Quality of life, unmet needs, and iatrogenic injuries in rehabilitation of patients with Ehlers–Danlos Syndrome hypermobility type/Joint Hypermobility Syndrome
Abstract
Ehlers–Danlos Syndrome, hypermobility type (EDS-HT) and the joint hypermobility syndrome (JHS) are connective tissue disorders that form an overlapping clinical syndrome and are associated with frequent medical visits and substantial morbidity. EDS-HT/JHS-associated pain correlates with poor quality of life. While physical therapy is the recommended treatment for EDS-HT/JHS, little is known about therapy-related patient experiences and iatrogenic injuries. We studied 38 adult EDS-HT/JHS patients, eliciting health-related quality of life (HRQoL) from 28 patients through the RAND SF-36 questionnaire. We also explored physical therapy experiences through focus groups with 13 patients. Our patients displayed poor HRQoL, with 71% reporting worse health over the past year. SF-36 scores were significantly lower than the scores of the average American population (P < 0.001 for 8 of 10 categories assessed), but were comparable to EDS-HT/JHS populations in Belgium, the Netherlands, Sweden, and Italy. Focus groups identified factors associated with: negative past physical therapy experiences, iatrogenic joint injuries, positive treatment experiences, and unmet rehabilitation needs. This group of EDS-HT/JHS patients has significant decrements in HRQoL and many unmet treatment needs, as well as a risk for iatrogenic injuries. We identify several approaches to help meet patients' needs and improve joint rehabilitation in patients with EDS-HT/JHS. © 2016 Wiley Periodicals, Inc.
INTRODUCTION
Ehlers–Danlos Syndrome (EDS) is a connective tissue disorder chiefly characterized by joint hypermobility, musculoskeletal pain, and skin findings. It encompasses a number of subtypes, of which the classical and hypermobility types are the most common. This study explores the hypermobility type of EDS, which is readily distinguished from vascular and classical EDS by the lack of visceral rupture, arterial findings, and widened atrophic scars [Castori et al., 2010b]. The overall incidence of EDS is disputed; studies have historically estimated a prevalence of 1 in 5,000, [Pyeritz, 2000] but the condition is likely under-diagnosed according to current diagnostic guidelines [Hakim and Sahota, 2006; Castori et al., 2013; De Wandele et al., 2014]. The joint hypermobility syndrome (JHS) shows substantial clinical and familial overlap with the EDS hypermobility type, (EDS-HT) [Beighton et al., 1998; Grahame et al., 2000; Hermanns-Lê et al., 2012] leading to a consensus that EDS-HT and JHS are variable expressions of the same disorder [Tinkle et al., 2009; Castori, 2013; De Wandele et al., 2013]. In separate literature, JHS has been reported as a relatively common condition, affecting five to 20% of women and 1% of men in the general population [Beighton et al., 1998; Russek and Errico, 2015].
Patients with EDS-HT/JHS experience significant reductions in quality of life (QoL) and may have substantial disability [Rombaut et al., 2010; Murray et al., 2013; Berglund et al., 2015]. Pain associated with EDS-HT/JHS is associated with reduced quality of life, decreased physical activity time, and psychiatric illness [Rombaut et al., 2010; Hershenfeld et al., 2015]. Many patients also face negative attitudes from providers, are often belittled or ignored, and face delayed diagnosis as a result [Berglund et al., 2010]. Early diagnosis is important in avoiding unnecessary surgeries and preventing further functional decline, but is also difficult to achieve due to the wide range of symptoms, delayed presentation in some patients, and overlap with routine musculoskeletal complaints.
No conclusive research exists as to the best treatment options for pain and disability in EDS-HT/JHS; many patients use medications, surgery, physical therapy, and other modalities but their effectiveness has not been well studied [Rombaut et al., 2012]. Physical therapy is widely regarded as the mainstay of EDS-HT/JHS treatment, [Simmonds and Keer, 2007; Sahin et al., 2008; Simmonds and Keer, 2008; Kemp et al., 2010] but there is no consensus on the method of treatment among these studies. Furthermore, physical therapists in one study reported a lack of knowledge about EDS-HT/JHS, and were not comfortable assessing and treating patients with EDS-HT/JHS [Rombaut et al., 2015]. This lack of knowledge is crucially important because patients with joint hypermobility have unique rehabilitation needs [Sahin et al., 2008]. In our EDS-HT/JHS population, many patients have reported that standard physical therapy has caused them injury and worsened disability, in part due to therapists' lack of familiarity with EDS. Our goal in this study was to characterize the health-related quality of life (HRQoL) of our patients with EDS-HT/JHS and to explore their needs and experiences surrounding physical therapy.
