Right inguinal metastasis from hepatocellular carcinoma
Abstract
Inguinal hernias are common diseases, but malignant lesions in groin hernias are rare; metastatic hepatocellular carcinoma (HCC) in the hernia sac is extremely rare. We report a 72-year-old man who had advanced stage HCC with portal vein invasion and multiple metastatic lymphadenopathies. He presented a painless palpable mass in the right groin. Computed tomography scan showed a contrast-enhanced soft tissue mass (2.8 cm in size) at the right herniated inguinal sac. Tumor excision and hernia repair were performed, and the histopathological examination revealed metastatic HCC. After being stabilized from surgery, the patient received combination therapy with sorafenib and nivolumab; however, he still died of rapid tumor progression and liver decompensation 1 month later. This case raises clinical awareness of unusual extrahepatic metastases of HCC, especially for patients at an advanced tumor stage.
1 INTRODUCTION
Hepatocellular carcinoma (HCC) accounts for the majority of primary liver cancers and is the fourth leading cause of cancer-related deaths worldwide.1 Despite the promotion of regular surveillance and hepatitis B vaccination, a large number of cases are still at an advanced stage with macrovascular invasion or extrahepatic metastasis.2 Extra-hepatic metastases of HCC are often observed in lungs, lymph nodes, bones, adrenal glands, and the brain.3 However, some unusual metastatic sites might be disregarded and would lead to misdiagnosis in clinical practice.
2 CASE REPORT
A 72-year-old man living in the United States had a medical history of chronic hepatitis B for around 40 years, but did not take any antiviral agents or engage in regular surveillance for HCC. He underwent bilateral hernioplasty 12 years ago. In May 2019, he had a medical exam for a persistent poor appetite and a new palpable mass at right upper quadrant of the abdomen. A large hepatic tumor was found by sonography; so he returned to Taiwan and presented at our hospital for further evaluation and management. The serial examination revealed an acceptable liver reserve at Child-Pugh class A, a high serum level of alpha-fetoprotein (AFP) to 9067.29 ng/mL, a low titer of hepatitis B surface antigen (1.12 IU/mL), nonreactive hepatitis B e antigen, a low serum HBV viral load (HBV DNA: 75 IU/mL) and nonreactive anti-hepatitis C antibody. The dynamic contrast-enhanced computed tomography (CT) scan disclosed a poorly enhanced confluent mass (10.3 × 9.5 × 6.2 cm), mainly at the posterior segment of right hepatic lobe, with invasion of right portal vein and right hepatic vein as well as multiple enlarged lymph nodes at hepatic hilar, retrocaval, and celiac areas (Figure 1A,B). After tumor biopsy and pathologic diagnosis of HCC, he received selective internal radiation therapy with Yttrium-90 microspheres (SIRT-Y90) for HCC and co-administration of self-paid anti-viral therapy with entecavir to reduce the possibility of HBV reactivation during anti-cancer treatment.
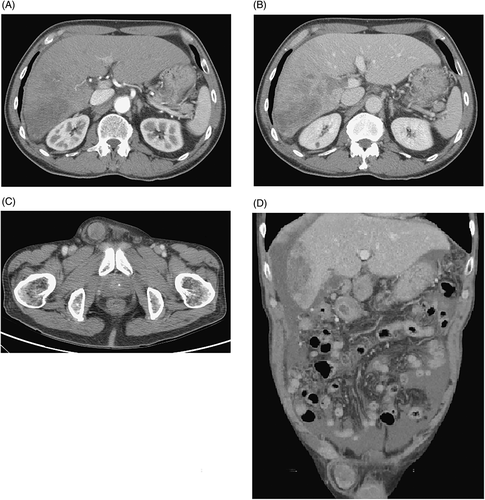
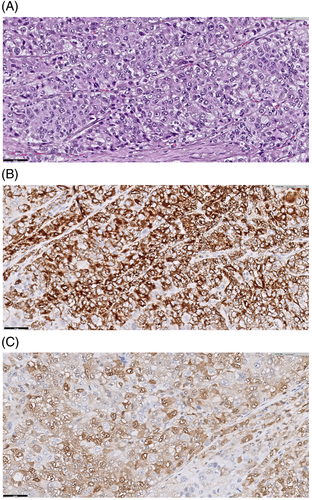
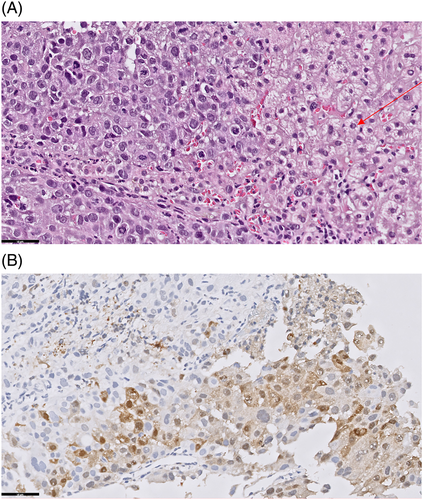
One month later, the patient presented with a newly found, painless, and palpable mass at the right groin. The follow-up abdominal CT scan showed progressive disease with enlarged lymphadenopathies, peritoneal seeding, and a 2.8 cm soft tissue mass at the right herniated inguinal sac with mild contrast enhancement at arterial phase and wash out at venous phase (Figure 1C,D). The following AFP level also increased to 10 000.63 ng/mL. Thereafter, excision of the inguinal mass with hernia repair was arranged, and only a tumor mass but without other herniated organs was observed in the hernia sac intraoperatively. Histologically the mass showed aggregates of neoplastic cells with abundant eosinophilic cytoplasm and centrally located nuclei, arranged in a solid or trabecular structure (Figure 2A). The tumor cells expressed hepatocyte paraffin-1 (HepPar-I) and arginase-1 (Arg-1) immunohistochemically (Figure 2B,C). Morphologically, it resembled the previously obtained intrahepatic HCC (Figure 3A,B) that could be consistent with a metastatic HCC. The tumor did not adhere to the spermatic cord; and no lymph node tissue, large intestine or small intestine could be identified in the hernia sac.
