Frontometaphyseal dysplasia and keloid formation without FLNA mutations
Abstract
Frontometaphyseal dysplasia (FMD) is a distinctive sclerosing skeletal dysplasia associated with a number of non-skeletal manifestations including hearing loss, cardiac malformations, and stenosis, particularly of the upper airway and urinary tract. Some, but not all, patients have mutations in FLNA causing the condition. Consonant with the X chromosomal location of FLNA males are generally more severely affected than females. FLNA mutations can be detected in 82% of affected males. We describe seven patients (one male, six females) all of whom have the major clinical and radiological features of FMD, but without detectable mutations in FLNA. The females in our cohort are affected to a similar degree as is usually found in males. In addition, all patients have marked keloid formation at various body sites, including the eye, from an early age. Other features that may indicate a different etiology in these patients are the increased frequency of cleft palate, Robin sequence, tracheal stenosis, and mild intellectual disability, which all occur in three of more patients in the present group. All patients are isolated. We hypothesize that the presently reported patients represent further evidence that phenotypes strongly resembling FMD exist that are not accounted for by mutations in FLNA. Since the frequency of several of the manifestations, their sporadic presentations, and the presence of keloid formation differ from the X-linked form of this condition we propose de novo autosomal dominant acting mutations in a gene functionally related to FLNA, underpin this disorder. © 2015 Wiley Periodicals, Inc.
INTRODUCTION
Frontometaphyseal dysplasia (FMD) is one of the Oto-Palato-Digital Spectrum Disorders (OPDSD) and is characterized by a generalized bone dysplasia and a wide variety of other manifestations such as hearing loss, cardiac malformations, and urogenital defects [Robertson et al., 2006; Hennekam et al., 2010]. The clinical diagnosis of FMD can be molecularly confirmed in 82% of male cases by finding mutations in the X-linked gene FLNA, encoding filamin A (FLNA) [Robertson, 2005]. FLNA is a protein that participates in the modulation of the cytoskeleton through cross-linking actin and scaffolding a diverse array of juxta plasma membrane proteins. Loss of function mutations in FLNA are associated with periventricular nodular heterotopia, and other FLNA functional alterations lead to otopalatodigital syndrome type 1 and type 2, Melnick–Needles syndrome, terminal osseous dysplasia, and FMD [Verloes et al., 2000; Robertson et al., 2003; Mariño-Enríquez et al., 2007; Sun et al., 2010].
Here we present seven patients with a clinical diagnosis of FMD, who exhibit in addition a propensity to keloid formation and several other unusual signs, and in whom no FLNA mutation could be detected. We propose that these patients have either a specific subtype of FMD or a hitherto unrecognized entity caused by mutations in a gene that may well demonstrate a functional relationship with FLNA.
CLINICAL REPORTS
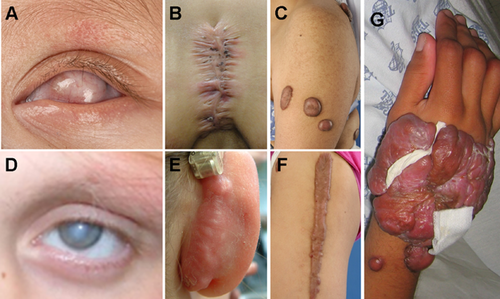
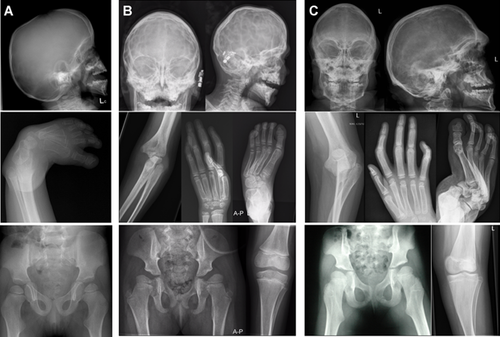
The main findings in the seven patients are summarized in Table I and illustrated in Figures 1-4. We describe the first two patients in detail, and provide a more limited description of the other patients.
