Characterization of the rate, predictors, and thrombotic complications of thrombocytosis in iron deficiency anemia
Sources of support (financial, equipment, drugs): A. Song is the recipient of the American Society of Hematology HONORS Award.
Abstract
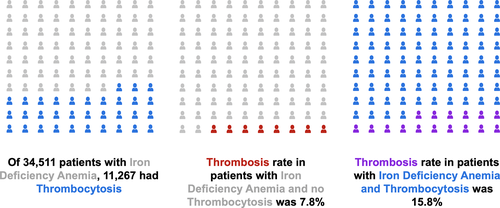
The association of thrombocytosis with iron deficiency anemia (IDA) is well-recognized, but data describing the rate, predictors, and risk of thrombotic complications associated with IDA-related thrombocytosis are limited. We queried an institutional patient data repository containing comprehensive chart data for over 6 million patients to identify IDA patients with and without thrombocytosis and thrombotic events over a 40-year time period (1979 to 2019). Demographics, hematological parameters, thrombosis history, and other medical history were collected. Fidelity of query data was assessed via detailed manual chart review of 700 patients, including confirmation of ferritin and hematologic parameters in addition to temporal and clinical association of thrombocytosis. Our queries identified 36 327 cases of IDA of which 15 022 had thrombocytosis. Following assessment for data integrity, we observed a thrombocytosis rate of 32.6% in patients with IDA. The rate of thrombosis was calculated to be 7.8% in patients with IDA and 15.8% in patients with IDA and thrombocytosis. Platelet mass index at time of peak thrombocytosis was significantly higher than at baseline and was strongly negatively correlated with hemoglobin at peak thrombocytosis. A multivariable model demonstrated a significant predictive relationship between decreasing hemoglobin and increasing platelet count at peak thrombocytosis. In conclusion, we observed reactive thrombocytosis in one-third of IDA patients, and a 2-fold thrombosis risk in patients with IDA and thrombocytosis compared with patients with IDA alone. Given the global burden of untreated and undertreated IDA, adequate IDA treatment may reduce thrombotic complications and associated morbidity and mortality.
1 INTRODUCTION
Iron deficiency anemia (IDA) is the most common cause of anemia worldwide, comprising over 60% of the global anemia burden.1 Clinical manifestations of IDA include fatigue and weakness, pica, neuropsychiatric changes including restless legs syndrome, as well as skin and mucosal changes.2 Iron deficiency anemia occurs due to inadequate iron levels for heme synthesis, precluding adequate hemoglobin content for normal red cell development.3 Thrombocytosis reactive to IDA is a long-recognized hematologic phenomenon.4 Although the underlying mechanism for thrombocytosis reactive to IDA has been largely unclear, recent data has demonstrated that low iron preferentially diverts megakaryocytic-erythroid progenitors (MEPs) towards commitment to the megakaryocytic lineage, partly in addition to altering metabolism, attenuating ERK signaling, and decreasing proliferation of MEPs.5 From an evolutionary perspective, it is thought that thrombocytosis might confer selective hemostatic advantage in the setting of major bleeding, whereas limiting erythroid differentiation could preserve iron stores for other essential functions in DNA synthesis, respiratory chain proteins, and repair enzymes.6, 7
Thrombocytosis can be associated with thrombotic risk in a variety of disease states. Primary thrombocytosis can be observed in myeloproliferative neoplasms which exhibit a significant thrombotic risk secondary to leukocytosis, particularly for those patients who harbor JAK2 mutations.8, 9 Although secondary thrombocytosis is typically not felt by hematologists to be associated with increased thrombotic risk, secondary thrombocytosis may increase risk for venous thromboembolic events (VTEs) in particular contexts such as in patients with cancer10 and critical illness in the intensive care unit.11 In vitro, the platelet count in reactive thrombocytosis exhibits a linearly associated prothrombotic potential as measured by thrombin generation although clinical correlation is varied.12
The clinical significance of thrombocytosis secondary to IDA, if any, is not yet clear. Iron deficiency anemia itself has been shown to be associated with thrombotic events in several small retrospective studies.13-16 Although recent animal studies demonstrated an elevated thrombotic risk in iron deficient mice with thrombus size correlating with platelet count17, whether the elevated thrombotic risk in IDA can be attributed to thrombocytosis has not been clearly elucidated in human analyses. There are numerous case reports describing thrombotic events (particularly in unusual sites) in patients with thrombocytosis reactive to IDA and no other thrombotic risks suggesting a possible relationship.18, 19 Moreover, there is no clear consensus on the rate of thrombocytosis in iron deficiency anemia; given that IDA is so common, the rate and thrombotic risk of thrombocytosis is important to clarify on an epidemiological level.
