Frontonasal dysgenesis, first branchial arch anomalies, and pericallosal lipoma: A new subtype of frontonasal dysgenesis†
How to Cite this Article: Guion-Almeida ML, Richieri-Costa A. 2010. Frontonasal dysgenesis, first branchial arch anomalies, and pericallosal lipoma: A new subtype of frontonasal dysgenesis. Am J Med Genet Part A 152A:2039–2042.
Abstract
We report on two unrelated Brazilian boys with craniofacial anomalies that involve the frontonasal process and the first branchial arch associated with pericallosal lipoma. To our knowledge this condition seems to have been reported only once previously, but may represent a new condition within the group of the frontonasal dysgenesis. Clinical and imaging data, phenotypic evolution, and differential diagnosis are discussed. © 2010 Wiley-Liss, Inc.
INTRODUCTION
Frontonasal dysgenesis (FND) is present in several syndromes that result from the abnormal development of the frontonasal process [Sedano and Gorlin, 1988]. It has been reported together with branchial arch involvement, limb anomalies, pericallosal lipomas, callosal agenesis, and congenital heart defects among other less common congenital anomalies [Gorlin et al., 2001]. The identification of specific subtypes within the FND group of conditions has been considered useful to establish prognosis [Wu et al., 2007]. Here we report on two unrelated Brazilian boys with high and narrow forehead, hypertelorism, downslanted palpebral fissures, broad nose, bilateral preauricular tags, alar clefts, dimple in the columella, cleft lip and palate, and pericallosal lipoma. Despite similarities with the oculoauriculofrontonasal syndrome (OAFNS), the unique facial phenotype led us to consider the possibility that they have a hitherto undefined condition.
CLINICAL REPORTS
Patient 1
Patient 1, male, born in 1982, was the first child of a normal 23-year-old G3P3 mother and her normal and nonconsanguineous 28-year-old husband. Pregnancy was uneventful with no exposure to toxic, traumatic, infectious agents or radiation. Delivery was normal at term. Birth weight was 3,600 g (50–75th centile). Neuropsychological development was delayed: he lifted his head at 5 months, sat without support at 11 months, walked at 18 months, and acquired first words at age 3 years. Examination at 6 years (Fig. 1A,B) showed a weight of 20.5 kg (75th centile), height of 121 cm (90th centile), OFC of 50 cm (<50th centile), ICD 4.0 cm (>97th centile), OCD 8.7 cm (>97th centile). He had mild mental retardation, an irregular frontal hairline, high forehead, long face with hypoplastic lower part of the right hemiface, hypertelorism, wide and abnormally distributed eyebrows, short and downslanted palpebral fissures, hypoplastic lacrimal puncta, high and broad nasal root and bridge, alar nasal cleft at left and hypoplastic nostril and nasal ala at right, dimple in the midline of the philtrum just below the base of the columella, high-arched palate, thin upper lip; low, posteriorly angulated ears, hypoplastic tragus, and bilateral preauricular skin tags. No other cranial anomalies were present. Results of ophthalmological and audiological evaluations were normal. Results of routine blood tests and G-banded chromosomes (550 bands) in peripheral lymphocytes were normal. MRI showed a midline pericallosal lipoma (Fig. 1F,H). The follow-up showed a remarkable change of the phenotype. The face became markedly triangular due to an excessive prominence of the chin (Fig. 1C,E), but the basic clinical signs remained unchanged. Presently he is an active man with hyperactive behavior.
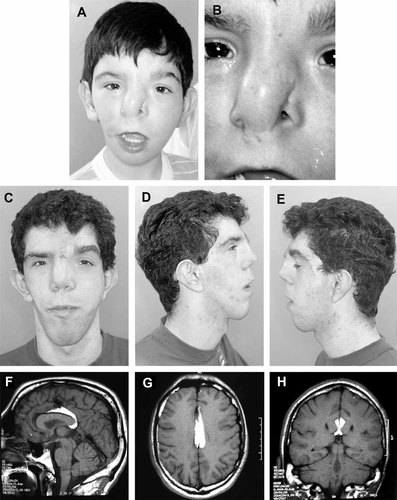
A,B: Face of Patient 1 at age 6 years. C–E: Facial aspect at age 18 years showing the change of phenotype. F–H: MRI of Patient 1 demonstrating pericallosal lipoma.
