Fryns syndrome without diaphragmatic hernia, DOOR syndrome or Fryns-like syndrome? Report on patients from Indian Ocean islands
Abstract
We report on six patients (five unpublished patients) from the Indian Ocean islands, with coarse face, cleft lip or palate, eye anomalies, brachytelephalangy, nail hypoplasia, various malformations (genitourinary or cerebral), abnormal electroencephalograms with impaired neurological examination and lethal outcome. Massive polyhydramnios was noted in the third trimester of pregnancy and neonatal growth was normal or excessive. The combination of the features is consistent with the diagnosis of Fryns syndrome (FS) without congenital diaphragmatic hernia. Besides chromosomal aberrations and microdeletion syndrome, differential diagnoses include conditions overlapping with FS such as Simpson–Golabi–Behmel, and conditions with hypoplasia/absence of the distal phalanges such as DOOR syndrome, Schinzel–Giedion syndrome, and Rudiger syndrome. © 2013 Wiley Periodicals, Inc.
INTRODUCTION
Fryns syndrome (FS) [OMIM 229850] is a multiple congenital anomaly syndrome with autosomal recessive inheritance, first described by Fryns et al. [1979]. The classic phenotype includes congenital diaphragmatic hernia (CDH) with pulmonary hypoplasia, craniofacial dysmorphism with cleft lip/palate, brachytelephalangy with nail hypoplasia, and variable internal malformations [Fryns, 1987]. The phenotype of FS was reviewed and diagnostic guidelines were proposed [Slavotinek, 2004; Lin et al., 2005]. Diaphragmatic hernia is a leading feature in FS, present in more than 80% of cases [Hanssen et al., 1992; Slavotinek, 2004], associated with pulmonary hypoplasia and responsible for perinatal death in the majority of patients. No molecular genetic studies have been published and the diagnosis of FS remains clinical. However, it is possible that CDH is over-represented in reported patients, because of enrollment bias due to this malformation. Thus, published patients having FS without CDH have been reviewed [Alessandri et al., 2005].
DOOR syndrome [OMIM 220500] (deafness, onychodystrophy, osteodystrophy, and mental retardation) is a presumed autosomal recessive disorder with no known genetic locus, characterized by coarse face, hypoplasia/absence of the nails and distal phalanges of the hands and feet, neurological manifestations, and sensorineural hearing loss [James et al., 2007].
We report on six patients (of whom five are unpublished patients) over a 10-year period with features of FS, except CDH. All patients were native from Indian Ocean islands (Comoros, Madagascar, and La Réunion Island). We consider they have a heterogeneous condition difficult to delineate, overlapping with FS (without CDH), DOOR syndrome or another Fryns-like condition.
CLINICAL REPORT
Patient 1
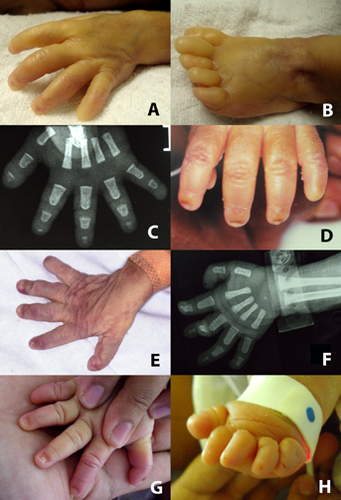
This patient was the first male child of unrelated and healthy Caucasian parents from La Réunion Island. The mother was 28 years old at the time of the pregnancy, and the father 30 years old. Ultrasonographic examination performed at 22 weeks of gestation (WG) revealed a labial cleft, a cystic dilatation of the 4th ventricle, and polyhydramnios. Magnetic resonance imaging (MRI) of the fetal brain at 25 WG showed moderate hypoplasia of the cerebellar vermis. Amniotic fluid chromosome analysis performed at 25 WG revealed a normal 46,XY karyotype. Spontaneous vaginal delivery occurred at 26 WG and 5 days. Apgar score was 2 at 1 min, and 7 at 3 min. The infant was intubated and ventilated immediately after birth. Birth weight was 1.230 g (97th centile), length 37 cm (90th centile), and head circumference 26.5 cm (90th centile). He had a coarse face, abnormal ears, and a unilateral cleft lip and palate. The fifth digits were very short, with absent nails. The terminal phalanges of the toes were hypoplastic. External genitalia were abnormal with a small penis, and bilateral cryptorchidism. Ophthalmologic examination revealed bilateral cataracts. Chest X-rays showed normal diaphragmatic shadows. Skeletal radiographs confirmed absence of distal phalanges of both 5th fingers, marked hypoplasia of the distal phalanges of the other digits. Echocardiography showed a ventricular septal defect. Electroencephalogram performed at 5 days of life showed a burst suppression-pattern with paroxysmal elements. Serial transfontanellar ultrasound scans revealed progressive ventricular dilatation. The baby died at 8 days of life. Array comparative genomic hybridization (array CGH) on extracted fetal DNA in amniotic fluid was normal. The diagnosis of FS without CDH was considered for this patient.
