Thricho-rhino-phalangeal syndrome and severe osteoporosis: A rare association or a feature? An effective therapeutic approach with biphosphonates
Abstract
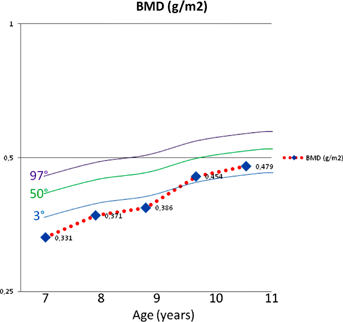
Trichorhinophalangeal syndrome (TRPS) is a rare, autosomal dominant malformation syndrome characterized by hair, craniofacial and skeletal abnormalities, skin laxity, deformation of phalanges and anomalies of pelvis, femurs, and tibias. Three subtypes have been described: TRPS I, caused by mutations in TRPS1 gene on chromosome 8; TRPS II, a microdeletion syndrome affecting the TRPS1 and EXT1 genes; and TRPS III, a form with severe brachydactyly, due to short metacarpals, and severe short stature, but without exostoses. We present the case of a 7-year-old boy, affected by TRPS with a severe osteoporosis and several spontaneous bone fractures, an association described only once in the literature, successfully treated with biphosphonates. Bone mineral density (BMD) at dual-energy X-ray Absorptiometry (DXA) was of 0.331 g/cm2 at lumbar spine with. He had four spontaneous femoral fractures in a year, and for this reason he was been operated for positioning intramedullary osteosynthesis and orthopedic supports. Due to the severity of the clinical and radiological pattern it was established, after approval of the Ethical Committee, to begin off-label therapy with infusions of neridronate at a dose of 2 mg/kg IV every 3 months. The treatment was, in this patient, effective both in terms of clinical (absence of new fractures) and mineralomethric (+45% BMD ath the lumbar level). We therefore suggest that treatment with biphosponates can be taken in account as a possible therapeutic option in case of bone fragility in patients with TRPSI. © 2013 Wiley Periodicals, Inc.
INTRODUCTION
Trichorhinophalangeal syndrome (TRPS) is a rare autosomal dominant syndrome, characterized by a triad of hair, craniofacial, and skeletal abnormalities, associated with skin laxity, deformation of phalanges, and anomalies of pelvis, femurs, and tibias [Giedon, 1966; Hall et al., 1974].
Three subtypes have been described: trichorhinophalangeal syndrome type I is characterized by a distinctive facial appearance that includes sparse scalp hair; a rounded nose; a long, flat area between the nose and the upper lip (philtrum); and thin upper lip vermilion. Individuals with this condition also have skeletal abnormalities such as cone-shaped epiphyses in their fingers and toes and short stature. People with trichorhinophalangeal syndrome type III have similar features as those with type I, but with a more severe phenotype with severe brachydactyly and short stature. Mutations in the TRPS1 gene have been found to cause trichorhinophalangeal syndrome type I and trichorhinophalangeal syndrome type III.
TRPS II, a microdeletion syndrome affecting the TRPS1 and EXT1 gene is characterized by similar phenotype associated with cognitive impairment and multiple cartilaginous exostoses [Lüdecke et al., 2001].
The TRPS1 gene (OMIM: 604386) is located on 8q24.12 and encodes for a zinc-finger (ZF) transcriptional repressor, Trps1. Trps1 binds DNA through a single GATA-type ZF that recognizes a DNA consensus sequence common to all GATA transcription factors. However, the repression activity of Trps1 maps to the C-terminal Ikaros-like double ZF motif; in vitro studies demonstrated that the presence of the DNA-binding domain is indispensable for the Trps1 repression function [Malik et al., 2001].
Osteoporosis has been rarely associated with TRPS type I. We report here on treatment with infusions of neridronate in an additional TRPS type I patient, presenting with severe osteoporosis symptomatic for recurrent fractures.
CLINICAL REPORT
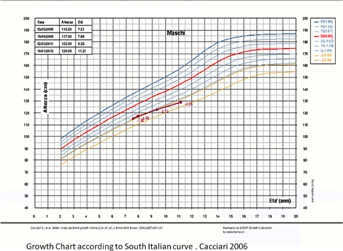
A 7-year-old boy, the eldest of two siblings of nonconsanguineous parents, was evaluated for history of recurrent bone fractures. The child had clinical and radiological features of TRPS type I, including short stature (H = 115 cm, −2 SD; W = 19 kg, −1.20 SD; BMI 15.1 kg/m2), thinning hair, bulbous nose, pectus excavatum, conical epiphyses, and a significant shortening of bilateral metacarpal and metatarsal bones (Fig. 1). Neuropsychological milestones and cognitive development were normal. At age of 5 years he had been treated for short stature and partial deficiency of GH at another hospital with human recombinant growth hormone for 6 months.

