Development of acrocyanosis associated with pain and increased creatinine level in histoplasmosis patient: Medication therapy
1 INTRODUCTION
Amphotericin B is a potential anti-fungal antibiotic; it is a polyene and shows action on many species of fungi. It is mainly used in life-threatening fungal infections and has evidence of producing nephrotoxicity when used in high doses; hence its use is limited. It also shows many dose-dependent adverse effects; allergic reactions, nausea and vomiting, and an imbalance in electrolytes are other adverse reactions. We report a case of development of acrocyanosis and increased serum creatinine levels on the use of amphotericin B. We describe the rare complications and evaluate the risk factors. Anisodamine was used to treat the acrocyanosis and pain.
2 CASE REPORT
A 70-year-old man was admitted to hospital due to histoplasmosis. The patient's past medical history included senile degenerative valvular heart disease, alteration in ventricular contractions, and anemia. He had not previously had any other pain, acrocyanosis, or allergies to food, drugs, or pollens. His personal history revealed alcohol and smoking habits for 40 years, which he had ceased 2 years previously. He had experienced histoplasmosis previously and had been treated with itraconazole, voriconazole, and caspofungin acetate successfully a year previously; the oral solution of itraconazole had been prescribed on discharge 9 months previously. In the Pulmonology Department, the patient now reported week-long pain in the right back and chest side, respectively; he also reported that he had stopped taking the oral solution of itraconazole 3 months previously. The vital signs of the patient are presented in Table 1.
| S. no | Parameter | Value |
|---|---|---|
| 1 | Blood pressure | 130/90 mm Hg |
| 2 | Temperature | 36.5°C |
| 3 | Heart rate | 78 beats per min |
| 4 | Respiratory rate | 20 breaths per min |
There was no wheezing and crackles were audible with both lower lungs. The fifth-level muscle strength of both the upper and lower limbs was graded and the physical examination did not reveal any disability or abnormality. Computed tomography (CT) of the thorax showed infection associated with peripheral access in three to five thoracic vertebrae, causing the compression of the spinal cord (Figure 1). Lung CT showed a high-density shadow, which indicates pleural thickening, and encapsulated effusion on the left side (Figure 2). The patient also suffered from prostate calcification and two renal cortical cysts, which were detected through the ultrasound scan. Lab investigations revealed C-reactive protein (CRP) of 98.5 mg/L and creatinine clearance of 39 mL/min; and the complete blood count revealed: a platelet count of 225 × 109/L (normal range: 100-300 × 109/L), a white blood count of 7.2 × 109 L (normal range: 4-10 × 109/L), and neutrophils of 68% (normal range: 47%-77%). The liver function tests revealed a total bilirubin of 7.4 μmol/L (normal range: 1.8-25 μmol/L), alanine aminotransferase of 16 U/L (normal range: 7-40 U/L), aspartate aminotransferase of 24 U/L (normal range: 8-40 U/L), blood urea of 7.9 (normal range: 1.8-7.2 U/L), and serum creatinine of 99 μmol/L (normal range: 45-135 μmol/L).