METHODS
Study Design
This study used two approaches to explore patient needs in our EDS-HT/JHS population. The first was to gather baseline data on HRQoL by using a validated questionnaire, the RAND SF-36. The SF-36 is a well-validated questionnaire completed by the patient that assesses various dimensions of health on a scale from 0 to 100 [Ware, 2000]. This questionnaire has been used in EDS-HT/JHS populations in Sweden, the Netherlands, Belgium, and Italy but not previously in patients from the United States [Verbraecken et al., 2001; Castori et al., 2010b; Rombaut et al., 2010; Berglund et al., 2015]. The second was to obtain qualitative information on patients' past experiences with physical therapy through a series of focus groups.
Participants
Participants for the study were recruited from 2013 to 2015 from an adult medical genetics clinic, a local patient support group, and a university-affiliated physical therapy program for patients with suspected or confirmed EDS-HT/JHS. Patients were selected on the basis of a self-reported diagnosis of EDS-HT/JHS, treatment for EDS-HT/JHS, or a clinical diagnosis of EDS-HT/JHS. We clinically assessed all patients participating in the SF-36 questionnaire, but did not take specific steps to confirm a diagnosis of EDS-HT/JHS in patients who participated in the focus groups only. Patients were over 18 years of age, not pregnant, and English-speaking. Participants in the focus groups were recruited by email and print advertisements for the medical genetics clinic, physical therapy program, and local support group. In all, 38 patients participated in the study; 13 participated in the focus groups and 28 completed at least one SF-36 questionnaire. Two patients participated in both parts of the study.
Data Collection
Eligible patients seen at the university-affiliated physical therapy program who chose to participate in the study were offered an SF-36 questionnaire to complete at the physical therapy site. Of 29 patients, 28 submitted a completed questionnaire and informed consent, and were included in the study. Participants in the focus groups provided oral data that was audio-recorded and transcribed, and the researcher conducting the focus groups noted impressions after each group.
Questionnaire Data Analysis
The questionnaires were scored according to the RAND SF-36 scoring instructions, and composite scores calculated. Scores range from 0 to 100, with lower numbers indicating worse health-related quality of life. Using the 36 questions, eight composite scores are calculated, including two major composites: Physical Component and Emotional Component, as well as minor composites Physical Functioning, Physical Role Limitation, Emotional Role Limitation, Vitality, Mental Health, Social Functioning, Bodily Pain, and General Health. A single question is also used to assess Health Change. Scores were averaged and then compared to a randomly selected American population (n = 22,462)[McHorney et al., 1993; Ware, 2000]. Summary statistics were computed using standard methods, and an independent Student's T-test with heteroscedasticity was used to compare EDS-HT/JHS group scores to the randomly selected American group scores.
Focus Group Data Analysis
Focus group audio was transcribed and analyzed using a framework approach [Swallow et al., 2003; Rabiee, 2004]. Briefly, one investigator (CB) used immersion in the data to become familiar with all transcripts and verify data saturation, and was also the person conducting all focus groups, which helped with full data immersion [Ward et al., 2013]. Recurring themes were then identified, charted, and organized into sub-themes. These themes were then applied back to the original transcripts to create an analytical framework, and thematic saturation was demonstrated. Finally, representative quotations from the original transcript were used to highlight particular themes and the overall synthesis.
RESULTS
Participants
Overall, 38 patients participated in this study. Table I lists demographic characteristics of the patients. Our participants were mostly female (84.6%), a trend noted in other EDS-HT/JHS populations as well [Castori et al., 2010a; Rombaut et al., 2011; Russek and Errico, 2015]. The questionnaire arm contained 88% women, compared to 76% women in the focus group arm.
| SF-36 arm (n = 26) | Focus group Arm (n = 13) | Total (n = 38) | |
|---|---|---|---|
| Sex | |||
| Percent female | 84% | 76% | 82% |
| Percent male | 15% | 23% | 18% |
| Age—median (range) | 35 (19–64) | 40.5 (28–57) | 36 (19–64) |
| BMI—mean | 24.6 | 26.6 | 24.9 |
- BMI, body mass index.