Patient 2
Patient 2, male, born in 1990, was the first child of a normal 30-year-old G1 mother and her normal and nonconsanguineous 34-year-old husband. Pregnancy was uneventful with no exposure to toxic, traumatic, infectious agents, or radiation. Delivery was normal at term. Birth weight was 2,600 g (3rd centile) and length was 48 cm (3rd–10th centile). Neuropsychological development was normal: he lifted his head at 3 months, sat without support at 7 months, walked at 15 months, and acquired the first words at age 1 year. Examination at 2 years (Fig. 2A,D) showed a weight of 11 kg (10th centile), height of 83.5 cm (10–25th centile), OFC of 47 cm (<50th centile), ICD of 4.9 cm (97th centile), OCD of 9.7 cm (>97th centile). He had normal psychomotor development, irregular frontal hairline, high forehead, asymmetric face, hypertelorism, abnormally distributed eyebrows, epicanthus, downslanted palpebral fissures, hypoplastic lacrimal puncta, high and broad nasal root and bridge, alar nasal cleft at left, and a Tessier 2 cleft at right, a dimple in the midline of the philtrum just below the base of the columella, right cleft lip and palate, thin upper lip, and bilateral preauricular skin tags. No extra cranial anomalies were present. Results of ophthalmological and audiological evaluations were normal. Results of routine blood tests and G-banded chromosomes (550 bands) in peripheral lymphocytes were normal. CT scan showed a midline pericallosal lipoma (Fig. 2H). Despite of the same basic findings, the follow-up showed significant phenotypic differences. The face became thinner and longer with increased asymmetry and prominent chin (Fig. 2E,G). Presently, he has a normal general performance, but is hyperactive.
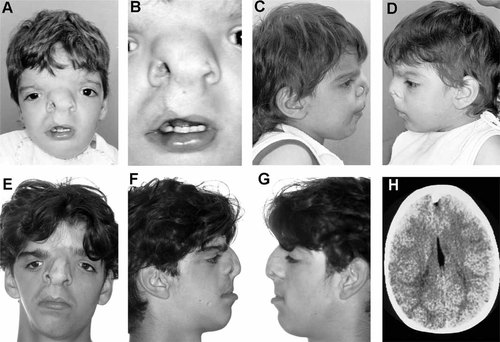
A–D: Face of Patient 2 at age 2 years. E–G: Facial aspect at age 16 years showing change of phenotype. H: CT scan of Patient 2 demonstrating pericallosal lipoma.
DISCUSSION
FND is a rare and heterogeneous condition and encompasses a large group of syndromes involving the frontonasal process [Gorlin et al., 2001]. Several conditions within this group have been delineated, each one with specific characteristics that support a differentiation between them. Frontonasal process involvement, branchial arch defects, and pericallosal lipoma in the patients reported here, seems to represent a new condition. Differential diagnosis includes two FND syndromes with the same developmental field involvement: the syndrome of frontonasal malformation, first branchial arch anomalies, congenital heart defect, and severe central nervous system involvement [Guion-Almeida and Richieri-Costa, 2006] and OAFNS [OMIM 601452; Online Mendelian Inheritance in Man OMIM (TM), 2009]. The first condition was described in a girl, also with tetralogy of Fallot and severe CNS involvement. This girl died at age 80 days. In spite of the similarities of the involved fields, the facial structure, the clinical signs, and the pattern of CNS anomalies permit a distinction between this girl and the patients here reported.
OAFNS combines malformations due to abnormal development of both frontonasal process and branchial arches. Recently, this condition was well characterized as a distinct entity taking into account its overall clinical phenotype when compared with the signs observed in the Goldenhar anomaly [OMIM 164210; Online Mendelian Inheritance in Man OMIM (TM), 2009] and in FND [OMIM 136760; Online Mendelian Inheritance in Man OMIM (TM), 2009; Gabbett et al., 2008]. Intracranial abnormalities were observed in 58% of the cases, a midline lipoma in almost 50%. Considering the present cases, in spite of the clinical overlap with OAFNS patients, the facial involvement and the change of the phenotype with age, supports the differentiation between them. Interesting to note that in a series of patients with nasal clefts, published by Ortiz-Monasterio et al. 1987, one case (Fig. 8A,B) presents the same facial characteristics of the patients here reported. There is no information about an intracranial evaluation.
Thus, we conclude that our patients and the one reported by Ortiz-Monasterio et al. 1987 present a hitherto unidentified condition with hypertelorism, bilateral preauricular tags, alar clefts, dimple in the columella, cleft lip and palate, and pericallosal lipoma. Behavior disturbance and/or mild mental retardation seem to be part of the clinical manifestations.
Acknowledgements
The authors are indebted for CNPq support (grant: 470996/2006-4; 301926/2007-7 to AR-C; and 310659/2006-0 to MLG-A).