After stabilization from surgery, he received combination therapy with sorafenib (400 mg twice daily) and nivolumab (2-3 mg/kg, every 2 weeks) for progressive advanced HCC. However, he died of rapid tumor progression and liver decompensation 1 month later. This case report was approved by the Institutional Review Board of the Taipei Veterans General Hospital (IRB numbers: 2020-12-010AC).
3 DISCUSSION
Extrahepatic metastases have been reported to occur in 14.0% to 36.7% of HCC patients,4 and would develop in 13.5% of patients presented with intrahepatic HCC during a median follow-up of 21 months.5 Patients with more advanced tumor stages at diagnosis are more likely to develop extrahepatic metastases. A previous retrospective study declared that 73.8% of patients with extrahepatic metastases had intrahepatic HCC staged at T3 or T4 according to the TNM classification.5 In addition, a higher serum level of AFP, larger tumor size, or vascular invasion are also strongly associated with extrahepatic metastasis of HCC.6 Regarding the case presented in this report, the large confluent tumor mass (more than 10 cm in size) with macrovascular invasion and a high AFP level contributed to a remarkably higher risk of development of extrahepatic metastasis.
The lung is the most common metastatic site of HCC. Screening tests for lung metastases should be performed regularly for HCC patients because of its high probability of development and few symptoms presenting when the size is small.5 In contrast, bone metastases (the top three metastatic sites of HCC) often cause severe pain and a deteriorated quality of life that could be clearly identified by the patients.5 Metastasis of HCC in the groin region is extremely rare; and only two cases have been reported till now.7, 8 Although it is not causing much pain for our patient, the metastatic HCC at groin was easily observed due to its apparent bulging. However, malignant tumors within the inguinal hernia sac were rare and the reported incidence was only 0.4% to 0.5% among the cases with excision.9 It could be easily misdiagnosed as hernia or other reproductive organ disorders. Precise evaluation of newly developed groin lesion is very important and necessary, especially in patients with advanced HCC who are at high risk of extrahepatic metastasis.
Extrahepatic metastasis of HCC may cause a diagnostic problem because it may show a variety of histologic patterns and can mimic plenty of malignant or nonmalignant tumors. The markers including Arg-1, HepPar-1, glypican-3 (GPC-3), and AFP are suggested to differentiate HCC from non-HCC in extrahepatic metastasis, because of their optimal sensitivity and specificity, especially in poorly differentiated lesions.10 In this case, the histopathological characteristics of right inguinal mass were similar to that of primary HCC, which was diagnosed on the microscopic presentation of large and polygonal cells arranged in a trabecular pattern. In addition, the tumor cells were positive for Arg-1 and HepPar-I immunohistochemically, which have been reported as reliable markers for HCC.10 In combination with clinical and pathological features, the inguinal mass was diagnosed as metastasis from HCC, different from the other primary tumor.
According to the conventional treatment strategy for solid tumors, locoregional therapies were not effective to patients with metastatic lesions, because the tumor cells are considered to spread systemically. From the vantage point of reduced tumor burden or relief of symptoms, locoregional therapy to the target lesion may be acceptable when the metastatic mass accounts for the major portion of tumor volume, or contributes to the patients' major symptoms. The previous study also indicated that resection of metastatic lesions or locoregional therapy would produce a satisfactory local response and improve quality of life.3 Regarding our patient, excision of the inguinal mass with hernia repair was arranged not only for confirming the diagnosis, but also for symptom relief.
Systemic therapies with sorafenib or lenvatinib are the first line treatment for patients with advanced HCC. Immunotherapy with immune checkpoint inhibitors, including nivolumab, pembrolizumab, and atezolizumab provides promising tumor response and have therapeutic roles in HCC patients who are intolerant to, or have progressed under approved tyrosine kinase inhibitors.11 Synergistic benefits of combination therapy for advanced-stage HCC have also been explored. Recent clinical trials suggested that combination treatment, such as atezolizumab plus bevacizumab, lenvatinib plus pembrolizumab, or nivolumab plus ipilimumab could bring about a promising tumor response.11 According to the real-world data in Taiwan, a significantly better tumor response was observed in patients who received combination therapy compared to monotherapy with immune check-point inhibitors.12 For our patient, we prescribed combination therapy with sorafenib and nivolumab after he stabilized from the excision operation of right inguinal tumor. Unfortunately, he still died of rapid tumor progression and liver decompensation.
We discussed a rare case of metastatic HCC in the inguinal hernia sac. The clinical features of extrahepatic metastases should be precisely evaluated, particularly for the patients with advanced HCC and higher risk of developing distant metastases.
CONFLICT OF INTEREST
The authors declare no conflict of interest.