Therefore, using a large institutional patient data registry, our study aimed to describe the rate of thrombocytosis in patients with IDA, to characterize laboratory characteristics associated with thrombocytosis in IDA, and to elucidate the thrombotic risk associated with thrombocytosis in IDA.
2 METHODS
2.1 Data collection
This study was approved by the Institutional Review Board of Partners Healthcare (approval number 2018P002434). Data for this study was collected from the Partners Research Patient Data Registry (RPDR). The RPDR is a large patient data repository containing comprehensive electronic health record data for over six million patients in the Partners Healthcare system.20 Iron deficiency anemia was defined as a patient with an ICD-9 or ICD-10 code designating a diagnosis of iron deficiency anemia, who also had a hemoglobin measurement below the laboratory reference range for gender, as well as a synchronous documented ferritin value of <30 ng/mL. Thrombocytosis was defined as platelet count above the laboratory reference range (>450 × 109/L). Venous thromboembolic events were defined as deep venous thrombosis (DVT, including mesenteric or cerebral vein thrombosis), superficial venous thrombosis (SVTs), or pulmonary embolus (PE) confirmed on imaging (Doppler ultrasound or cross-sectional imaging). Arterial thrombotic events were confirmed using cross-sectional imaging (strokes), Doppler ultrasound and/or cross-sectional imaging (peripheral arterial thrombosis), or clinical criteria plus biomarker elevation and electrocardiographic changes (myocardial infarction).
Patient repository queries were submitted to identify patients with history of IDA as well as those with history of thrombocytosis using a combination of ICD codes, laboratory values, and enhanced text analyses of ambulatory visit notes (query details are given in the supplementary appendix). Each of these queries was modified to identify individuals with these parameters as well as an ICD code corresponding with a diagnosis of a venous or arterial thrombotic event. Patients with records spanning a 40-year time period from 1979 to 2019 were included. Data returned from the queries included medical record numbers, demographics, diagnosis codes (including risk factors for thrombosis: pregnancy, oral contraceptive or hormone replacement therapy, hypercoagulable conditions [including Factor V Leiden, prothrombin gene mutation, protein C/S deficiency, antithrombin deficiency, antiphospholipid syndrome], obesity, hypertension, hyperlipidemia, diabetes, smoking history, malignancies, infections, inflammatory conditions), encounter histories, transfusion data, and laboratory data (hemoglobin, hematocrit, mean corpuscular hemoglobin concentration, mean corpuscular hemoglobin, mean corpuscular volume, iron, ferritin, iron saturation, total iron binding capacity, reticulocyte count, platelet, mean platelet volume, white cell count, erythrocyte sedimentation rate, C-reactive protein).
Comprehensive quality control of each query was done by performing detailed manual chart review of 700 total patients selected at random. For patients returned in the query for IDA patients with thrombocytosis, the temporal association of the thrombocytosis with the diagnosis of IDA and consistent hematologic and iron study parameters was verified. During this manual review, cases of thrombocytosis that could be attributed to other causes based on clinical encounter notes, including infection, recent surgery/trauma, inflammatory disorders like inflammatory bowel disease or arthritis, myeloproliferative neoplasms, active malignancy and use of thrombopoietic agents (recombinant human thrombopoietin, pegylated megakaryocyte growth and development factor, or thrombopoietin receptor agonists) were excluded. For patients returned in the queries for thrombosis, cases where there was no thrombotic event that was temporally related to the episode of iron deficiency anemia with or without thrombocytosis were excluded. The rates of thrombotic events and thrombosis risk factors from this manual chart review were applied to the full database to generate extrapolated rates of events and risk factors for the entire database.
2.2 Statistical analysis
Based on the validations of query fidelity, the total number of patients with IDA returned in our queries, as well as the number of patients with IDA and reactive thrombocytosis, was determined in order to calculate the rate of thrombocytosis amongst patients with iron deficiency anemia in our cohort. The extrapolated rates of thrombosis and thrombosis risk factors calculated from query validation were compared between patients with IDA alone and those with IDA and thrombocytosis. Pearson correlations and paired t tests were performed to assess relationships between CBC parameters and iron studies at three different time points: Time of IDA diagnosis, time of peak thrombocytosis (highest recorded platelet count with concomitant iron deficiency anemia), and at clinical baseline or resolution of IDA and thrombocytosis. Multivariable linear regression was performed to characterize predictive relationships between degree of thrombocytosis and other laboratory or demographic parameters.
