
| Delinquent behavior | 31 | 52.61 | 3.54 | 50 | 61 |
| Intrusiveness | 1 | 73.00 | 73 | 73 | |
- The ratio IQ have mean 100 and standard deviation 15, while the T-scores have mean 50 and standard deviation 10.
- a The adaptive behavior composite score has been obtained by grouping communication, daily living skills, and socialization domains.
Consistent with what expected for subjects with cerebellar malformation, motor organization was quite impaired and characterized by inferior gross motor skills (i.e., ability to balance and to co-ordinate and control movements) compared to fine eye and hand coordination (gross motor rQ: mean 34 SD 23; fine motor rQ: mean 42 AD 19; paired t-test = −4833, P < 0.001). The VABS motor rQs were lower than the GQ/Full IQ (fine motor rQ: t = 4.458, df = 32, P < 0.001; gross motor rQ: t = 6.609, df = 29, P < 0.001, motor skills: t = 5.830, df = 30, P < 0.001).
Communication, daily living, and socialization rQs correlated significantly with GQ/Full IQ (communication: r = 0.613, P < 0.001; daily living: r = 0.561, P < 0.001; socialization: r = 0.640, P < 0.001; motor skills: r = 0.723, P < 0.001), indicating a significant, reciprocal relationship between cognitive functioning and adaptive behavior.
Behavior
Twenty-one of the 54 patients showed emotional fragility, withdrawal, inattention, irritability, poor tolerance to frustration, and oppositional behavior linked to environmental stress. Only four subjects (7,4%) showed emotional–behavioral problems consistent with a DSM psychiatric diagnosis (i.e., two oppositional defiant and two bipolar disorders). Two patients with profound, not assessable intellectual disability showed atypical behavior suggestive of an autism spectrum disorder. Supplementary Table SII shows behavioral and emotional characteristics subject by subject.
On 40 subjects, the CBCL scores revealed more internalizing than externalizing problems (paired sample t-test, t = 4.734, P < 0.001). The frequencies of clinical scores were calculated with reference to cut-offs defined by the Achenbach method, that is, the standard scores are based on the 90th percentile (z-score = 1.3) for the internalizing and externalizing areas. Fourteen subjects (35%) obtained pathological scores at the internalizing scale, while two subjects (5%) exceeded the clinical cut-off of the externalizing one. The CBCL mean T-scores are outlined by Table III. The internalizing score correlated with the Socialization rQ of the VABS (P < 0.05), while the externalizing one did not correlate with any cognitive/adaptive scales. The CBCL total problem score was negatively correlated with the level of VABS social adaptive functioning (N = 34, r = −0.390, P < 0.05).
The repeated measures ANOVA indicated a significant difference in the mean subscale scores of the 31 subjects evaluated by CBCL/4-18 (F = 14.945, P < 0.001). Bonferroni corrected post hoc tests specified that the main effect was supported by the scores at the internalizing, attentional, and social problems scales. The aggressive and delinquent behavior scales were lower than anxious/depressed (respectively, P < 0.001 and <0.01), withdrawn (P < 0.01), somatic complaints (P < 0.001), attention (P < 0.001), and social problems (P < 0.001). On the other hand, the social problems scale as well as the two externalizing scales aforementioned resulted higher than anxious/depressed (P < 0.01), withdrawn (P < 0.05), attention (P < 0.01), thought problems (P < 0.001).
Although the profile tends to be similar in the school and preschool subgroups (N = 9), repeated measures ANOVA did not show significant results in children with JS who were younger than 6 years old (F = 1.825, P = 0.114).
Correlations with age
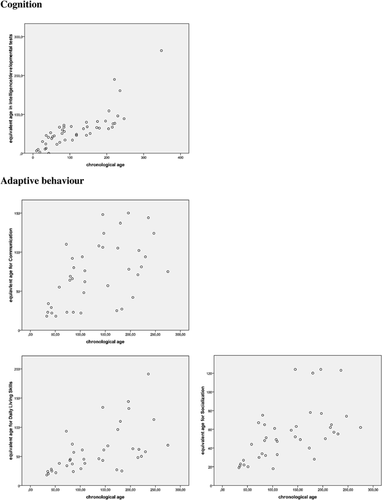
The chronological age of patients with JS correlated with the equivalent age in intelligence/developmental (r = 0.815; P < 0.001), and adaptive tests (r = 0.548, P < 0.001 for Communication; r = 0.575, P < 0.001 for daily living skills; r = 0.573, P < 0.001 for socialization).
Figure 1 shows the scatterplots of the correlation between chronological age and developmental age obtained in cognitive and adaptive scales.
DISCUSSION
To our knowledge, this is the first prospective study that evaluated a large cohort of children, adolescents, and young adults with JS using neuropsychological and behavioral standardized instruments. The main objective of this study was to investigate the JS-related cognitive and neurobehavioral phenotype.
