Hepatosplenic T cell lymphoma responsive to 2′-deoxycoformycin therapy†
Conflict of interest: Nothing to report
Hepatosplenic T cell lymphoma (HSTL) is a rare condition usually with an aggresssive course and a poor prognosis even after extensive treatment. We describe here a patient who presented with hemophagocytosis. The lymphoma had unusual phenotypic features, an indolent course and responded to 2′-deoxycoformycin therapy as a single agent. We suggest that this therapy be used in further cases as part of the treatment strategy.
HSTL is a rare neoplasm of cytotoxic T cells that was recognized initially in 1990 [1]. Although first described as having a γδ phenotype, a minority of cases were instead found to have αβ receptors [2-4]. The malignant cells in this condition usually express cytotoxic proteins such as TIA1 and granzyme M but are negative for granzyme B and perforin [5-7]. Isochromosome 7q is present in most cases [8, 9]. Somatic TRG@ and TRB@ gene rearrangements are found in both γδ and αβ variants. Biallelic TRG@ rearrangements are specific for γδ cases.
The cells appear as medium-sized lymphocytes with abundant pale cytoplasm; a few granules may be present but these are not prominent. There is a characteristic sinusoidal infiltration in the spleen, liver, and bone marrow. Patients present with marked splenomegaly, hepatomegaly but with no lymphadenopathy [5, 10].
The disease with the γδ phenotype occurs predominantly in young adult males. In the αβ form, the female incidence increases. The course is aggressive [5, 10, 11]. Treatment for this condition is disappointing with a median overall survival of about 1 year even after aggressive regimes of treatment [10, 12].
Our case was a 45-year-old caucasian woman who presented with B symptoms, pancytopenia, and a massive splenomegaly palpable in the abdomen 16 cm below the costal margin without lymphadenopathy. Initially, Hb was 9.6 g/dL, WBC 1.95 × 109/L, absolute neutrophil count was 0.69 × 109/L, and platelets were 66 × 109/L. The LDH (lactate dehydrogenase) was normal and there was no evidence of disturbed hepatic or renal function apart from a slightly raised serum alkaline phosphatase 160 U/L (normal 40–150). A bone marrow aspirate and trephine showed no diagnostic features. Splenectomy was performed 2 months later.
The excised spleen weighed 1.65 Kg. Initial histology findings were of an increase in macrophages with erythrophagocytosis in the red pulp and a diagnosis of hemophagocytic syndrome was entertained.
Post splenectomy, there was an improvement in peripheral blood parameters and the B symptoms resolved. The patient was asymptomatic for 1 year and then started to complain of lassitude and developed an increasing lymphocytosis. These cells were medium to large in size with condensed chromatin, no nucleoli, occasional nuclear projections, abundant pale cytoplasm, and a faint granulation. On flow cytometry, they were positive for CD2, CD3, CD7, CD16, CD56, CD94, CD161, CD158b, and TIA1 and negative for CD5, CD4, CD8, CD57, CD25, HLA DR, CD1a, TdT, CD34, CD52, TCR α/β, TCR γ/δ, and B cell markers. Analysis by PCR (polymerase chain reaction) showed TRB@ and TRG@ rearrangements consistent with a monoclonal T cell population.
A further bone marrow examination and a review of the splenic histology revealed a marked intrasinusoidal infiltration by T cells characteristic of HSTL (Fig. 1). Malignant cells were granzyme B positive. The phenotype otherwise on the histological sections was similar to that of the peripheral blood except for CD56, which was not detected in histological sections and positive in the blood. In situ hybridization with EBER (EBV-encoded RNA) probes did not show EBV (Epstein-Barr virus) association. FISH (fluorescent in situ hybridization) analysis on histological sections and on peripheral blood cells did not show evidence of an isochromosome 7q. Later investigation showed a TCR (T cell receptor) delta rearrangement confirming the γδ origin of the lymphoma.
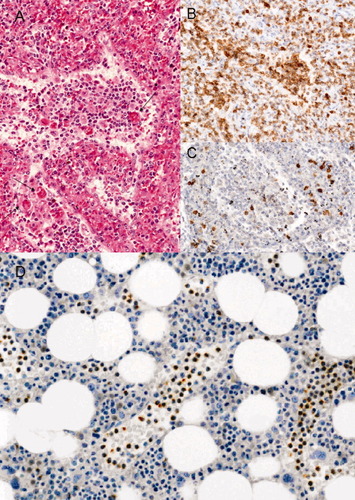
Histopathology. A Spleen: Sheets of medium-sized lymphoid cells in sinuses mixed with histiocytes. Erythrophagocytosis is marked with arrows. H&E stain. Magnification ×100. B Spleen: Lymphoid cells expressing CD3. Magnification ×100. C Spleen: Lymphoid cells not expressing CD5. Magnification ×100. D Bone marrow: Sinusoidal infiltration by small to medium-sized lymphocytes expressing the TIA1 antigen. Magnification ×200. [Color figure can be viewed in the online issue, which is available at wileyonlinelibrary.com.]