Statistical analysis was performed and graphs for figures were prepared using Stata version 14.2 (StataCorp LLC, College Station, TX) and Microsoft Excel 360 (Microsoft Corp., Seattle, WA).
3 RESULTS
3.1 Rate of thrombocytosis in iron deficiency anemia
The query for patients with iron deficiency anemia identified 36 327 patients of whom the query identified 15 022 cases also with thrombocytosis. Query fidelity rates were calculated to be 95% and 75%, respectively, after quality control and detailed manual chart review. The rate of reactive thrombocytosis in patients with IDA was thereby calculated to be 32.6% (Figure 1).
3.2 Risk of thrombosis attributed to reactive thrombocytosis in iron deficiency anemia
Using database query followed by manual chart review validation, the rate of thrombosis in patients with IDA was calculated to be 7.8%, while the rate of thrombosis in patients with IDA and reactive thrombocytosis was calculated to be 15.8% (Table 1). Both venous and arterial thrombotic events were more common in patients with thrombocytosis compared to those without thrombocytosis (Table 1). The most common thrombotic events were deep venous thrombosis and pulmonary embolism (with or without an accompanying DVT). Mean age at time of thrombosis was 56.5 years for the IDA cohort and 55.4 years for the IDA and thrombocytosis cohort. Among patients with IDA and a thrombotic event, slightly more patients with thrombocytosis had a risk factor for thrombosis compared to those without a risk factor in the extrapolated cohort (Tables 1 and 2).
| Iron Deficiency Anemia N = 34 511 | Iron Deficiency Anemia And Thrombocytosis N = 11 267 | |
|---|---|---|
| Mean Age at Thrombosis | 56.5 y.o. (22.0-94.2) |
55.4 y.o. (20.6-85.5) |
| Sex | 48.6% Male 51.4% Female |
46.5% Male 53.5% Female |
| Rate of Thrombotic Events | 2692 (7.8%) | 1785 (15.8%) |
| Arterial Events | 242 (0.7%) | 162 (1.4%) |
| Venous Events | 2450 (7.1%) | 1623 (14.4%) |
| Deep venous thrombosis | 1760 (5.1%) | 1028 (9.1%) |
| Pulmonary embolism | 449 (1.3%) | 325 (2.9%) |
| Other venous thromboembolism | 242 (0.7%) | 270 (2.4%) |
| Hematologic parameters at IDA diagnosis, median (interquartile range) | ||
| WBC (x109/L) | 8.59 (6.34-9.27) | 8.15 (5.92-9.18) |
| Hemoglobin (g/L) | 9.5 (8.9-10.1) | 9.8 (9.3-10.3) |
| Hematocrit (%) | 30.2 (27.4–31.1) | 31.2 (28.2–31.2) |
| MCV (fL) | 74.0 (70.2-78.6) | 77.9 (73.5-79.2) |
| MCHC (g/dL) | 31.7 (28.2-35.3) | 31.4 (28.4-34.8) |
| Platelets (x109/L) | 303 (223-387) | 358 (254-422) |
| Hematologic parameters at thrombotic event | ||
| WBC (x109/L) | 7.6 (6.13-8.72) | 8.01 (6.47-9.11) |
| Hemoglobin (g/dL) | 10.3 (8.7-11.2) | 9.7 (9.3-10.6) |
| Hematocrit (%) | 32.7 (26.5–34.3) | 30.9 (27.9–32.2) |
| MCV (fL) | 78.4 (72.4-82.2) | 77.0 (72.2-79.9) |
| MCHC (g/dL) | 30.7 (27.9-346) | 32.4 (30.2-36.7) |
| Platelets (x109/L) | 309 (245-401) | 399 (287-492)d |
| Number of patients with risk factors for thrombosis | 1693 (62.9%) | 1244 (69.7%) |
| Arterial risk factorsb | 1404 (51.4%) | 1028 (57.6%) |
| Venous risk factorsc | 893 (37.1%) | 541 (30.3%) |
- a Numbers calculated based on returned database queries and manual chart review of 700 total charts.