Intelligence
Intellectual functioning was found to be remarkably variable, with Full IQ scores ranging from 32 to 129, excluding five unassessable subjects. It is well substantiated that cognitive and emotional functioning of children with JS is often difficult to assess due to impaired fine/gross motor movements, abnormal eye movement, and speech control, all causing barriers to interaction, active communication, and appropriate emotional display [Ziegler et al., 1990] with the inevitable outcome that severe intellectual disabilities are overgeneralized [Hodgkins et al., 2004]. The first clinical studies highlighted severe motor, intellectual, and social disabilities; however, formal cognitive assessments had not been used [Boltshauser and Isler, 1977; Curatolo et al., 1980; Aicardi et al., 1983; Gitten et al., 1998; Kumandas et al., 2004]. Most clinical studies still confirm that developmental delays and intellectual disabilities are key features of the syndrome [Romani et al., 2014], and to date patients with JS with normal IQ have rarely been reported [Gunay-Aygun et al., 2009; Poretti et al., 2009; Romani et al., 2014]. The present study demonstrates a normal or borderline cognitive functioning in up to 28% (15/54) patients, a proportion that is much higher than expected. The reliability of the assessment is ensured by the expertise of neuropsychologists, working in centers specialized in the diagnosis and management of patients with JS, and by the use of tools with standardized methods of administration and scoring. Such a high percentage of normal or borderline IQs could stem either from the examination of a large sample, allowing for better detection of the heterogeneity of cognitive profiles, or from the increasing capacity to diagnose also those subjects with a very mild phenotype. Furthermore, 7 of the 15 subjects with IQ within the normal range were evaluated with Leiter-R due to the presence of serious language/speech disorders; in these patients, verbal impairment may hinder the adaptive capacity regardless of preserved IQ; if assessed with inadequate tests, these patients might have been misclassified as intellectually disabled.
Intellectual disability was found in 72% (39/54) of patients, and thus continues to represent a hallmark of the syndrome but cannot be considered a mandatory diagnostic criterion of JS. The profiles obtained by Leiter-R and Griffiths developmental scales were homogeneous, while the Wechsler scales showed significant differences among both verbal and performance subtests. The arithmetic and comprehension items were weak points of verbal functioning, with relative preservation of reasoning by similarities, and coding was a weak point on performance tasks. These findings seem to confirm, on a wider sample, the specific peaks, and valleys profile found in four patients with JS by Tavano and Borgatti [2010]. In accordance with the freedom from distractibility factor by Kaufman [1979], the low scores in arithmetic and coding may be interpreted as a working memory deficit and an impairment in the capacity to provide temporary storage and manipulate information, as confirmed by the correlation with digit span on the Wechsler scales. As the coding score was not significantly correlated with the VABS motor rQs, this would indicate that poor performance in the task was due to a difficulty in managing double tasks rather than a motor deficit.
Adaptive Behavior
The VABS showed that motor organization was the area of vulnerability of the adaptive functioning profile, its quotients being significantly lower than both the ABC (sum of communication, daily living, and socialization domains) and the cognitive scores (Wecshler and Leiter-R IQs, and Griffiths GQ). It may be that motor disabilities could affect all other areas of adaptive behavior, possibly limiting the acquisition of personal care (hygiene and getting dressed), social (play and sport autonomy), and scholastic (drawing and writing) skills.
On the contrary, the communication rQ was higher than the daily living and socialization rQs, confirming the clinical evaluation of patients with JS as effective and discrete communicators, despite their language impairment, ranging from its complete absence, to an understandable speech. The patients’ communicative skills in the daily context appear relatively preserved as they are sustained by communicative intentionality, good interaction with the environment, and attention to others’ verbal messages [Braddock et al., 2006].
Emotional and Behavioral Functioning
The results indicate quite good emotional and behavioral functioning in subjects with JS. Most children did not show maladaptive behaviors consistent with a psychiatric diagnosis. Four patients met the criteria for a DSM-oriented psychiatric diagnosis (i.e., two oppositional defiant and two bipolar disorders), and two showed the triad of symptoms typical of the autistic spectrum disorder (i.e., absent verbal communication, impairment in reciprocal social interaction, stereotyped and repetitive behaviors) associated with severe intellectual disability, unassessable with standardized testing, and sensory and motor disabilities, constituting a very complex picture. The percentage of psychiatric diagnoses in our JS group (7.4% or 11% including the two subjects with autistic-like symptoms) is consistent with that of large cohort studied by Bachmann-Gagescu et al. [2015] in which 47 subjects (8.8%) showed a variety of mental health problems such as anxiety, aggression, depression, and autism. Our findings are in disagreement with the studies reporting a high prevalence of autism in JS [Holroyd et al., 1991; Ozonoff et al., 1999], but are in line with Takahashi et al.'s [2005] hypothesis that JS is a genetically distinct disorder from autism. These authors found that, on 47 children with JS evaluated with the autism behavioral checklist, no child met the clinical cut-off for autism (parents’ symptom report), and that only 4 out of 32 exhibited clinically significant borderline symptoms of autism, with an overall profile more similar to the one expected for developmental delay. Steinlin et al. [1997] previously described 16 children with JS as pleasant, friendly, easy to guide, and socially included, although some had a tendency to react in a mildly aggressive manner when their handicap was pushing them to their limits. Moreover, the verbal children of the Steilin's group had relatively spared communicative skills even if they produced only simple sentences with flat prosody and hoarse voice. More recently, Braddock et al. [2006] also confirmed that patients with JS typically had verbal and tongue apraxia with reduced speech control, but showed good communicative skills including effective gestures, particularly in those with less intelligible language. Overall, it can be concluded that patients with JS did not show classic symptoms of autism spectrum disorder.
