Comparison of two different techniques in emergency surgery of colon diverticulitis: Hartmann's procedure and resection with primary anastomosis
Abstract
Colon diverticula may require emergency or elective surgery depending on its complications. Our aim is to compare the Hartmann's procedure and resection with primary anastomosis in the patients with colon diverticulitis and to demonstrate the surgical approach of our clinic. Patients were evaluated retrospectively who were operated for colon diverticulitis between January 2010 and January 2020. The patients who underwent emergency surgery for left colon diverticulitis were divided into two groups as patients with primary anastomosis resection (group 1) and Hartmann's procedure (group 2) and the groups were compared. In the aspect of the development of complications there was no remarkable difference between the groups (P = .56). Postoperative early mortality rate was similar in two groups (P = .12). According to the Hinchey classification, 31.7% of the cases were stage I, 9.8% were stage II, 31.7% were stage III, and 26.8% were stage IV. There was not a distinction in morbidity and mortality rates between Hartmann's procedure and resection with primary anastomosis. The best surgical approach should be determined by considering the operation to be performed, the patient's preferences, clinical status, and the predicted results of the surgical treatment of perforated diverticulitis.
1 INTRODUCTION
Diverticulosis is common in developed countries and western societies. The incidence of diverticulosis increases with age.1 Intra-abdominal abscess, purulent, or fecal peritonitis may occur in 15% to 25% of patients with acute diverticulitis.2 Although most of the diverticulitis attacks are relieved with antibiotherapy, emergency surgery is required in 10% to 20% of these patients. It is one of the major causes of emergency colostomy and segmental colon resection.3 Hartmann's procedure is performed in most of the patients with perforated diverticulum.4 However, different surgical procedures are discussed because of the patients bowel continuity could not be achieved due to difficulties in closing the end colostomy.5 Alternatively, sigmoid resection with primary anastomosis (with or without ileostomy) and laparoscopic lavage procedures can be applied.6, 7 In this study, we revealed clinical presentations of the operated patients with diverticulitis and the surgical approach of our clinic.
2 METHODS
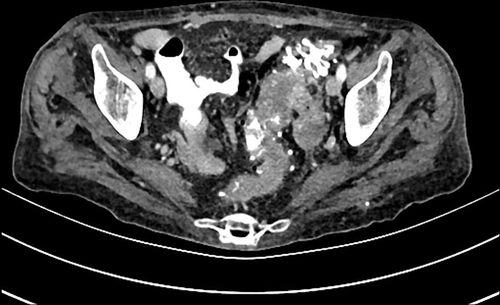
The cases were evaluated retrospectively which was operated for colonic diverticulosis and diverticulitis between January 2010 and January 2020. The exclusion criteria were previous sigmoidectomy and previous pelvic radiotherapy history. Only 64 patients who were operated emergency for diverticulitis in the left colon and sigmoid colon were included in the study. The patients who underwent emergency surgery for left colon diverticulitis were divided into two groups as patients with primary anastomosis resection (group 1) and Hartmann's procedure (group 2) and the groups were compared. Abdominal tomography of the cases was evaluated and Hinchey classification was made. Patients were compared due to their age, gender, location of diverticulum, Hinchey classification stage, duration of operation, operation to be performed, postoperative complications, and early postoperative mortality. Retroperitoneal abscess, wound infection, stoma retraction, and evisceration were evaluated as complications.
2.1 Procedures
In the Hartmann's procedure, transection was made from the proximal of the rectum and this part was closed as a stump. End colostomy was performed after resection of the diseased segment. The distal transection margin for sigmoidectomy with primary anastomosis was on the proximal rectum and the proximal margin was determined from the area where diverticulitis ended.
2.2 Statistics analyses
The computer software used for biostatistical analysis was Statistical Package for the Social Sciences (SPSS 21 Inc., Chicago, IL). Categorical variables were presented as frequency (percentage), and continuous variables were reported as mean ± SD. Differences in patients' characteristics between group 1 and group 2 were examined by Pearson's chi-square test for categorical variables, and by Mann–Whitney test and for numerical variables.
3 RESULTS
Eighty-two patients had undergone surgery for diverticulitis. The average age of 82 patients included in the study was 64.4 ± 15.2 (46.3% male, 53.7% female). Emergency surgery was performed in 80.4% of the cases (66 patients) and elective surgery in 19.6% (16 patients). Most common localization for diverticula was left colon. 87.8% of diverticula were found in left colon (73.2% and 14.6% in sigmoid and descending colon, respectively). There was no significant difference between the groups according to complication development (P = .56). The average operation time was same in both groups (P = .62). The length of hospitalization was seemed high in group 1; there was statistically difference (P = .03). Between two groups, postoperative early mortality rate was indifferent (P = .12). According to the Hinchey classification, 31.7% of the cases were stage I, 9.8% were stage II, 31.7% were stage III, and 26.8% were stage IV (Table 1). 75% of the emergency operated cases were stage III and stage IV (Figure 1).
| Characteristics | n (%) |
|---|---|
| Sex | |
| Female | 44 (46.3%) |
| Male | 38 (53.7%) |
| Hinchey | |
| Stage I | 26 (31.7%) |
| Stage II | 8 (9.8%) |
| Stage III | 26 (31.7%) |
| Stage IV | 22 (26.8%) |
| Location | |
| Caecum | 4 (4.9%) |
| Ascending colon | 6 (7.3%) |
| Descending colon | 12 (14.6%) |
| Sigmoid colon | 60 (73.2%) |
| Complication | |
| Retroperitoneal abscess | 2 (2.4%) |
| Wound infection | 4 (4.9%) |
| Stoma retraction | 2 (2.4%) |
| Evisceration | 2 (2.4%) |
| Surgical emergency | |
| Yes | 66 (80.4%) |
| No | 16 (19.6%) |
| Age (years) | 64.4 ± 15.2 |
| Postoperative stay (days) | 9 ± 6 |
| Operation time (min) | 140 ± 60 |
4 DISCUSSION
Diverticular disease of the colon is more common in societies with western lifestyle and nutritional properties.8 The prevalence of diverticulosis increases with age and it is estimated to be 5% in the 40 ages and it can increase up to 80% in older than 80 years.9 In accordance with the literature, the average age of our cases was 64.4 ± 15.2 years and 71% were over the age of 65.