- b Risk factors for arterial thrombosis defined as: obesity, hypertension, hyperlipidemia, smoking, diabetes, antiphospholipid syndrome.
- c Risk factors for venous thrombosis defined as: active malignancy, myeloproliferative neoplasm, recent surgery or trauma, pregnancy, hormonal therapy, obesity, hereditary or acquired thrombophilia.
- d Platelet counts were collected at the time of thrombosis during the episode of IDA and associated thrombocytosis, but not necessarily at the exact time point of thrombocytosis.
| IDA without thrombosis | IDA with thrombosis | IDA and thrombocytosis without thrombosis | IDA and thrombocytosis with thrombosis | |
|---|---|---|---|---|
| Pregnancy | 1.74% | 2.86% | 1.19% | 0%a |
| OCP/HRT | 8.70% | 2.86% | 7.14% | 6.06% |
| Hypercoagulability | 9.57% | 11.43% | 5.95% | 9.09% |
| Obesity | 16.52% | 20.00% | 17.86% | 24.24% |
| Hypertension | 27.83% | 31.43% | 26.19% | 33.33% |
| Hyperlipidemia | 20.87% | 31.53% | 16.67% | 18.18% |
| Diabetes | 17.39% | 20.00% | 11.90% | 12.12% |
| Smoking history | 17.39% | 20.00% | 15.48% | 21.21% |
| Any risk factor | 69.57% | 62.86% | 67.86% | 69.70% |
- a Cases with this risk factor were not captured in our sample of 700 manually reviewed cases.
3.3 Relation of hematologic parameters to thrombocytosis
Among patients with IDA and thrombocytosis, hemoglobin exhibited moderate negative correlations with platelet count at time of IDA diagnosis (r = −0.1734, P = .048) and at time of peak thrombocytosis (r = −0.3785, P < .001) (Table 3). Hemoglobin also demonstrated a negative correlation with platelet mass index (calculated as platelet count multiplied by mean platelet volume [MPV]) at time of peak thrombocytosis (r = −0.6888, P < .001). Platelet mass indexes both at time of IDA diagnosis and at time of peak thrombocytosis were significantly higher than at clinical baseline. Multivariable regression including age, sex, WBC, Hgb, platelet count, and MCV demonstrated a significant predictive relationship between decreasing Hgb and increasing platelet count at time of peak thrombocytosis (P < .001). The mean time from IDA diagnosis to normalization of hemoglobin and platelet counts was 1.69 years (95% CI, 1.28-2.10 years). There was no significant correlation between the peak platelet count and the time to resolution of the IDA episode and thrombocytosis (r = 0.1359, P = .337). Mean time from IDA diagnosis (of the relevant episode) to thrombosis was 1.34 years (95% CI, 0.74-1.94 years).
| Ferritin and platelets | ||
| IDA diagnosis | r = −0.3828 | P < .001 |
| Peak thrombocytosis | r = −0.1747 | P = .048 |
| Hemoglobin and platelets | ||
| IDA diagnosis | r = −0.1734 | P = .048 |
| Peak thrombocytosis | r = −0.3785 | P < .001 |
| Ferritin and hemoglobin | ||
| IDA diagnosis | r = 0.2958 | P < .001 |
| Peak thrombocytosis | r = 0.2479 | P = .005 |
| Mean corpuscular volume and hemoglobin | ||
| IDA diagnosis | r = 0.4115 | P < .001 |
| Peak thrombocytosis | r = 0.3494 | P = .048 |
| Platelet mass index and hemoglobin | ||
| IDA diagnosis | r = 0.1491 | P = .519 |
| Peak thrombocytosis | r = −0.6888 | P < .001 |
| Mean corpuscular hemoglobin concentration and hemoglobin | ||
| IDA diagnosis | r = 0.5559 | P < .001 |
| Peak thrombocytosis | r = 0.6586 | P < .001 |
| Mean platelet count | ||
| IDA diagnosis vs clinical baseline | 347 vs 292 | P < .001 |
| Peak thrombocytosis vs IDA diagnosis | 505 vs 347 | P < .001 |
| Platelet mass index | ||
| IDA diagnosis vs clinical baseline | 3400 vs 2858 | P = .006 |
| Thrombocytosis vs clinical baseline | 4892 vs 2836 | P < .001 |
- Relevant relationships of CBC parameters collected at three time points: (1) At time of peak thrombocytosis during an episode of iron deficiency anemia, (2) At time of IDA diagnosis (regardless of platelet count), and (3) At time of clinical baseline (prior to diagnosis of IDA or at resolution of anemia and thrombocytosis).
