Cup-like blasts in acute myeloid leukemia
Conflict of interest: Nothing to report.
Abstract
A patient with AML with normal karyotype and the cytological pattern of cup-like blasts (CLB) is reported. The typical morphology on Pappenheim stained blood smears is shown. In addition transmission electron microscopy pictures demonstrate impressively the invaginated nuclear pocket compressing the chromatin. Cup-like blasts usually do not express CD34. There is a close relationship of CLB-AML with the molecular aberrations of NPM1 and/or FLT3-ITD.Am. J. Hematol. 90:847–848, 2015. © 2015 Wiley Periodicals, Inc.
A female patient of 87 years with history of weakness and fever was admitted to our department. Blood cell counts were Hb 7.5 g/dl, leucocytes 165 G/l, platelets 72 G/l, mean corpuscular haemoglobin (MCH) 29 pg, mean corpuscular volume (MCV) 86 fl, and lactate dehydrogenase (LDH) was 719 U/l. The hematological diagnosis was an acute myeloid leukemia (AML) in cytology and flow cytometry.
Some cases of AML show blasts with prominent nuclear invaginations (NI), so called cup-like (CLB) or fish mouth blasts 1 due to indentation of the nucleus by bits of cytoplasm. The typical morphology is shown in Fig. 1. The blasts are medium-sized and have moderate cytoplasm with few fine azurophilic granules. The involved nuclear area shows a brighter color than the unaffected chromatin (Pappenheim staining, blood smear).
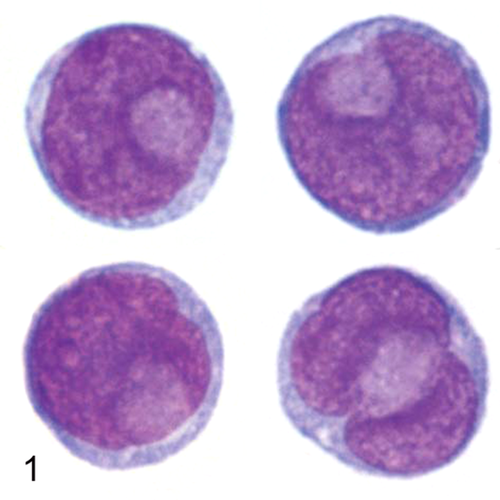
Cup-like blasts (CLB) with typical morphology on blood smear, Pappenheim staining (1,000×).
The transmission electron microscopy (Fig. 2) reveals a collection of mitochondria within the invaginated nuclear pocket partially compressing the chromatin. Besides the CLB, another part of the blast population does not show NI (Fig. 3). The definition of CLB is 1: at least 25% of the nucleus shows the described imprint of the nucleus. To be called CLB-AML, a minimum of 10% of blasts in peripheral blood or bone marrow must reveal the cytological CLB phenomenon 2; other investigators use a cut-off of 5% CLB 3. These blasts had a specific pattern in flow cytometry with CD34-negative blasts but expression of cytoplasmic myeloperoxidase; in addition, the CLB did not express human leukocyte antigen DR (HLA-DR) (data not shown). This expression pattern was typical for CLB-AML 2.
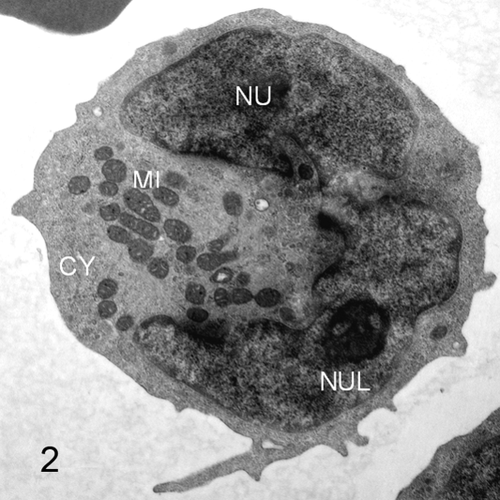
Transmission electron microscopy. CLB with large nuclear indentation by mitochrondria-rich cytoplasm.
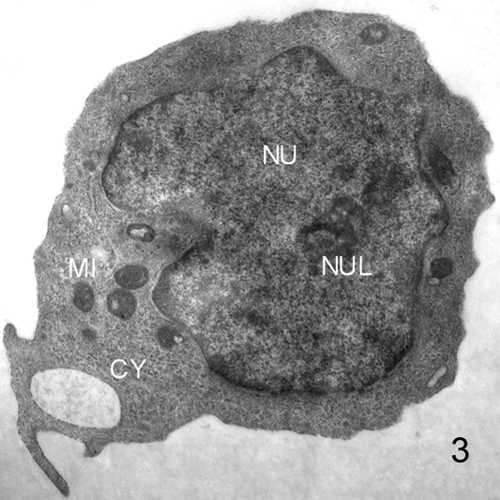
Non-CL blast with monocytic shaped nucleus.
CLB-AML presents with higher leucocyte and blast counts in the peripheral blood and bone marrow compared to non-CLB-AML. Based on the FAB-classification, the majority of cases show morphology of AML-M1 or a monocytic AML. Cytogenetically, a normal karyotype is found 1.
There is a close relationship of CLB-AML with specific molecular aberrations. NPM1-mutation and/or FLT3-ITD individually or in combination are present in >60% of CLB-AML 4 with normal karyotype (NK). The highest presence of CLB is observed if both mutations are detected 5. But CLB appear also in non-NPM1/FLT3-ITD-AML. Therefore, the specificity of CLB as a predictive factor for NMP1-mutation or FLT3-ITD is restricted to 60%. NK-AML patients with NPM1-mutation and without FLT3-ITD have an excellent prognosis with an overall survival at 5 years of 60% 6 similar to AML carrying core-binding factor (CBF) translocation or AML-NK with CCAAT/enhancer binding protein alpha (CEBPA) double mutation.
Patients with AML with NK, NPM1-mutation, and absence of FLT3-ITD can achieve long lasting remissions by conventional chemotherapy without the need for stem cell transplantation (SCT), however there is still no prospective study proving that chemotherapy alone is superior to SCT. Presence of a FLT3-ITD mutation changes the prognosis to an unfavorable outcome and a SCT must be discussed for these patients, especially if the FLT3-ITD ratio is high 7.