Diverticulitis perforation is graded according to the Hinchey classification; abscess formation is classified as Hinchey I or II, purulent peritonitis as Hinchey III, and fecal peritonitis as Hinchey IV.9 More than 70% of patients with acute diverticulitis do not develop abscess or perforation. Approximately 20% of patients has a localized abscess in the pericolic (stage I), pelvic, or retroperitoneal area (stage II). Almost 6% of them may develop perforation and generalized peritonitis (stage III and stage IV) and it can be required emergency surgery. More than 93% of stage I diverticulitis and 70% of stage II diverticulitis are known to relieve with medical therapy.10 In our study, elective surgery was performed after patients had repeated attacks with stage I or stage II diverticulitis who were given medical treatment. According to the Hinchey classification, 31.7% of the cases were stage I, 9.8% were stage II, 31.7% were stage III, and 26.8% were stage IV. Stage III and stage IV diverticulitis accounted for 75% of emergency operated cases.
Diverticular localization is different in patients from Western and Asian countries. In western countries patients, more than 90% of diverticula are found in sigmoid colon. In patients from Japan, 70% of diverticula located in the right colon.11 While right colon diverticula are more common in middle aged patients, diverticula commonly found in the left colon and frequency of diverticula increase with age in the entire colon.10 In 87.8% of our cases, diverticula were in the left colon (73.2% and 14.6%, sigmoid and descending colon, respectively), 4.9% in cecum, and 7.3% in the ascending colon. As mentioned in the reports, the patients with left colon diverticula were older than the others.
In case of developing purulent or fecal peritonitis after perforated diverticulitis, emergency operation is performed routinely. In many surgeries, the Hartmann's procedure is a preferred option because it prevents anastomosis leakage.12 The Hartmann's procedure was performed in 78% of our cases. In some studies, sigmoidectomy with primary anastomosis was suggested equal to the Hartmann's procedure in terms of postoperative mortality and morbidity.13, 14 Also in our study, there was not seen any difference in complication development between the groups (P = .56) (Table 2). However, we think that we cannot be sure of the anastomosis safety in an environment with peritonitis; we prefer the Hartmann's procedure especially in elderly patients with comorbidity.
| Variables | Hartmann's procedure group (n = 50) | Primary resection with anastomosis group (n = 14) | P value |
|---|---|---|---|
| Age | |||
| Mean age | 68.7 | 62.7 | .20 |
| Gender | |||
| Male | 48 (24) | 57 (8) | .54 |
| Female | 52 (26) | 43 (6) | |
| Hinchey stage | |||
| I-II | 20 (10) | 43 (6) | .08 |
| III-IV | 80 (40) | 57 (8) | |
| Location | |||
| Sigmoid | 92 (46) | 57 (8) | .005 |
| Descending | 8 (4) | 43 (6) | |
| Complication | |||
| Yes | 12 (6) | 14.2 (2) | .56 |
| No | 88 (44) | 85.8 (12) | |
| Postoperative stay (days) | 9.5 ± 6.9 | 11 ± 3 | .44 |
| Operation time (min) | 120.2 ± 56 | 137.1 ± 30 | .62 |
| Mortality | |||
| Yes | 8 (4) | 7 (1) | .12 |
| No | 92 (46) | 93 (13) | |
In a systematic review it was reported that according to the duration of operation, any difference was not found between in patients who underwent resection with primary anastomosis and the Hartmann's procedure.15 In our study, the mean operation time was almost same in both groups (P = .62). The length of hospitalization has been reported to be similar in both patients group.16 In our study, we found same results as reported (P = .44).
A study of Acuna et al.5 reported that postoperative complications were same between the Hartmann's procedure and resection with primary anastomosis, in a meta-analysis. In another meta-analysis, study of Vasilis et al.17 found that complications such as postoperative wound infection, abscess, and peritonitis were less in the resection with primary anastomosis group. In our study, although the complications were more common in group 2, there was no statistically difference between groups (P = .56). Our complication rate was 12.5%. Wound infection developed in two patients, intra-abdominal abscess in two patients, colostomy retraction in two patients, and evisceration in two patients.
In generalized peritonitis, such as Hinchey III and Hinchey IV, mortality may increase up to 14%.18 There are publications reporting that mortality rates are similar between two groups.5, 12 In another study, it was stated that resection with primary anastomosis reduces mortality. In our study, our mortality rate was 7% (five patients). Mortality was not different statistically between the two groups (P = .12).
The limitations of the study are the small number of patients and the comparison of the surgical technique in the left colon diverticula which were operated only in emergency.
As a result, short-term morbidity and mortality was not changed between Hartmann's procedure and resection with primary anastomosis techniques. The best surgical approach should be determined considering the operation to be performed, the patient's preferences, clinical status, and the predicted results of the surgical treatment of perforated diverticulitis.
CONFLICT OF INTEREST
The authors declare no conflict of interest.
AUTHOR CONTRIBUTIONS
Study conception and design of study: Mustafa Şentürk and Abdulkadir Çelik. Acquisition of data: All authors. Analysis and interpretation of data: Mustafa Şentürk and Mehmet Aykut Yıldırım. Drafting of manuscript: Mustafa Şentürk and Mehmet Metin Belviranl.