4 DISCUSSION
To date, several smaller retrospective studies13-16 and numerous case reports18, 19 have suggested a thrombotic risk associated with iron deficiency anemia. To our knowledge, this study is the first to directly assess the thrombotic risk associated with reactive thrombocytosis in iron deficiency anemia. While prior studies have observed increased thrombotic risk with IDA, the potential attribution of that risk to reactive thrombocytosis has not been evaluated. Using large-volume clinical data from a large institutional research database, we estimated a 2-fold increased thrombotic risk associated with reactive thrombocytosis in patients with IDA compared to patients with IDA and no thrombocytosis. The thrombotic events observed mostly included deep venous thromboses and pulmonary emboli; smaller numbers of splanchnic events (eg, portal vein thrombosis) or thromboses in other unusual locations were also observed. Notably, we utilized strict inclusion and exclusion criteria to ensure that only cases with thrombocytosis that could definitively be attributed to the iron deficiency anemia were included; cases with alternative causes of thrombocytosis (and thrombosis) such as inflammatory disease, malignancy, myeloproliferative neoplasms, and infection were excluded. To our knowledge, this was not performed in prior studies.13-16
Rates of thrombosis were high overall in our study: 7.8% in patients IDA and 15.8% in IDA and thrombocytosis. We suspect this can be attributed to the inclusion of both outpatient and inpatient data (for which we did not discriminate); obviously, inpatients are much more likely to either present with or develop a thromboembolic event. Given that we relied on ferritin testing and diagnosis codes alone without use of the transferrin saturation, it is also likely that our queries did not capture all patients in our healthcare system with iron deficiency anemia, but our query method was optimized to identify cases of isolated IDA without other confounding conditions. It is true that some patients with IDA will have a normal or even elevated ferritin owing to underlying inflammation (and these are the patients for whom a low transferrin saturation is required to make the diagnosis), but it was important to exclude such patients in any case as inflammation is a common cause of secondary thrombocytosis and a risk factor for thrombosis.
Accepting the likely artificial elevation in overall thrombotic rates due to inclusion of more morbid inpatients in our analysis, we found an approximately 2-fold increased thrombotic risk in IDA patients with thrombocytosis, compared to those without thrombocytosis. In comparison to other known common risk factors for thrombosis (such as factor V Leiden or use of estrogen-containing oral contraceptives, which each impart an approximately 4-fold increased risk of venous thromboembolism21), a 2-fold temporary risk elevation is relatively minor at the individual level. However, if confirmed in other studies, this modestly increased risk could be profound from an epidemiologic perspective, given that over five million individuals in the United States and approximately 20% of the human population worldwide have IDA at any given time.3 Although more patients with thrombocytosis had a risk factor for thrombosis compared to those without thrombocytosis, the difference was relatively minor.
Recognition of this increased thrombotic risk raises the question of potential low-dose aspirin thromboprophylaxis during thrombocytosis episodes in patients with IDA. We did not evaluate this in our study but expect that this is likely to be of low clinical utility for several reasons. The number needed to treat to prevent one thrombotic event is likely very high given the modestly increased individual thrombotic risk; many patients are iron deficient because of acute or chronic blood loss (ie, menstrual or gastrointestinal bleeding) and thromboprophylaxis might exacerbate this; and the iron deficiency itself is just as easy to correct and should be the focus of treatment. Indeed, the latter point is most important: recognition and prompt treatment of IDA is important for a number of reasons, the potential increased thrombotic risk being just one of many. There are several studies investigating the cost-effectiveness of more proactive diagnosis and treatment of iron deficiency anemia, and our results contribute to the body of knowledge regarding the morbidity and mortality of undiagnosed or undertreated iron deficiency anemia.22-24
Given our study design and aims, we did not re-demonstrate whether patients with iron deficiency anemia with or without thrombocytosis have elevated thrombotic risk compared to healthy patients without iron deficiency anemia as has been reported in the existing literature. Our data do suggest, however, that thrombocytosis contributes to, or is largely responsible for, this increased risk. Many disorders associated with thrombocytosis are also associated with increased thrombotic risk such as malignancy25 and myeloproliferative neoplasms,8 although the underlying mechanism is not well-characterized. It is unlikely to be related to an increase in whole blood viscosity, as thrombocytosis, even when severe, does not appreciably increase viscosity. This has been confirmed in an analysis of patient blood sample viscosity, which found no difference in viscosity between those patient with counts less than or more than 400x109/L in patients with iron deficiency anemia.26 Another possible etiology of elevated thrombotic risk conferred by thrombocytosis is increased platelet hyperreactivity and aggregation. In vitro, platelet count has been shown to exhibit a positive linear relationship with thrombin generation using platelet-poor plasma samples.12 A recent analysis of 57 children with IDA and 48 healthy controls demonstrated that blood samples from children with IDA showed higher tendency to coagulate, as defined by shorter clot formation times and higher mean clot firmness, although the thromboelastography results remained in normal range.27 This may be due to the limited sensitivity of thromboelastography as IDA is associated with a modestly increased thrombotic risk. Relevant to the present study, while the mean platelet count of the IDA samples was higher than that of the control samples, thromboelastography results were not stratified by the presence or absence of thrombocytosis.