Although psychiatric diagnoses are rare, a subset of approximately 40% displayed inattention, hyperactivity, social withdrawal, and atypical behaviors that affected parents’ ability to manage the child's physical and emotional needs. The prevalence of behavioral and emotional problems detected by the CBCL is very high when compared to typically developing Italian children [Gritti et al., 2014] and adolescents [Frigerio et al., 2009], but not when compared to populations with neurodevelopmental disorders, such as intellectual [Masi et al., 2002] and learning [Capozzi et al., 2008] disabilities. In our sample, internalizing problems (anxiety/sociality) were confirmed as common, and the CBCL total score was negatively correlated with the level of global social adaptive functioning. It seem to suggest that emotional and behavioral problems impact on the patients’ adaptive behavior, in particular reducing the social competence and daily-life independence, consequently increasing the perceived parental stress in everyday management [Farmer et al., 2006]. This result is an interesting and novel finding that needs to be confirmed in other larger JS cohorts.
Developmental Approach
An interesting result was the positive correlation found between chronological and equivalent age on cognitive and adaptive behavior tests. Although in presence of slow, progressive improvement, these findings can be considered developmentally as a continuum with gradual acquisition of new skills until adulthood. This interpretation refutes the conclusions of some long-term follow-up studies on patients with JS which suggested that motor and cognitive deterioration occurs across their life span [Cantani et al., 1990; Gitten et al., 1998], while it is consistent with the conclusions of Tavano and Borgatti [2010] and with the data on single cases reported by Ziegler et al. [1990]. Also Romani et al. [2014] reported two cases of patients with severe developmental delay until 5 years of age, who, at later follow-up, showed unexpected and exceptional mental abilities. As these data are cross-sectional, a longitudinal study needs to confirm these observations.
Our data also suggest that there is discontinuity between developmental delay and intellectual disability [Shevell et al., 2003]. In fact, five out of eight subjects with a clinical history of normal global development were later diagnosed by us with intellectual disability, conversely 12 out of 15 children with normal IQs at our testing had a history of global developmental delay.
Limitations
Variability in the cognitive and behavioral phenotype is very common in genetic syndromes, especially during development.
The daily clinical work demonstrates to neuropsychologists and child neurologists that it is necessary to choose the best possible tool for each patient, that is, that can describe cognitive and behavioral functioning with more effectiveness. This attention in individualizing the assessment implicates that it is impossible to use a unique test, which constitutes a clinical strength but a methodological limitation.
However, the wide range of age, the different degrees of sensorial impairment and the severity of intellectual disability within 54 subjects with JS required the use of different tools for the collection of intelligence data.
The correlations between the cognitive/behavioral profiles and the genetic causes of the disease is not applicable because the genotype is not fully defined yet [Romani et al., 2014]. To date, biallelic mutations in about 30 genes, all involved in primary cilium biology, are known to compose the genetic spectrum of JS. However, the genetic cause remains unidentified in nearly 40% of JS-affected individuals [Bachmann-Gagescu et al., 2015], and the neuroradiological identification of the molar tooth sign still remains the diagnostic tool for JS [Romani et al., 2013; Poretti et al., 2014].
CONCLUSIONS
This study included the participation of a sizeable group of patients with JS and a defined protocol composed of standardized tests to obtain clinically reliable and statistically comparable results. Cognitive functioning is extremely variable in JS, ranging from severe disability to normal, to even above average intelligence, and it strongly correlates with adaptive function. Most children did not show maladaptive behaviors consistent with a psychiatric diagnosis but approximately 40% of them presented emotional and behavioral problems.
Further longitudinal studies will be able to assess cognitive development, social, language, and behavioral skills throughout the lifespan. Since no therapies are available to treat this syndrome, such longitudinal studies are particularly important to guide the rehabilitation process of affected children, aiming to improve their functioning, their skills, and their overall quality of life.