SF-36 Questionnaire Data
The data from SF-36 questionnaires indicate that EDS-HT/JHS patients have an overall decreased HRQoL, with low physical and emotional component scores (Table II). Measures of physical ability, including the physical component score (PCS), physical functioning (PF), role limitation from physical causes (RP), and bodily pain (BP) were notably low. Furthermore, when physically related and emotionally related scores are paired, the physically related scores are lower: mean PCS was 30.0 compared to mean emotional component score (ECS) of 51.0. Likewise, mean role limitation from physical causes (RP) was 10.2, much lower than mean role limitation from emotional causes (RE), which was 59.2. Notably, there was greater variation in ECS scores than PCS scores.
| SF-36 components | Mean score | Standard deviation |
|---|---|---|
| PCS | 30.0 | 20.9 |
| ECS | 51.0 | 22.0 |
| PF | 39.6 | 26.0 |
| RP | 10.2 | 18.7 |
| RE | 59.2 | 43.7 |
| V | 26.3 | 19.7 |
| MH | 59.9 | 17.1 |
| SF | 32.2 | 23.4 |
| BP | 21.9 | 21.4 |
| GH | 26.8 | 16.9 |
| Health change | 30.8 | 28.6 |
- F-36 scores are reported on a scale of 0–100, with 0 representing severe impairment and 100 representing perfect function with no impairment. The following are composite scores and their abbreviations: PCS, physical component score; ECS, emotional component score; PF, physical functioning; RP, role limitation physical; RE, role limitation emotional; V, vitality; MH, mental health; SF, social functioning; BP, bodily pain; GH, general health. Health change is a single-item question for which 0 represents “my health is much worse than this time last year” and 100 represents “my health is much better than this time last year.”
A single-item question also assessed patients' perception of changes in their health overall during the previous year (Fig. 1). Notably, most patients (73%) felt that their health has worsened in the past year, with the majority assessing their health as somewhat worse (46%). Only 19% of patients felt their health had improved during the past year.
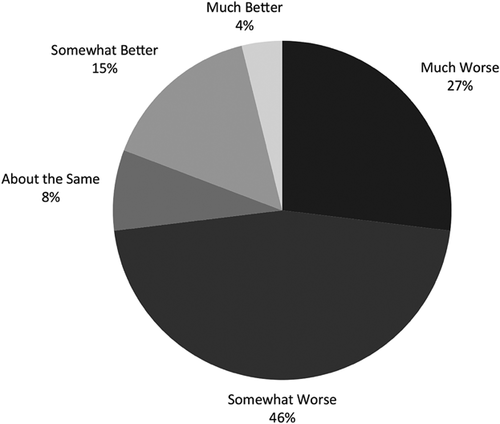
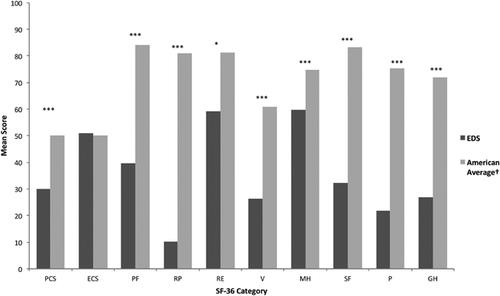
Figure 2 compares this group of EDS-HT/JHS patients with a representative sample of the American population [Ware, 2000]. Compared with the average American population, EDS-HT/JHS patients had statistically significant decreases in health-related quality of life in almost all measures. The only exception was the emotional component score. In addition, all measures except for RE scores were significantly different at the P < 0.001 level.
