Factors associated with the continuum of care of HIV-infected patients in Belgium
Abstract
Introduction
We studied factors associated with the continuum of HIV care in Belgium.
Methods
Data of the national registration of new HIV diagnosis and of the national cohort of HIV-infected patients in care were combined to obtain estimates of and factors related with proportions of HIV-infected patients in each step of the continuum of care from diagnosis to suppressed viral load (VL). Factors associated with ignorance of HIV seropositivity were analyzed among patients co-infected with HIV and STI in the Belgian STI sentinel surveillance network. Associated factors were identified by multivariate logistic regression.
Results
Among 4038 individuals diagnosed with HIV between 2007 and 2010, 90.3% were linked to care. Of 11684 patients in care in 2010, 90.8% were retained in care up to the following year, 88.3% of those were on ART, of whom 95.3% had suppressed VL (<500 cp/ml) (Figure 1). In multivariate analyses, factors associated with ignoring HIV+ status were being younger (p<0.001), being heterosexual compared to MSM, and of a region of origin other than Belgium, Sub-Saharan Africa and Europe. Non-Belgian regions of origin were associated with lower entry and retention in care (p<0.001 for both). Preoperative HIV testing was associated with lower entry in care (p=0.003). MSM had a higher retention in care (p<0.001), whilst IDU had lower retention (p=0.004). Low CD4 at first clinical contact and clinical reasons for HIV testing were independently associated with being on ART (p<0.001 for both); whilst prenatal HIV diagnosis was associated with lower proportion on ART (p=0.016) and lower proportion with suppressed VL among those on ART (p=0.005). Older age was associated with both being on ART and having suppressed VL among those on ART (p=0.007 and p<0.001 respectively), independently of time since HIV diagnosis (Table 1).
Conclusions
Regions of origin and risk groups (MSM/heterosexual/IDU) are the main factors associated with ignorance of HIV seropositivity, entry and retention in care, but once the HIV patient is retained in care, no effect of these factors on the proportions on ART and with suppressed VL are observed. The association of prenatal HIV diagnosis and proportions on ART and with suppressed VL could be biased by transitory CD4 disturbances during pregnancy and ART discontinuation after pregnancy. The higher probabilities of older patients to be on ART and have suppressed VL once retained in care could be influenced by factors not studied here like comorbidities, adherence or duration on ART.
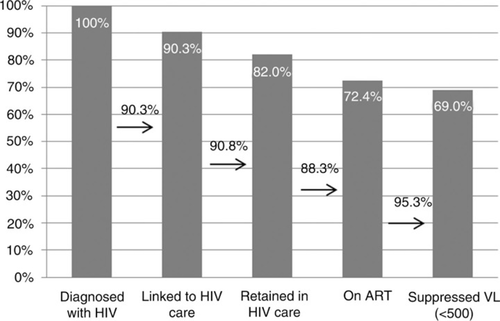
The continuum of HIV care in Belgium.
| Risk factors | Adjusted OR (95% CI)a Undiagnosed HIV + | Adjusted OR (95% CI)a No entry in care | Adjusted OR (95% CI)a No retention | Adjusted OR (95% CI)a On ART | Adjusted OR (95% CI)a Suppressed VL (<500 cp/ml) |
|---|---|---|---|---|---|
| Sex | |||||
| Male | 1 | 1 | 1 | 1 | 1 |
| Female | 1.32 (0.39–4.44) | 0.88 (0.58–1.34) | 0.87 (0.70–1.07) | 0.76 (0.55–1.04)b | 1.02 (0.73–1.42) |
| Age at diagnosis | |||||
| <40 yrs | 1 | 1 | 1 | 1 | 1 |
| ≥40 yrs | 0.42 (0.27–0.64) | 0.98 (0.69–1.39) | 1.05 (0.86–1.28) | 1.31 (1.04–1.65)b | 1.75 (1.27–2.42) |
| Way of transmission | |||||
| Heterosexual | 1 | 1 | 1 | 1 | 1 |
| MSM | 0.39 (0.16–0.95) | 0.86 (0.52–1.44) | 0.61 (0.47–0.78) | 0.80 (0.58–1.09)b | 1.06 (0.72–1.56) |
| IDU | / | 1.50 (0.55–4.11) | 1.88 (1.22–2.88) | 2.42 (0.69–8.46)b | 1.46 (0.52–4.11) |
| Region of origin | |||||
| Belgium | 1 | 1 | 1 | 1 | 1 |
| Sub-Saharan Africa | 1.02 (0.33–3.14) | 3.11 (1.84–5.26) | 1.41 (1.12–1.78) | 0.90 (0.66–1.23)b | 0.73 (0.51–1.03)b |
| Europe | 0.83 (0.41–1.69) | 2.74 (1.59–4.71) | 1.86 (1.38–2.52) | 0.97 (0.67–1.40)b | 0.97 (0.57–1.66)b |
| Other | 2.25 (1.26–4.04) | 3.23 (1.79–5.83) | 1.54 (1.10–2.17) | 0.90 (0.59–1.37)b | 0.89 (0.51–1.48) |
| Reason for testing | |||||
| Patient's request | / | 1 | 1 | 1 | 1 |
| Clinical arguments | / | 0.98 (0.64–1.50) | 0.95 (0.74–1.21) | 1.76 (1.34–2.31)b | 0.92 (0.63–1.35) |
| Prenatal | / | 1.14 (0.51–2.52) | 1.16 (0.75–1.78) | 0.49 (0.30–0.81)b | 0.42 (0.23–0.78) |
| Preoperative | / | 3.22 (1.50–6.89) | 1.21 (0.72–2.04) | 1.14 (0.56–2.31)b | 0.85 (0.35–2.04) |
| Other | / | 0.92 (0.55–1.54) | 1.13 (0.86–1.49) | 1.54 (1.11–2.14)b | 1.03 (0.65–1.63) |
| CD4 at first visit | |||||
| CD4 ≥350 | / | / | 1 | 1 | 1 |
| CD4 <350 | / | / | 1.16 (0.89–1.51) | 8.02 (5.80–11.11) | 1.16 (0.78–1.70) |
- Note: Rem: p<0.05, statistically significant variables presented in italic.
- a Adjusted for sex, age at diagnosis, nationality and ay of transmission
- b additionally adjusted for CD4 value at first visit.