Patient 2
This female patient was the sister of the Patient 1. This second pregnancy was again complicated by polyhydramnios at 28 WG and resulted in a female infant who had CDH. Spontaneous vaginal delivery occurred at 30 WG. Apgar scores were 1 at 1 min, 3 at 3 min. Birth weight was 1.420 g (75th centile), length 38.5 cm (10th centile), and head circumference 27.5 cm (50th centile).The infant was intubated and needed respiratory support. She presented with refractory hypoxemia and died at 24 hr of life, despite mechanical ventilation, inhaled nitric oxide and instillation of surfactant. She had coarse face, abnormal ears, hypertelorism, and cloudy corneae (Fig. 1) Toenails were absent and the fifth digits presented terminal hypoplasia with absence of fingernails (Fig. 2). Chest X-ray showed right-sided diaphragmatic hernia. Autopsy was refused. Array CGH on DNA extracted from blood sample was normal.

Patient 3
This patient was reported in a previous article [Alessandri et al., 2005]. He was the first male child of a nonconsanguineous healthy couple from Mayotte Island, Comoros Islands. The mother was 39 years old at the time of the pregnancy and had 11 healthy children from a former partner. Ultrasonographic examinations performed at 29 and 30 WG revealed polyhydramnios without any fetal morphological anomaly. Fetal growth and movements were normal.
The mother was admitted to the hospital at 30 WG. The weight gain since conception was 13 kg, and marked edema of legs with elevated blood pressure were noted. Caesarean section was performed at 30 WG and 2 days. The 1 min Apgar score was 4, requiring intubation. The baby's weight was 1.675 g (75th centile), and head circumference 29 cm (50th centile). He had a coarse face, poorly shaped ears, hypertelorism, bilateral cloudy corneae and a cleft palate (Fig. 1). The fingers were short with marked hypoplasia of distal phalanges and he had rocker bottom feet. External genitalia were normal. Clinical cardiac examination was normal. Chest X-ray revealed bilateral alveolar syndrome, with normal cardiac and diaphragmatic shadows. Radiological skeletal anomalies were noted: absence of distal phalanges of both 5th fingers with marked hypoplasia of the distal phalanges of the other fingers (Fig. 2), and broad clavicles. Ophthalmologic examination revealed bilateral cataracts. Widened inter-hemispheric and sylvian fissures, with normal appearance of the corpus callosum and median structures of the brain were noted on transfontanellar ultrasonography. Electroencephalogram performed on the 2nd day of life showed marked disruption with absence of physiological features and sharp theta bursts.
The respiratory distress syndrome was treated by mechanical ventilation and intra-tracheal instillation of exogenous surfactant. Respiratory condition progressively worsened with development of refractory hypoxemia and persistence of alveolar syndrome despite repeated instillation of intra-tracheal surfactant at 24th hour of life. The baby died on the 4th day. Necropsy was refused by the parents.
Cytogenetic study of peripheral lymphocytes and skin fibroblasts showed a normal 46,XY karyotype.