The patient was referred to our center for the occurrence of three spontaneous femoral fractures in a year. X-Rays showed the results of femoral fractures and pathological markers of bone loss. No exostoses were detected at the X-ray. Bone mineral density (BMD) at dual-energy X-ray Absorptiometry (DXA) (model Hologic 70400 Delphi) showed severe osteoporosis in lumbar spine with a BMD of 0.331 g/cm2 (normal range 0.4–0.6 g/cm2). The child was following a proper diet with an appropriate intake of calcium and he was not following corticosteroid therapies. Serum calcium metabolism values and renal function were repeatedly normal. Celiac disease, inflammatory bowel disease, thyrotoxicosis, and hyperparathyroidism were excluded.
Surgical intervention with intramedullary osteosynthesis was performed, orthopedic supports of the left femur were used and a ban on physical activities was imposed. Due to the severity of the clinical and radiological pattern it was established, after approval of the Ethical Committee, to begin off-label therapy with intravenous neridronate at a dose of 2 mg/kg IV every 3 months. After 2 years of treatment, the child has no longer experienced fractures with a normal life, and sport activities. He presented a progressive improvement in BMD and at present, DXA shows a normal BMD at the lumbar spine (BMD: 0.479 g/cm2, Z-score: 1.9 SD), right hip (BMD: 0.848 g/cm2, Z-score: 1.1 SD), and left hip (BMD 0.918 g/cm2, Z-score: 1.8 SD) (Fig. 2).
The child's growth is shown in Figure 3. His growth is still poor.
The child's father had also phenotypic features of TRPS type I, including short stature (height 156 cm), generalized scalp alopecia, tubular nose, thin vermilion of the upper lip, deviated fingers, and toes.
The father was previously surgically treated with left hip replacement because of Perthes disease. He had no history of bone fractures. A DXA analysis was performed in adult age and was normal, although at the lower level of the range of normal.
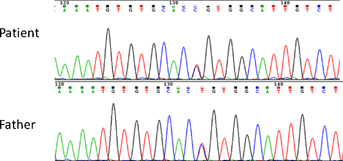
Mutational analysis was performed in the child and the father, by bidirectional sequencing of the entire coding regions of TRPS1 gene. The mutation C1233R was found in both (Fig. 4).
DISCUSSION
Review of the literature shows that severe osteoporosis is reported in a single patient with TRPS type I, carrying the de novo 1096insA mutation in TRPS1 gene [Shao et al., 2011], while significantly reduced bone mass and quail were described as a new feature of TRPS type I by Stagi et al. [2008] and Sarafoglou et al. [2010]. Therefore, osteoporosis and alterations of BMD should be considered an additional rare feature of TRPS type I. Interestingly, a single nucleotide polymorphism (rs4355801) mapping on the same chromosomal locus of TRPS1 (8q24.12) has been significantly associated with BMD and osteoporosis by genome-wide association study (GWAS) [Richards et al., 2008].
In the present case, in consideration of the occurrence of fractures and severe degree of bone demineralization, a treatment with biphosphonates a therapeutical strategy borrowed from osteogenesis imperfecta (OI), was tried. In a Cochrane meta-analysis of 2009, Phillipi et al. [2008] showed that the results from the included studies provide evidence, albeit in a relatively small population, that there is significant improvement in BMD in individuals affected with OI when treated with either oral or IV bisphosphonates. Whether the increase in BMD is a surrogate marker for fracture reduction and clinical functional improvement needs to be demonstrated. Additionally, the long-term safety of bisphosphonates in OI, particularly when used in children, and the effects of bisphosphonates on fracture and perioperative bone healing have not been sufficiently evaluated. Effects of bisphosphonates on fracture incidence, growth, bone deformity, mobility, and pain have not yet been adequately studied. Randomized controlled studies have not been realized because of the small subject pool and the difficulty in randomizing a child with an insufficiency fracture to a placebo arm of a study [Phillipi et al., 2008]. In a recent retrospective study Dominguez-Bartmess et al. [2012] showed that oral alendronate treatment failed to produce a significant improvement in bone mineral density in children with low bone density for their age compared with matched, untreated controls, but this result is quite controversial if compared with other studies.
In our report the father had the same mutation but has not a history of fractures. He was treated with hip bone replacement because of Perthes disease. He did not showed signs of osteoporosis.
One could state that improvement of bone density in the child might be due to age; however this seems unlikely because the degree of osteoporosis was severe and symptomatic (a number of spontaneous fractures) before treatment, and normalization of BMD and absence of fracture was achieved in a relatively short period of time.
Although this is a single experience, biphosponate infusional therapy seemed to be effective, both in terms of clinical (absence of new fractures) and mineralomethric parameters (+45% BMD at the lumbar level) (Fig. 2). We suggest that treatment with biphosponate be considered as a possible therapeutic option in case of bone fragility in patients with TRPS.