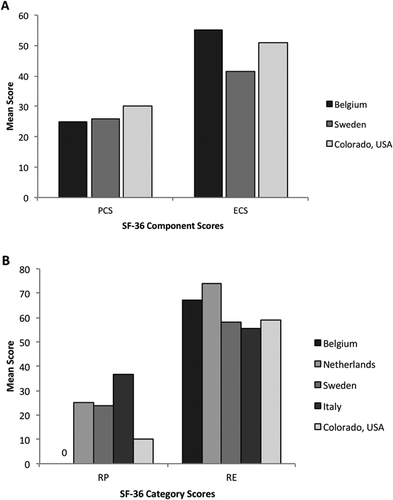
We also examined whether our EDS-HT/JHS population was similar to other such populations in terms of HRQoL. While no other American EDS-HT/JHS studies exist using the SF-36 to measure HRQoL, there are four similar studies internationally that use the SF-36 (Table III) [Verbraecken et al., 2001; Castori et al., 2010b; Rombaut et al., 2010; Berglund et al., 2015]. We found that our EDS-HT/JHS population had similar HRQoL to EDS-HT/JHS populations in other countries (Fig. 3). Figure 3A highlights mean PCS and ECS scores of our patients compared to the two populations that included these measures. The PCS in particular was very similar; the Belgian group had a mean score of 25, the Swedish group had a mean score of 26, and our group had a mean score of 30 on the PCS. Figure 3B includes all four other studies and compares the mean physical and emotional role limitations (RP and RE, respectively). All five data sets show distinctly lower RP and higher RE scores.
Focus Group Data
Our focus group analysis revealed poor past experiences with physical therapy for EDS-HT/JHS, highlighted unmet needs, and suggested factors that could contribute to high-quality treatment. Providers' lack of knowledge about EDS-HT/JHS was frequently described as a causative factor in receiving poor-quality care, and education frequently cited as a way to improve the quality of care.
Factors Leading to Iatrogenic Injuries
“The shoulder exercises they would tell me to do…were the exact exercises that caused my shoulder to pop out initially.”
Patients also cited delayed diagnosis, poor communication with providers, and lack of provider education about EDS-HT/JHS as factors behind their iatrogenic injuries.
Other Factors Contributing to Poor-Quality Care
“I hate getting that vibe from people…I'm the last person who would want to make this up!”
Several patients felt the need to leave primary care and specialty practices as a result of provider attitudes toward their EDS-HT/JHS diagnoses.
Contributors to High-Quality Care
“The whole medical system is set up so that it was focused on my feet. But now my PT recognizes to work on the whole body, not just my feet.”
Another key component of a positive experience was the use of multiple modalities, such as complementary medicine and therapy techniques. Massage, pool therapy, yoga or Pilates, manual manipulation, and dry needling were often cited as helpful; a few patients also experienced benefit from chiropractic and acupuncture treatments. Other desired features were multi-disciplinary coordination across the healthcare system; a focus on stabilizing joints, rather than mobilizing them; and teaching patients tools to promote safety.
Provider Knowledge of EDS-HT/JHS
“My experience is that the PTs [Physical Therapists] just don't know about [EDS].”
“I just needed to see somebody who knew what we were dealing with. I didn't want to be the educator.”
Increasing healthcare provider education about treating EDS-HT/JHS was the most common suggestion of how to better meet the needs of the EDS-HT/JHS patient population. Knowledge about EDS-HT/JHS played into all key themes of the framework, touching on negative and positive experiences with joint rehabilitation as well as solutions to meet patients' needs in the future.
DISCUSSION
This is the first study to quantify poor health-related quality of life in American adults with EDS-HT/JHS, and also the first to explore patient needs surrounding physical therapy for hypermobility. Given the high prevalence of JHS in studies and its link with EDS-HT, this condition appears to be under-studied in the United States, and information leading to improvements in joint rehabilitation is vital for this growing population. Furthermore, the occurrence of at least one injury attributed to formal physical therapy in 38% of patients indicates a need to dramatically change practice in joint rehabilitation for hypermobile patients. Even if not all of the reported injuries were directly due to physical therapy, the high prevalence of perceived harm related to physical therapy may undermine patient trust and acceptance of referrals to physical therapists.
The SF-36 data suggest that while EDS-HT/JHS patients experience both physical and emotional limitations, the physical limitations have a greater impact on quality of life. Scores like the PCS, RP, and pain components are highly linked to physical complaints, [Castori et al., 2010b] and these were some of the lowest score categories. While mental and emotional health categories like ECS, RE, MH, and SF were low, they were not as uniformly low as categories pertaining to physical health. These results are comparable to those obtained in several other EDS-HT/JHS populations worldwide, confirming that physical limitations including pain are the major challenge facing EDS-HT/JHS patients.
In addition, analysis of the Health Change question reveals deteriorating health for most of the patients surveyed. This information is consistent with the natural history of EDS-HT/JHS as a chronic illness [Castori et al., 2013]. Furthermore, this chronic disease causes significant reductions in HRQoL compared to the American population as a whole. Taken in combination with the increasing rate of diagnosis and relatively high prevalence of EDS-HT/JHS, this finding justifies increased research into assessment of hypermobility and treatment for EDS-HT/JHS.