| Patients | |||||||||||
|---|---|---|---|---|---|---|---|---|---|---|---|
| Literaturea (%) | 1 | 2 | 3 | 4 | 5 | 6 | 7 | ||||
| FLNA mutation | FLNA positive | FLNA negative | FLNA negative | ||||||||
| Gender | Male | Female | Male | Female | F | F | F | M | F | F | F |
| Clinical FMD characteristics | |||||||||||
| Height <10th centile | 21 | 0 | 0 | 22 | + | + | + | + | + | + | – |
| Prominent supraorbital ridges | 100 | 91 | 100 | 100 | + | + | + | + | + | + | + |
| Downslanting palpebral fissures | 100 | 64 | 100 | 89 | + | + | + | +/− | + | + | + |
| Hypertelorism | 100 | 100 | 100 | 100 | + | + | + | + | + | + | + |
| Cleft palate | 0 | 9 | 0 | 11 | + | + | Ua | − | − | + | + |
| Micrognathia | 70–90 | 85–100 | unk | unk | + | + | + | + | − | + | − |
| Dental anomalies | 100 | 18 | 33 | 11 | + | + | + | + | − | + | + |
| Muscular underdevelopment | 86 | 9 | 100 | 67 | + | − | + | + | + | − | + |
| Restricted elbow movements | 100 | 45 | 100 | 44 | + | + | + | + | + | + | + |
| Flexion contractures wrist | 85–100 | 65–75 | unk | unk | + | + | + | + | − | − | + |
| Ulnar deviation hands | 85–95 | 70–90 | unk | unk | + | + | − | + | − | + | + |
| Interphalangeal joint contractures | 89 | 90 | 100 | 67 | + | + | + | + | + | + | + |
| Long slender digits | 89 | 45 | 100 | 56 | + | + | + | + | + | + | + |
| Distal phalangeal wide/small thumb | 80–95 | 70–90 | unk | unk | + | + | + | + | + | + | + |
| Camptodactyly | 89 | 81 | 100 | 44 | + | + | + | + | + | + | + |
| Deafness | 67 | 27 | 100 | 33 | + | + | + | + | + | + | + |
| Tracheal stenosis | 25 | 9 | 0 | 11 | − | − | − | + | + | − | + |
| Cardiac defect | 24 | 0 | 66 | 22 | + | + | + | − | + | + | − |
| Urethral obstruction | 32 | 0 | 0 | 0 | − | − | − | − | − | − | − |
| Radiological FMD characteristics | |||||||||||
| Supraorbital hyperostosis | 100 | 100 | 100 | 100 | + | + | + | + | + | + | + |
| Antero inferior mandibular spurt | + | + | + | + | + | + | − | + | − | − | unk |
| Craniosynostosis | 5 | 0 | 0 | 0 | + | + | − | − | − | − | − |
| Skull base sclerosisb | 100 | 100 | 100 | 100 | + | + | + | + | + | + | + |
| Absent frontal sinuses | 89 | 54 | 100 | 68 | + | + | + | + | + | + | + |
| Dislocated radial heads | 44 | 9 | 100 | 11 | + | + | + | + | + | + | + |
| Carpal fusions | 0 | 9 | 66 | 0 | − | − | − | − | − | − | − |
| Poorly modeled phalanges | 100 | 36 | 100 | 44 | + | + | + | + | + | + | + |
| Abnormally modeled meta/diaphyses | 100 | unk | 100 | unk | + | + | + | + | + | + | + |
| Undermodeling metatarsals | 100 | unk | 100 | unk | + | + | + | + | + | + | + |
| Fusion C2/3—subluxation C3/4 | 33 | 0 | 66 | 11 | − | + | − | + | + | + | − |
| Scoliosis | 53 | 18 | 33 | 33 | − | + | + | + | + | − | + |
| Bowed long bones | 56 | 18 | 100 | 11 | + | + | − | − | − | − | + |
| Non-FMD characteristics | |||||||||||
| Keloid/hypertrophic scars | + | + | + | + | + | + | + | ||||
| Coxa valga (radiological finding) | + | + | + | + | + | + | + | ||||
| Pes equinovarus | + | + | + | + | + | − | + | ||||
| Hirsutism | + | + | − | − | + | − | − | ||||
| Mild intellectual disability | + | + | − | − | + | − | − | ||||
| Sacral dimples | + | + | − | − | − | − | − | ||||
| Robin sequence | + | + | − | − | − | − | − | ||||
| Eye abnormalitiesc | + | − | + | − | − | − | + | ||||
| Large joint dislocation | + | − | + | − | + | + | + | ||||
| Thickened knee joints | − | + | − | − | − | − | − | ||||

Patient 1