At 2 years from the initial presentation, mild elevations of serum SGOT (serum glutamic oxaloacetic transaminase) (55 U/L normal 0–37), SGPT (serum glutamic pyruvate transaminase) (47 U/L normal 0–43), LDH (644 U/L normal 230–480), and alkaline phosphatase (165 U/L normal 40–150) were noted. The white cell count had by then risen to 94.26 × 109/L with an absolute lymphocyte count of 80.37 × 109/L, neutrophils 2.52 × 109/L, Hb 14.0 g/dl, and platelets 185 × 109/L. Lymphocyte morphology appeared unchanged. At this stage, treatment with 2′-deoxycoformycin as a single agent was started (see Fig. 2). This was given at a dose of 4 mg/m2 and caused a rapid cell lysis within a few days accompanied by a nonseptic febrile reaction. Within 1 month liver function tests became normal. Treatment was continued on a 2–5 weekly basis for 10 months, and the patient remained asymptomatic with an absolute lymphocyte count below 2.0 × 109/L. During this time, repeat PCR for TRG@ in peripheral blood lymphocytes showed an oligoclonal population. An attempt to increase the interval between the treatments resulted in an increase in the counts, which again responded to a more aggressive schedule of 2′-deoxycoformycin administration.
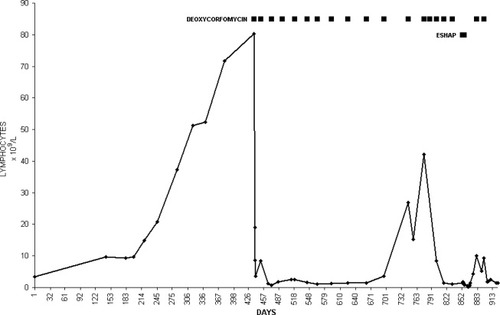
Absolute lymphocyte count and response to therapy.
It was decided to proceed to allogeneic stem cell transplantation. Prior to this combination, chemotherapy with ESHAP (etoposide, methylprednisone, cytarabine and cisplatin) was administered to try to reduce the bulk of malignant cells. This treatment caused profound pancytopenia but lymphocytosis returned within 3 weeks. Further therapy with 2′-deoxycoformycin was again successful in controlling the lymphocytosis.
High dose therapy with BEAM (BCNU, etoposide, cytarabine, melphalan) was then administered followed by allogeneic stem cell transplantation from an HLA (human leukocyte antigen) compatible sibling. She died of acute graft versus host disease 2 months after transplantation and 43 months from the date of initial presentation.
An association with hemophagocytosis and HSTL has been described before [13] and the two conditions may be difficult to differentiate [14].
The indolent course of this patient is unusual for HSTL which is usually aggressive, only a few more chronic courses have been described [15].
The histopathological features of preferential sinusoidal infiltration in the spleen and bone marrow were in favor of HSTL, but there were unusual phenotypic features, in particular, granzyme B expression and a lack of isochromosome 7q. The TCR silent phenotype was also unusual although TRG@ and TRB@ rearrangements were demonstrated. Single cases of this have been previously reported sometimes related with cytological progression over time [1, 10]. In agreement with previous findings [16], there was coexpression of several NK markers including CD16, CD56, CD94, CD161, KIR (killer immunoglobulin-like receptor), CD158b, and TIA-1.
The use of 2′-deoxycoformycin has been reported in five patients with HSTL and shown to have cytotoxic activity. Its efficacy has been supported by in vitro studies [17]. The response here as a single agent was dramatic with a complete although temporary clearance of peripheral lymphocytosis and normalization of the liver abnormalities. She even responded to a further two courses of treatment before eventually succumbing to complications following allogeneic transplantation. The effect of 2′-deoxycoformycin was superior to combination therapy with ESHAP. This case supports the activity of 2′-deoxycoformycin in HSTL, which was superior to combination chemotherapy that is used in high-grade lymphomas. It should be considered as initial therapy for this condition.
References
Michael Bennett*, Estella Matutes , Philippe Gaulard , * Department of Haematology, Ha'Emek Medical Centre, Afula, Israel, Department of Haematology, The Royal Marsden Hospital, London, United Kingdom, Department of Pathology, Henri Mondor Hospital, Paris, France.