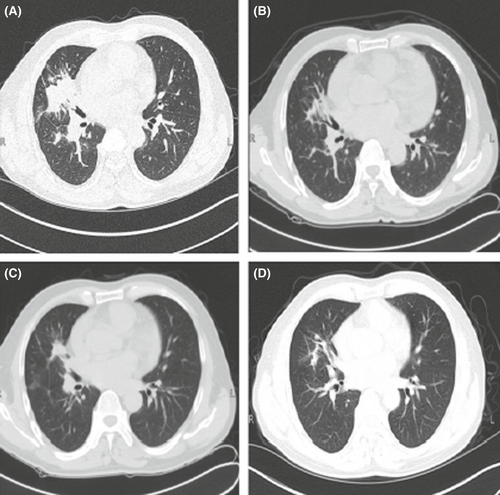
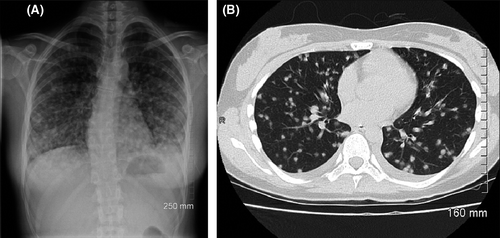
The patient was then admitted to the Pulmonology Department and he received intravenous (IV) cefepime 2 g for 12 hours in divided doses for the pulmonary infection. The treatment regimen also included IV mannitol 125 mL, oral alendronate sodium 70 mg once per week, and loxoprofen 60 mg twice a day. The same treatment regimen was followed to 8 days and the patient had no response to the regimen. On the 9th day, the patient complained that he had a severe pain on the right chest side. His CRP level was 157 mg/L; the loxoprofen was discontinued, and then IV tramadol was administered 0.1 g daily. A year previously, he had suffered from histoplasmosis, which was confirmed with biopsy on the right lung and scapula. As he was not responding to the cefepime, on the 12th day it was replaced with amphotericin B to treat the histoplasmosis. The dose was started at 10 mg on Day 1, and then it was increased to 15 mg on Day 2, 30 mg on Day 3, 60 mg on Day 4, 120 mg on Day 5, and 150 mg on Day 6. On the 15th day, the patient showed decreased CRP of 33 mg/L; however, by the 19th day, the patient had developed cyanosis and pain on both the upper and lower limbs, as shown in Figure 3.

The CRP on Day 20 was found to be elevated enormously to 159 mg/L and on Day 23, the patient complained of severe pain and acrocyanosis. On the same day, the lab investigation showed serum creatinine levels of 148 μmol/L. Amphotericin B use was halted and IV anisodamine was administered at a dose of 20 mg every 6th hour to treat the pain and acrocyanosis. We observed clinical improvement in the patient over 8 days, including a decline in the serum creatinine level to 42 mg/L revealed by the lab investigation; and the creatinine level in the serum was 116 μmol/L. On Day 29, the patient was discharged with oral voriconazole, with complete absence of pain and acrocyanosis (Figure 4).

3 DISCUSSION
Based on the World Health Organization-Uppsala Monitoring Centre criteria and Naranjo's Scale,1 we carried out an assessment for adverse drug reaction (ADR). The improvement in acrocyanosis and pain was observed on amphotericin B withdrawal and treatment with anisodamine. Hence the suspected ADR was probably due to amphotericin B and there were no other factors that could have caused this ADR. According to the Modified Hartwig and Siegel Scale,2 the severity of the ADR was Level 3 and the reaction was a severe ADR.
The possible predisposing factors in this case included renal impairment and the patient's advanced age, which would have been responsible for the elevated serum creatinine as amphotericin B is excreted through the kidneys and the nephrotoxicity was due to the accumulation of the drug in the kidneys. Our patient's renal impairment and advanced age would have increased the potential for this accumulation.3-5 In this case, amphotericin B could have led to liposome-induced elevated serum creatinine because of drug-induced nephrotoxicity. It was not clear whether amphotericin B liposome-induced acrocyanosis and pain were related to impaired renal function; it should be noted that the patient had a history of alcohol and smoking for 40 years. Smoking is associated with Raynaud's phenomenon,6 Buerger's disease, and impaired peripheral vasculature endothelium-dependent vasorelaxation, which might be a considerable risk factor.7 Anisodamine is used for the treatment of acrocyanosis and pain; it has membrane stabilization and cell-protection action (which is probably related to its calcium antagonist action) and it reduces the serum creatinine level.8
In conclusion, this case suggests that careful attention should be paid to amphotericin B-induced acrocyanosis and majorly elevated serum creatinine in elderly patients with a history of smoking and impaired renal function. Anisodamine was used to treat acrocyanosis and pain and the amphotericin B was discontinued. The results need to be further confirmed in a large randomized controlled clinical trial, which is ongoing in our tertiary care teaching hospital.
ACKNOWLEDGMENTS
The authors wish to thank the Dean, and the teaching and nonteaching faculty of Santhiram Medical College and General Hospital for their valuable support for this study. Also, we thank the management of Santhiram College of Pharmacy for providing the hospital facility.
CONFLICT OF INTEREST
There are no conflicts of interest.