The proband is the first child of healthy, unrelated parents. Her mother is of Caucasian extraction, and known to have beta-thalassemia trait. Her father is of Surinam Creole origin and he has a daughter from a previous relationship with pubertas praecox (precocious puberty) due to a pituitary disorder. The proband was born at term after an uncomplicated pregnancy and delivery with a birth weight of 2.270 g (−2.5 SD), length of 49 cm (0 SD) and head circumference of 31.5 cm (−2.5 SD). She presented at birth with Robin sequence: a cleft palate, micrognathia, and significant respiratory and feeding problems requiring a nasopharyngeal airway for 12 months and tube feeding from birth until the present day. In addition, she was found to have marked left corneal thickening; it was unsure whether this was attributable to thickening of the cornea or dermoid formation (Fig. 3). The anterior chamber of the left eye was very shallow. The right eye was structurally normal with unimpaired acuity. She was also noted to have mild wrist contractures, ulnar deviation of the fingers, which had flat and broadened distal phalanges, most marked in the thumb, limited mobility of her elbows, pedes adducti, and radiologically confirmed bilateral hip dislocation (Fig. 2). At examination she had short downslanting palpebral fissures, hypertelorism, a low nasal bridge, full cheeks, low-set ears with a large antitragus, a small mouth, and a dimple in her chin. Echocardiography showed a small hemodynamically insignificant ventricular septal defect.

Brachy-turricephaly was evident at 9 months and X-rays showed bicoronal craniosynostosis for which surgery was not required. Her palate was repaired at 18 months, at which time bilateral conductive hearing loss was diagnosed and hearing aids were fitted. She had delayed motor milestones and walked independently at 3 years of age. Her cognitive development was also slow and she uttered her first words at 5 years. The hip dislocations needed surgical correction at age 3 years, after which she developed large keloids on both legs. These were removed but subsequently recurred (Fig. 3). At age 4 years, she developed a recurrent, severe infection of her left eye culminating in endophthalmitis, which was refractory of intensive treatments. At 5 years the eye was enucleated, and a prosthesis was inserted. Audiometry showed a conductive loss of 70 dB (lower tones) and 50 dB (higher frequencies) in the left ear and complete deafness of the right ear. Pathological examination of the enucleated eye confirmed the endophthalmitis but failed to show other specific abnormalities.
She was last evaluated at age 5.5 years. Her height was 113.6 cm (0 SD), weight was 18 kg (−2 SD), and head circumference (measured over the supraorbital ridges) 48 cm (−1 SD). The initial physical findings had persisted but her supraorbital ridges had become more prominent, and her wrist and finger contractures had progressed. The muscle bulk in the lower arms, calves, and lower legs was underdeveloped. Array CGH showed a gain of 30.8 kb of 22q12.3, which was also present in her unaffected mother. MLPA of subtelomeric probes failed to show imbalances.
Patient 2
This female patient was born at term as the 5th child of healthy, unrelated parents. Her siblings were normal. Routine prenatal ultrasounds had shown a somewhat small cerebellar vermis. Her birth weight was 2,925 g (−1 SD), length 54 cm (2 SD), and head circumference 33.0 cm (−1 SD). A cleft palate and micrognathia were present, causing respiratory and feeding problems, which necessitated hospitalization for months (Robin sequence). She had long, thin fingers held in a wind-swept position, ulnar deviation of the hands, and pedes equinovari. Her motor and cognitive developments were delayed and she required special education. At age 2 years, she was found to have bilateral conductive hearing loss of 70 dB for which hearing aids were provided. In addition she had very narrow external auditory canals associated with recurrent otitis externa and treated surgically. Eye examination at 6 years of age yielded normal results other than showing that the lower temporal part of both corneas colored significantly resembling exposure keratopathy but she closed her eyes normally during sleep.