Patient 4
This girl was the first child of a mother from Anjouan Island, Comoros Islands. Information about familial history and pregnancy was not available. Spontaneous vaginal delivery occurred at 35 WG and 6 days. Polyhydramnios was present. Apgar score was 10 at 1 min, and 8 at 3 min. Birth weight was 2.490 g (50th centile), length 45 cm (10th centile), and head circumference 32 cm (25–50th centile). The baby had a coarse face, dysplastic and low-set ears, anteverted nares, a depressed nasal bridge, and a cleft palate. The fingers were short, with nail hypoplasia (Fig. 2). A narrow chest, with pectus excavatum was noted. Ophthalmological examination was normal. Skeletal radiographs showed hypoplasia of the distal phalanges of the fingers, and broad clavicles. Chest X-ray was normal. Electroencephalogram performed at 8 days of life showed marked disruption with periods of abnormally interrupted activity, multiple spikes and significant asynchronism.
Abdominal and transfontanellar ultrasounds were normal. Neonatal course was complicated by seizures at 8 days of life, poorly controlled by clonazepam and valproate therapy. After discharge, the baby died at 5 weeks of life, due to inhalation and respiratory distress.
Karyotype on peripheral lymphocytes was normal, 46,XX.
Patient 5
This boy was the second child of healthy, unrelated parents from Madagascar Island. The previous child was healthy. The mother was 26 years old at the time of the pregnancy, and the father 38 years old. Ultrasonographic fetal examination performed at 19 WG revealed left hydronephrosis. At 26 WG severe hydronephrosis and polyhydramnios were noted. Fetal karyotype from amniotic fluid at 19 WG was normal, 46,XY. From 27 WG, massive polyhydramnios was noted. Three therapeutic amniocenteses were performed and one liter of amniotic fluid was removed at each procedure. Serial ultrasonographic examinations revealed ventricular septal defect and micropenis. Spontaneous vaginal delivery occurred at 33 WG and 6 days, with marked dystocia due to the fetal abdominal distension. Apgar score was under 3 at 1 and 3 min. Tracheal intubation, respiratory support and medical resuscitation were initiated, but failed and the neonate died 20 min after delivery. Birth weight was 3.180 g (97th centile), height 46 cm (50th centile), abdominal circumference 37 cm (>97th centile), and head circumference 33 cm (50–75th centile). The neonate had coarse facies, midface hypoplasia, depressed nasal bridge, infra-orbital skin creases, and wide anterior fontanel. Nail hypoplasia was noted on digits 2–5 together with abdominal distension, micropenis and cryptorchidism. Skeletal radiographs showed marked hypoplasia or absence of distal phalanges of all digits (Fig. 2). Autopsy revealed marked left hydronephrosis, and absence of the left ureter. Diaphragm and lung segmentation were normal. The diagnoses of Schinzel–Giedion syndrome or FS without CDH were first considered for this patient.
Patient 6
This female patient was the fifth child of the same Madagascan parents. Ultrasonographic fetal examination performed at 25 WG revealed a unilateral cleft lip, a pyelic dilatation, and massive polyhydramnios. Parents denied amniocentesis for fetal karyotype. Spontaneous vaginal delivery occurred at 39 WG. Apgar score was 2 at 1 min, and 7 at 3 min. The infant was intubated and ventilated 5 min after delivery. Birth weight was 4.470 g (above 97th centile), length 55.5 cm (above 50th centile), and head circumference 36.5 cm (97th centile). He had unilateral cleft lip and palate, hypertelorism, epicanthic folds, flat nasal bridge, and dysplastic ears (Fig. 1). The terminal phalanges, nails of fingers and toes 1–4 presented with marked hypoplasia. Terminal phalanges and nails of the 5th fingers were absent (Fig. 2). Ophthalmologic examination was normal. Radiological skeletal anomalies were noted: absence of the distal phalanges of the toes, and broad clavicles. Hand X-rays were not available. Renal ultrasound showed bilateral hydronephrosis. Cerebral MRI revealed marked hypoplasia of olfactory bulbs. Electroencephalogram performed on the 1st day of life showed marked disruption with absence of physiological features and left temporal spikes. Neurological clinical examination was always abnormal with poor spontaneous movements and reactivity, weakness, absent sucking reflex, and permanently adducted thumbs. Tonico-clonic seizures were observed on the 3rd week of life, controlled by valproate therapy. Electroencephalogram on the 14th day of life showed diphasic frontal notches, slow waves in the anterior regions and temporal theta bursts. The neonatal course was complicated by refractory hypoxemia and pulmonary arterial hypertension, treated by mechanical ventilation and inhaled nitric oxide. The baby was extubated on the 8th day of life and died at home after 21 days, due to respiratory distress and pneumopathy.