Focus groups have previously been employed to assess patients' experiences with physical therapy [Palmer et al., 2015; Terry et al., 2015]. In one study, Palmer et al. found substantial agreement between EDS-HT/JHS patients and physical therapists on important features of a good treatment program. These included many themes appearing in this study as well, such as knowledgeable providers, a holistic approach, and recognition of the chronic nature of the condition [Palmer et al., 2015]. A similar study examined patient experiences of JHS symptoms and diagnosis, also noting that patients struggled to find knowledgeable providers who expressed positive attitudes toward JHS [Terry et al., 2015]. However, this study is the first to characterize patient interactions with physical therapists in the U.S. healthcare system, and the first to describe patient-reported iatrogenic injuries caused by physical therapy.
Several important features emerge from the results on these apparent iatrogenic injuries. Notably, a lack of therapist education on joint hypermobility appears to be a risk factor for injury, as does following a set protocol without accounting for the patient's hypermobility. These two trends suggest a role for development of specific EDS-HT/JHS protocols in rehabilitation, to minimize the risk of patient injury and increase provider comfort in treating EDS-HT/JHS patients. Many physical therapists do not feel comfortable assessing and treating EDS-HT/JHS patients, [Russek et al., 2014] making a protocol even more desirable. Components of such a protocol could draw from these focus group data to include a whole-body approach, need for long-term maintenance care, incorporation of multiple rehabilitation techniques, and patient-centered care that addresses safety and stability. Encouragingly, data suggest that physiotherapeutic interventions can be effective in improving patient quality of life [Ferrell et al., 2004] as well as specific functional measures [Sahin et al., 2008]. Finally, there is a growing need for physicians, physical therapists, and all health professionals to recognize signs of EDS-HT/JHS and be able to manage hypermobile patients. Further education through primary literature will help to achieve this goal and increase awareness of EDS-HT/JHS among healthcare providers.
LIMITATIONS
A principal limitation of this study is the small number of patients who participated and the recruitment of patients from a single genetics practice. Subjects were also somewhat self-selected and bias due to participation of only a subset of our clinical population cannot be excluded. Our data collection methods used standardized tools but also included focus group data that was likely more subjective. Patients participating in the focus groups did not receive a clinical evaluation as part of this study, so some of these patients may not have EDS-HT/JHS or may have other EDS subtypes besides the hypermobility type. Reported injuries due to physical therapy were self-reported by patients but verification of these injuries, many of which included elevations of pain without documented new musculoskeletal pathology, was not possible in this study. The perspective and knowledge of EDS-HT/JHS in the treating physical therapists was not assessed, thus the physical therapy approaches used in this population were not measured.
CONCLUSIONS
Patients with EDS-HT/JHS are likely under-diagnosed, under-studied, and face challenges with many aspects of diagnosis and treatment. In this study, we found poor health-related quality of life in 27 patients with EDS-HT/JHS, significantly worse than the general population but comparable to EDS-HT/JHS populations around the world. In addition, these patients have suffered injuries during the course of treatment, and have unmet needs relating to physiotherapeutic treatment of their injuries. Analyzing these aspects of the patient experience has provided valuable insights into quality of life, rehabilitation needs, and potential ways to improve patient care for those with EDS-HT/JHS. Our data suggest that EDS-HT/JHS patients anticipate a poor outcome with standard physical therapy. We propose that additional research is warranted into the impact, effectiveness, and safety of physical therapy in the chronically ill EDS-HT/JHS population. Consideration may be needed for an integrated care approach that combines a whole-body focus with a chronic disease perspective, utilizing multiple treatment modalities to address safety, stability, and pain management. Further studies will be needed to assess the efficacy of such programs on outcomes in this growing patient population.
AUTHOR'S CONTRIBUTIONS
CB and MT designed the study. MC conducted physical therapy sessions with patients. CB analyzed SF-36 and focus group data and conducted the focus groups. CB authored the manuscript, with input from all study authors. All contributors have read and approve of the submission of this manuscript.
ACKNOWLEDGMENTS
The authors would like to thank Jean Jirikowic, Emily Todd and Darcy Huismann for their contributions to this project through the Medical Genetics Clinic.