At the age of 6 years, she began to develop small keloid lesions, mainly over the upper thorax and upper arms, often without an obvious initiating event. She developed further intensely itchy keloid scars after any surgery and chicken pox. Her primary dentition erupted normally but exfoliation was limited to a few elements. Because of irregularly placed teeth orthodontic braces were provided.
At 13.5 years, her height was 149 cm (−2 SD), weight was 57.4 kg (+2 SD) and head circumference 52.7 cm (−1 SD). Craniofacial features included a short forehead with a low anterior hairline, prominent supraorbital ridges, broad eyebrows that were extended laterally, hypertelorism, downslanted palpebral fissures, a low nasal bridge, a short nose with a thick, rounded nasal tip, a broad nasal base, full cheeks, a short and deep philtrum, thin upper and lower vermillion, small pointed chin and irregularly implanted teeth (Fig. 1). She had a broad thorax, decreased shoulder mobility, deep sacral dimples, flexion contractures of her elbows with limited pronation–supination, mildly decreased wrist mobility, long and flat fingers, a short distal phalanx of the thumb and clinodactyly of the 5th fingers (Fig. 2). The metacarpophalangeal joints of all fingers showed decreased mobility. Her feet showed pedes adducti, and short distal phalanges of the halluces. There was mild generalized hirsutism, and multiple keloids (Fig. 3).
Over the ensuing years, the mobility in most of her joints gradually decreased despite physiotherapy and attempted surgical correction. Any surgery resulted in thick keloid scars. New keloids arose, and existing keloids expanded slowly. Echocardiography showed a bicuspid aortic valve and limited dilatation of the aortic root and proximal part of the ascending aorta (diameter 35 mm) probably secondary to the bicuspid valve. Her general health was robust, pubertal development was normal, and micturition and defecation were normal. As an adult she was largely independent for her self-care. When examined at 23.5 years of age, her height was 150 cm (−3 SD), weight was 74 kg (+3 SD), and head circumference 55 cm (−0.5 SD; OFC was 57 cm if measured over the supraorbital ridges: +1 SD). Her facial appearance has remained more or less unchanged apart from increasingly prominent supraorbital ridges (Fig. 1). Six permanent teeth had failed to erupt, and she had a number of retained primary teeth. The contractures and stiffness of her arms and digits had progressed (Fig. 2). Screening for metabolic disorders and conventional karyotyping yielded normal results.
Patient 3
The proband was born to nonconsanguineous parents at 41 weeks gestation by normal vaginal delivery after an uncomplicated pregnancy. Family history was non-contributory. Her birth weight was 3,316 g. At birth, she had multiple congenital dislocations, severe bilateral talipes equinovari, short metacarpals, thumb hypoplasia, elongation of the clavicles, high scapulae, and bilateral hip dislocation. Other findings included aortic root dilatation, which was slowly progressive over time, supra-umbilical hernia, retinal hemorrhages, pale peripheral haloes around both optic discs, deep anterior chambers, and bilateral vesico-ureteric junction obstruction. Craniofacial features included a high forehead, hypertelorism, down-slanting palpebral fissures, a short nose, a broad nasal tip with a slight midline groove, a deep inferiorly splayed philtrum, malformed ears, high palate, bifid uvula, and thin upper vermillion with a capillary hemangioma. There was reduced shoulder movement, a long narrow thorax, abnormal scapulae with overlying medial dimples, elbow contractures, wide flat thumbs adducted across the palms, and stiffness of the distal interphalangeal joints of all fingers.