Karyotype from peripheral lymphocytes was 46,XX, and array CGH on extracted DNA from blood sample was normal.
Array-Comparative Genomic Hybridization (CGH) Analysis
The microarrays used in this study were the Agilent 60 K oligonucleotide microarray (Agilent Technologies, Santa Clara, CA) with a 60 kb resolution. The technique was performed according to manufacturer's instructions. The scanning was performed with an Agilent G2565 BA DNA microarray scanner using defaults settings. Images were analyzed using Feature Extraction 9.1.3. Raw data text files from this software were then imported for analysis into CGH Analytics 3.3.1. Aberrations were detected with ADM2 algorithm and filtering options of a minimum of 5 probes and abs (log2Ratio) > 0.3. Aberration segments were individually reviewed using GRCh37 (Feb. 2009) hg19 of UCSC.
DISCUSSION
In this report, we present six patients from the Indian Ocean islands, with coarse face, abnormal ears, cleft lip or palate, eye anomalies, and various malformations (genitourinary or cerebral) with lethal neonatal outcome. Massive polyhydramnios was noted in the second or third trimester of pregnancy and fetal growth was normal or excessive. All patients had abnormal neurological examination or abnormal electroencephalograms. Brachytelephalangy and nail hypoplasia were constant findings, often with marked involvement of the fifth digits. G-banded karyotype analyses were normal. The families are not related, and their origin could not be traced to one specific area (i.e., Madagascar). Features of the reported patients are listed in Table I.
| Patient 1 | Patient 2 | Patient 3 | Patient 4 | Patient 5 | Patient 6 | Fryns syndromea | Rudiger syndromeb | Schinzel–Giedion syndromec | DOOR syndromed | |
|---|---|---|---|---|---|---|---|---|---|---|
| Polyhydramnios | + | + | + | + | + | + | 56 % | − | 23% | Common |
| Birth weight | 97th centile | 75th centile | 75th centile | 50th centile | 97th centile | 97th centile | Normal | 97th centile | 50th centile | Normal |
| Coarse face | + | + | + | + | + | + | 17% | + | − | 78% |
| Cleft lip/palate | + | − | + | + | − | + | 75% | + | − | 17% |
| Cloudy corneae/cataracts | + | + | + | − | ND | − | 17% | − | − | Rare feature |
| Brachytelephalangy (fingers) | + | + | + | + | + | + | Major feature | + | + | 100% |
| Hypoplastic/absent nails | + | + | − | + | + | + | 60% | + | Hyperconvex nails | 100% |
| CDH | − | + | − | − | − | − | 96% | − | − | − |
| Cardiovascular malformations | + | ND | − | − | − | − | Frequent feature | − | 43% | 17% |
| Genitourinary malformations | + | ND | − | − | + | + | Frequent feature | + | 91% | 17% |
| Cerebral malformations | + | ND | − | − | − | + | Frequent feature | − | <10% | 67% |
| Abnormal EEG/seizures | + | ND | + | + | ND | + | 4% | + | 70% | 87 % |
| Distal digital hypoplasia (radiology) | + | + | + | + | + | + | Major feature | + | 33% | 100% |
| Lethal course | + | + | + | + | + | + | Major feature | + | Death in infancy | 32% |
| Inheritance | Autosomal recessive | Autosomal recessive? | Autosomal dominant | Autosomal recessive |
Although CDH was absent in five patients, the combination of polyhydramnios, normal, or excessive growth, coarse facies, cleft lip/palate, internal malformations, and distal hypoplasia of fingers and toes was consistent with the diagnosis of FS, according to the current diagnostic guidelines [Slavotinek, 2004; Lin et al., 2005]. Patient 1 had a sib (Patient 2) with features suggestive of FS with CDH, reinforcing retrospective diagnosis of FS proposed for him. Lin et al. [2005] suggested a definition of the Fryns phenotype according to the combination of six criteria based on