A significant strength of our study involves the use of manual chart review of 700 randomly-selected charts to determine event and risk factor rates to then apply to the database, rather than use of administrative or billing codes, which have well-described limitations.28 We suspect that the improved accuracy of manual chart review in adjudicating thrombotic events over use of administrative or billing codes is likely to be substantial. However, our study does have a number of clear limitations. This includes its retrospective, observational nature and the inherent limitations of large database analysis, including the infeasibility to review every chart manually and therefore the need to use a combination of database query and manual chart review to extrapolate event rates for the full database cohort. While we utilized manual chart review of a large number of randomly-selected charts for each query, sampling bias is still possible such that the manually-reviewed charts did not accurately reflect the full database cohort. Multivariable logistic regression to evaluate thrombotic risk accounting for covariates and confounders was not feasible given the inability to collect granular data on each patient in the entire cohort of several thousand patients. There is no established laboratory-based definition for iron deficiency, which necessitated selection of a ferritin cutoff. Lastly, we appropriately excluded patients with inflammatory conditions given the confounding influence of systemic inflammation on the ferritin, but some patients with known inflammatory conditions could have also had iron deficiency, and any such patients were invariably excluded by our methodology.
In conclusion, in a large database study with extensive manual chart review to ensure quality control, we observed a 32% rate of thrombocytosis in patients with iron deficiency anemia which is similar to results of prior small analyses.29, 30 Thrombocytosis was associated with an approximate 2-fold increasein overall thrombotic risk in patients with IDA, including elevations in rates of both venous and arterial thrombosis. While our findings require confirmation in additional studies, given the global burden of unrecognized and undertreated iron deficiency anemia, our findings emphasize the importance of prompt identification and effective treatment of this common hematologic disorder.
ACKNOWLEDGEMENTS
A. Song is the recipient of the American Society of Hematology HONORS Award. H. Al-Samkari is the recipient of the National Hemophilia Foundation-Shire Clinical Fellowship Award, the Harvard KL2/Catalyst Medical Research Investigator Training Award, and the American Society of Hematology Scholar Award.
AUTHOR CONTRIBUTIONS
A. B. Song wrote the first draft of the manuscript and contributed to concept and design, data collection, data analysis, creation of tables and figures, critical writing and revision of the intellectual content, and final approval; D. J. Kuter contributed to concept and design, critical writing and revising the intellectual content, and final approval; H. Al-Samkari contributed to concept and design, data analysis, creation of tables and figures, critical writing and revision of the intellectual content, and final approval.
DISCLOSURES
The authors report no disclosures relevant to the present work. Universal Disclosures: Song: None. Al-Samkari: Consultancy (Agios, Dova, Moderna), Research Funding (Agios, Dova). Kuter: Research funding (Protalex, Bristol-Myers Squibb, Rigel, Bioverativ, Agios, Syntimmune, Principia, Alnylam); Consultancy (ONO, Pfizer, 3SBios, Eisai, GlaxoSmithKline, Genzyme, Shire, Amgen, Shionogi, Rigel, Syntimmune, MedImmune, Novartis, Alexion, Bioverativ, Argenx, Zafgen, Fujifilm, Principia, Kyowa Kirin, Takeda, Platelet Disorders Support Association).