She had innominate artery compression of the trachea but no treatment was required. She developed gross bilateral hydronephrosis and hydroureters, underwent a vesicostomy for neurogenic bladder, and re-implantation of both ureters. Bladder histology showed focal partial replacement of smooth muscle by fibrous tissue associated with pallor and cytoplasmic vacuolation of smooth muscle fibers. These findings were thought to resemble hollow visceral myopathy. She had numerous plastic surgeries and skin grafts for severe keloid scars. She had a talectomy of the left foot and left forefoot reconstruction. Her puberty was delayed, but hormonal profile was normal. Pelvic ultrasound showed no ovaries or uterus. She had bilateral hearing aids for sensorineural deafness. Her motor development was delayed, she walked after age 2 years, and cognition was normal. The timing of dental eruption was normal but asymmetrical. At age 2 years, her anterior fontanel was still open (25 mm). She had triangular shaped palpebral fissures, pale blue sclerae, a thick columella and alae nasi, triangular nares, a broad nasal bridge, and horizontal grooves on either side of the midline below the lower lip. She had soft translucent skin, cutis marmorata, pterygium colli, a lower cervical/upper thoracic kyphosis, and a marked pectus excavatum. Movement in almost all joints was limited, but some distal interphalangeal joints were hypermobile. She had broad short halluces and proximally placed distally broad thumbs. Keratosis pilaris of the cheeks and chin was present from birth. She had pits at the mucosal junction of the angles of the mouth and a longitudinal groove on either side of the midline of the hard palate.
At age 2.5 years she was commenced on beta blockade for aortic root dilatation. Avapro was commenced around 16 years of age. Ophthalmological examination yielded normal results. Her general health was good but she grew poorly, height was 123.7 cm (−2.5 SD) and weight was at the 3rd centile by age 9.5 years. By age 12 years 9 months, her weight was 25.6 kg −3 SD), and height 129.7 cm (−3 SD). Her joint contractures were not progressive. Urinary metabolic studies failed to show abnormalities.
Patient 4
This patient was born after a normal full-term pregnancy to healthy, nonconsanguineous Korean parents. An unusual face, undescended testes, bilateral clubfeet, and borderline finger stiffness were diagnosed at birth. At 20 days pyloric stenosis was surgically corrected. His facial appearance became more unusual with age and differed from his parents. His clubfeet did not correct fully after manipulation and serial castings and so he underwent a series of surgical corrections between 6 months and 13 years of age. His hands became gradually stiffer, and currently the metacarpophalangeal joints are fixed in 90° of flexion, while the interphalangeal joints are in extension. Keloid scars have developed at the sites of surgical incisions on the feet and at the site of a traumatic injury. Tracheal stenosis was noted at the induction of anesthesia. He developed sleep apnea, confirmed by sleep studies, likely due to the tracheal stenosis. Audiology shows mild hearing loss, which does not interfere with daily life. Cognitive function is normal and his academic performance is upper 10% in school. At age 18 years his height is 160 cm (−2 SD).
Patient 5
This girl was born at 34 weeks gestation by caesarean to nonconsanguineous parents of Mexican background. Bilateral clubfeet and finger contractures were obvious at birth. Other congenital anomalies included dislocation of the left hip, patent ductus arteriosus, and a bicuspid aortic valve. She was found to have congenital sensorineural hearing loss and wears hearing aids bilaterally. Postnatally, ongoing respiratory distress led to the diagnosis of subglottic tracheal narrowing for which a tracheostomy was created. Keloids developed progressively during childhood after surgical incisions, needle insertions, minor trauma, and on the inner thighs. Attempts to control the growth of the keloid with radiation therapy was not successful, and resulted in rebound growth of the tissue with a tendency for it to break down, become infected, and develop sinus tracts. Progressive scoliosis prompted assessment in adolescence but surgery was not performed because of her propensity to develop keloids. She has gastro-esophageal reflux, and was diagnosed with ulcerative colitis after a previous history of rectal bleeding. She completed high school, mobilized in a motorized wheelchair, could bathe herself and had held a job performing data entry. She has been admitted to the hospital repeatedly for treatment of infection and skin breakdown at various sites. At the age of 26 years she was living with her parents.