previously published articles: diaphragmatic defects, characteristic facies, distal digital hypoplasia, pulmonary hypoplasia, characteristic anomalies (polyhydramnios, cloudy corneae, cleft lip/palate, genitourinary, cardiovascular, cerebral malformations), and affected sibs. Presence of four among the six criteria could allow a narrow definition of FS, while presence of three criteria could suggest a broad definition of FS. However, all these features are strongly suggestive of FS (especially terminal digital hypoplasia) if they are associated with CDH. Thus, until now, there is probably an overrepresentation of published patients having FS with diaphragmatic defects, further considering that molecular markers have not yet been identified for this syndrome. Diagnosis of FS in patients without CDH is a challenge given its impact on parental genetic counseling.
Karyotyping is mandatory before considering a diagnosis of FS as several chromosomal aberrations have been associated with phenotype similar to FS. Pallister–Killian syndrome (or tetrasomy 12p) is characterized by a tissue specific mosaic distribution of an additional isochromosome 12p, and shares features with FS (CDH, polyhydramnios, coarse facies, congenital cardiac anomalies, distal limb hypoplasia, and fetal overgrowth) [Doray et al., 2002]. The additional isochromosome 12p is usually identified by FISH on chorionic villi, amniocytes, or skin fibroblasts, rarely in blood lymphocytes. Failure of prenatal diagnosis with chorionic villus sampling or amniocentesis has been rarely reported [Doray et al., 2002], and post-natal exclusion of Pallister–Killian diagnosis by skin fibroblasts culture should be mandatory prior to the diagnostic of FS. Thus, diagnosis of Pallister–Killian has not been completely ruled out for the Patient 4.
Patients with CDH with associated malformations or facial dysmorphism, and normal G-banded karyotypes have been diagnosed as FS and then reclassified after using array CGH and detection of submicroscopic chromosomal aberrations [Slavotinek et al., 2005; Kantarci et al., 2006]. Three main loci for Fryns-like phenotype have been identified: monosomy 15q26 [Slavotinek et al., 2005; Klaassens et al., 2007]; monosomy 8p23 [Slavotinek et al., 2005]; and finally monosomy 1q41q42 [Kantarci et al., 2006; Shaffer et al., 2007]. Array CGH is therefore mandatory before considering a diagnosis of FS. Such molecular studies were not carried out in Patients 3 and 4, and differential diagnosis of microdeletion syndrome must be considered for them.
Some single-gene conditions associated occasionally with CDH overlap with FS, but have a specific clinical pattern allowing distinction from FS. Simpson–Golabi–Behmel syndrome (SGBS) is an X-linked overgrowth syndrome resulting from deletions or mutations in the GPC3 gene. This condition is characterized by macrosomia, distinctive facies, and congenital heart, renal or gastrointestinal malformations. Reported Patients 1, 5, and 6 presented neonatal macrosomia, but some distinctive features of SGBS (supernumerary nipples, postaxial polydactyly, syndactyly) were absent; besides SGBS has an X-linked inheritance with a rarely full-blown expression in female patients, making this diagnosis improbable in Siblings 5 and 6.
In all the reported patients, distal digital hypoplasia was a constant feature. Besides Fryns syndrome, chromosomal aberrations, and microdeletion syndromes, the differential diagnoses include conditions with hypoplasia/absence of the distal phalanges such as Schinzel–Giedion, DOOR, and Rudiger syndromes (Table I). Severe neonatal form of Coffin–Siris syndrome can also be discussed [Coulibaly et al., 2010].