Patient 6
This girl was born to nonconsanguineous Mexican parents after an uncomplicated pregnancy and delivery. Immediately obvious at birth were multiple congenital anomalies including hypertelorism, micrognathia, a bifid uvula, restricted elbow extension, camptodactyly, and a dislocated right hip. Over childhood she developed increasing supraorbital prominence, digital flexion contractures, growth failure, right ventricular outflow tract obstruction necessitating an infundibular resection, and increasing contractures of the elbows, wrists, and hands. Surgical interventions led to the formation of excessive keloid scarring. Crohn's disease was diagnosed in adolescence and was managed medically. A bicornuate uterus was noted at the same time. At age 32 years, she held paid employment and lived autonomously.
Patient 7
Patient 7 is a 16-year-old girl born to healthy unrelated Caucasian parents with no family history of note. She was delivered at 35 weeks gestation after a normal pregnancy weighing 2.53 kg (−2 SD). She had a large patent anterior fontanel with bitemporal narrowing, a short webbed neck, crumpled ears, a cleft soft palate, thin lips, a small deeply grooved chin, a mild scoliosis, arachnodactyly of the fingers and toes with ulnar deviation and contractures, and flexion deformities of the hips, elbows, wrists, and ankles. Echocardiogram showed a mild valvular pulmonary stenosis, small patent foramen ovale and small patent arterial duct, which did not require any intervention. During intubation for her cleft repair at 6 months she was found to have a narrow trachea. She had a dislocated left hip requiring an osteotomy with internal fixation aged 16 months. She has had recurrent episodes of glue ear, treated with grommets, and developed marked bony narrowing of the auditory canals complicated by chronic otitis externa. She developed a cholesteatoma of her left ear requiring surgery. She had bilateral hearing impairment with severe sensorineural loss on the left and predominantly conductive loss on the right for which she used aids and more recently a right BAHA. At 8 years of age she had bilateral otoplasties following which she developed severe post-auricular keloid scarring which has not responded to triamcinolone injections. She has had surgery to straighten her toes associated with keloid scarring as did the surgical scar on her left hip surgery. Her other joints have been managed with physiotherapy and splinting but more recently she has developed a lumbar scoliosis from T10 to L4 of 53°. At 3 years of age she developed a left corneal opacity thought to be due to exposure and a keratopathy assumed to be caused by a reduced corneal sensation and failure to fully close her eyes at night. There were no other ocular abnormalities apart from mild hypermetropia and astigmatism. She had several retained primary teeth and missing permanent teeth. Cognitive testing at around 10 years of age showed average abilities. She has been through a normal puberty.
At 15 years of age she had a height of 155.7 cm (−2 SD) with a head circumference of 51.8 cm (−2 SD) (53.8 cm if including brows). She had a slim build triangular face and chin, with a mild asymmetry, down-slanting palpebral fissures with prominent brows, a broad nasal bridge, a short deeply grooved philtrum, and thin upper vermillion. She had mild thoracic kyphosis and lumbar scoliosis and a marked pectus excavatum, reduced movement in her shoulders and wrists, incomplete extension of her elbows and forearms fixed in pronation. Her fingers were long and slim fingers, and the right distal thumb phalanx broad. All fingers showed asymmetric contractures, the knees had mild flexion contractures and her feet were long and narrow with mild metatarsus varus and flexion contractures of the toes.
ADDITIONAL INVESTIGATIONS
The X-rays of all patients showed a remarkable resemblance and showed all major characteristics of FMD: prominent supraorbital ridges, underdeveloped sinuses, mandibular spur, mild bowing of long bones, luxation of the radial head, small lateral epicondyle of the femora, underdevelopment of the carpals and tarsals, and under modeling of the metacarpals, metatarsals, and phalanges (Fig. 4). Patient 2 had a block vertebra of C2 and C3. An orthopantomogram of Patient 2 showed six missing elements (3-5, 4-5, 1-4, 1-5, 2-4, and 2-5) and five in Patient 3 (1-2, 1-5, 2-2, 2-4, and 2-5). Patients 3 and 7 also had absent glenoid fossae. Patient 7 had a small right 12th rib and absent left 12th rib, a cone-shaped epiphysis of the thumb, a supernumerary carpal bone, multiple Wormian bones in the sagittal suture, healed coronal clefts of the lumbar vertebrae, and disproportionately long fibulae. An MRI-brain of Patient 1 showed widened Virchow spaces and no brain malformations. CT-scan brain of Patient 2 demonstrated a small cerebellar vermis and wide extra-cerebellar spaces.