Schinzel–Giedion phenotype comprises facial features (midface retraction, wide fontanels, ocular hypertelorism, deep grooves under eyes, frontal bossing), hydronephrosis, and specific skeletal abnormalities such as sclerotic skull base, wide occipital synchondrosis, and broad ribs. Hypoplastic distal phalanges are present in 33% of the patients [Lehman et al., 2008]. Schinzel–Giedion syndrome was first suggested for Patient 5, but cleft lip/palate present in Patient 6 has never been reported in Schinzel–Giedion syndrome. Inheritance of Schinzel–Giedion syndrome is autosomal dominant, due to heterozygous de novo mutation in the SETBP1 gene [Hoischen et al., 2010]. The occurrence of the same condition in the Siblings 5 and 6 is therefore against the diagnosis of Schinzel–Giedion syndrome, although a dominant disorder with gonadal mosaicism cannot be excluded. In 1971, Rudiger reported a multiple congenital disorder with lethal outcome in two siblings, characterized by coarse facies, cleft soft palate, hydronephrosis with ureteral stenosis, bicornuate uterus in the female, and hypoplasia of the distal phalanges. None of the patients had CDH. Interestingly, for some authors the condition described by Rudiger overlaps with Schinzel–Giedion syndrome [Lehman et al., 2008], or with FS without CDH [Bamforth et al., 1989; Hanssen et al., 1992; Riela et al., 1995; Ramsing et al., 2000; Lin et al., 2005].
Some of our patients fulfilled diagnostic criteria for DOOR syndrome: coarse facies, anteverted nares, hypertelorism, hypoplastic or absent distal phalanges of the digits and toes, and hypoplastic or absent fingernails or toenails. Polyhydramnios is commonly reported in DOOR syndrome. Our patients had also ophthalmological anomalies (cataracts), cleft palate, and cardiac or renal abnormalities less commonly reported in DOOR syndrome [James et al., 2007]. Neonatal course of patients with DOOR syndrome is marked by abnormal neurological examination, feeding difficulties, severe gastroesophageal reflux, aspiration pneumonia, and refractory seizures with sometimes neonatal onset. All those features have been observed in our patients. However, the early lethal course of our patients does not correspond to the natural history of patients with DOOR syndrome [James et al., 2007]. Finally, Coulibaly reported a stillborn male with multiple congenital malformations (complex cardiac anomaly, corpus callosum agenesis, and Dandy–Walker malformation), coarse face, hirsutism, and absence of the nail and distal phalange of the fifth fingers. Severe hypoplasia of the second to fourth fingernails and of the toenails was noted. Karyotype and array CGH were normal. The patient might have a severe form of Coffin–Siris syndrome, an autosomal dominant MCA condition for which minimal clinical criteria are developmental delay, hirsutism, coarse face, and hypoplasia/absence of the fifth digit/toe nails or distal phalanges. Interestingly, authors have considered FS without CDH as differential diagnosis for their patient [Coulibaly et al., 2010].
The nosology of the condition we report is difficult to delineate. The diagnosis of FS is highly probable in Patient 1 with a sibling (Patient 2) having CDH. Patient 3 had incomplete molecular investigations, and submicroscopic chromosomal aberrations cannot be excluded. Patients 4 and 5 had a presumed autosomal recessive disorder overlapping FS and DOOR syndrome.
The gene(s) responsible for FS and DOOR syndrome has/have not been identified and the diagnosis remains clinical. If FS without CDH has been described, the diagnosis of this condition is more difficult, maybe unrecognized. However, the diagnosis of FS must be raised in patients having suggestive features even without CDH, after exclusion of chromosomal aberrations using array CGH. Genetic counseling must be carefully considered with a 25% chance of having an affected child in each subsequent pregnancy. In the future, identification of gene(s) causing FS or DOOR syndrome will clarify some ambiguous diagnoses in mislabeled patients.