Karyotype analysis and CGH arrays yielded normal results in all studied patients. In all patients, DNA sequencing failed to show a mutation in FLNA. MPLA with a custom designed probe set over FLNA (probes situated in intron 2 and exons 6, 10, 15, 19, 22, 26, 29, 34, 44, and 48) was performed in all patients and no anomalies were found. In two patients, a search for intragenic deletions using PCR amplification of FLNA exons 2–48, including intron–exon boundaries, failed to show abnormalities.
DISCUSSION
The seven patients we report have clinical and radiological findings consistent with FMD (Table I). FMD is caused by FLNA mutations on the X-chromosome. In keeping with an X-linked disorder, the classical FMD phenotype is typically present in males while females are more mildly and variably affected. Robertson et al. found FLNA mutations in 82% of clinically affected males and 45% of females. The same authors checked 10 patients with clinically FMD but without FLNA mutation, for intragenic deletions using PCR amplification of FLNA exons 2–48, including intron–exon boundaries, and did not detect any abnormality [Robertson et al., 2006]. Only the FLNA mutation negative patients from the latter cohort who had in addition keloid formation, were included in the present study, as the presence of keloids allowed us to recognize the individuals with a similar but apparently still different phenotype with more certainty. A comparison of the clinical features of those with and without detectable FLNA mutations (Table I) suggested several clinical differences, such as in the frequency of deafness, cardiac malformations, and cervical vertebral abnormalities.
The seven patients we report are unusual for a number of reasons. All six females have phenotypes of a severity usually found in FMD males, and even resembling especially markedly affected males. All seven patients have suffered from keloid scarring which is not a previously described feature of FMD. Furthermore, they demonstrate features, which are uncommon or not previously reported in FMD, particularly cleft palate (4/7, occurring as part of Robin sequence in two of them), ocular abnormalities (2/7), large joint dislocation (4/7), and intellectual disability (in 3/7).
We have been unable to find descriptions in literature of patients with FMD who have keloid or unusual scar formation. The keloid scarring in our patients has occurred early, mainly after trauma or surgery but in at least one patient without an obvious precipitant, and the scars have been resistant to conventional management. Keloid scars are often cosmetically unsightly, may restrict skin and joint mobility and may be associated with discomfort and severe itching. The pathogenesis of keloid scarring remains poorly defined with many signaling pathways and growth factors implicated in its pathogenesis. Keloid formation may cluster in families and is more common in those of African, Asian, and Hispanic descent. Keloid scarring can form part of a wider syndrome, an example being Rubinstein–Taybi syndrome where up to 24% of individuals with a heterozygous CREBBP mutation have been observed to have keloid scars [van de Kar et al., 2014]. In such cases, the keloid scars are usually located over the shoulders, upper arms, and thorax, which are also the predilection sites for isolated keloids [Abarca et al., 2014]. We remain uncertain whether the eye findings in two of the present patients are related to this keloid formation or not.
It is difficult to classify the patients. There is the obvious significant overlap with FMD, as the major characteristics of FMD are present. The present patients have manifestations such as keloid formation and intellectual disability that do not occur in FMD. Whether this is sufficient to distinguish the two entities will await further characterization [Hennekam, 2007]. None of the present seven patients had a detectable FLNA mutation and likely the patients have a different etiology for their FMD manifestations. All were sporadic and none had consanguineous parents. The females were affected to a similar degree to the male. For those patients in whom karyotyping or array-CGH testing for chromosome imbalance was performed, the results were normal. In aggregate, these findings suggest the possibility that this entity is caused by a de novo autosomal dominantly acting mutations in a gene that has a functional relationship with FLNA.