Exercise Training for Heart Failure Patients with and without Systolic Dysfunction: An Evidence-Based Analysis of How Patients Benefit
Abstract
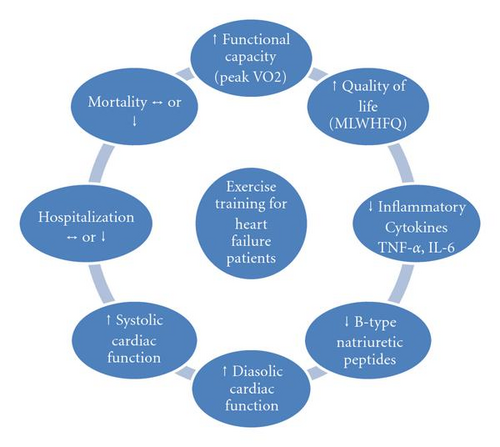
Significant benefits can be derived by heart failure patients from exercise training. This paper provides an evidence-based assessment of expected clinical benefits of exercise training for heart failure patients. Meta-analyses and randomized, controlled trials of exercise training in heart failure patients were reviewed from a search of PubMed, Cochrane Controlled Trial Registry (CCTR), CINAHL, and EMBASE. Exercise training improves functional capacity, quality of life, hospitalization, and systolic and diastolic function in heart failure patients. Heart failure patients with preserved systolic function (HFnEF) participating in exercise training studies are more likely to be women and are 5–7 years older than their systolic heart failure (CHF) counterparts. All patients exhibit low functional capacities, although in HFnEF patients this may be age related, therefore subtle differences in exercise prescriptions are required. Published works report that exercise training is beneficial for heart failure patients with and without systolic dysfunction.
1. Background
Exercise training has become an accepted adjunct therapy for patients with systolic heart failure. Recent data have shown that exercise is considered beneficial for heart failure patients in terms of improved mortality and morbidity [1], quality of life [2, 3], functional capacity [4], and improved cardiac [5] and vascular function [6]. Characteristics of heart failure patients who participate in community-based prevalence and exercise training studies may be different with the latter likely to be younger and predominantly male [1, 4, 7, 8]. North American [9], European [10], and Australian [11] guidelines on the use of exercise training in heart failure patients have been developed, although subtle differences exist between the various guidelines. Subtle differences may also exist in the demographics of heart failure patients with abnormal systolic function (CHF) and heart failure patients with normal left ventricular ejection fraction (HFnEF). CHF patients are normally defined as having left ventricular ejection fraction <50% and impaired diastolic filling, while HFnEF patients have a normal (>50%) ejection fraction but impaired diastolic filling.
The aims of this work were to review highlighted differences between the demographics of heart failure patients participating in prevalence studies and those completing exercise training studies. Moreover demographic data were presented for systolic heart failure patients and those with heart failure with preserved systolic function. This work also aimed to provide a clinical update on the benefits of exercise training in heart failure patients.
2. Methods
Data relating to exercise training protocols in heart failure patients and subsequent outcomes were reviewed. Pub Med (MEDLINE), Medscape, EMBASE, CINAHL, and Cochrane Controlled Trials Registry were searched up until June 2010. Reference lists of papers found were scrutinized for new references. North American, European, and Australian heart failure treatment guidelines were also sourced. Search terms used were combinations of the terms exercise training, heart failure, left ventricular dysfunction, physical training, resistance training, guidelines, position stands, systematic reviews, meta-analysis, quality of life, functional capacity, mortality, morbidity, cardiac function, heart failure with preserved systolic function, safety, cytokine expression, brain natriuretic peptide, and aerobic exercise. There were no restrictions on the year of publication. We examined the latest editions of relevant journals that were not yet available on electronic databases. The reference lists of identified articles were subsequently scrutinized and relevant articles were included. Information on clinical variables was archived in a database. Community-based heart failure prevalence studies were also sought to draw comparisons with exercise studies in heart failure patients.
Outcome measures fell into three categories: demographics, clinical measures, and public health issues. Demographics: age and gender of heart failure patients enrolled in community-based prevalence versus exercise training studies. Clinical measures: mortality and morbidity rates, functional capacity, quality of life, cardiac function, cytokine, and brain natriuretic peptide (BNP) expression in those who did and did not undertake exercise training. Public Health: number needed to treat, cost-effectiveness, safety, and minimization of adverse events during exercise training.
3. Results
3.1. Demographics of Heart Failure Patients in both the Community and in Exercise Training Studies
-
Evidence suggests younger, male heart failure patients are more likely to participate in exercise training due to possible selection bias.


3.2. Demographics of CHF and HFnEF Patients Participating in Exercise Training Studies
-
Evidence suggests CHF patients participating in exercise training are younger and more likely to be male.
3.3. Clinical or Prognostic Characteristics
3.3.1. Mortality and Hospitalization Benefits
-
Evidence equivocal for mortality and hospitalization benefits and also whether disease severity predicts which patients may benefit most.
3.3.2. Functional Capacity
-
Evidence suggest functional capacity undoubtedly improves, but what is uncertain is the size of change in Peak VO2 which is likely to be between 4%–15%.
3.3.3. Quality of Life (QOL)
-
Evidence is unequivocal for improvement in quality of life.
3.3.4. Cardiac (Systolic) Function
-
Evidence suggests exercise training will improve systolic function and should be predominantly aerobic, and if tolerated, intermittent high intensity, in nature as this will convey the greatest improvements in systolic function.
3.4. Cardiac (Diastolic) Function
-
Evidence suggests exercise training may enhance diastolic function.
3.5. Circulating Levels of Proinflammatory Cytokines
-
Evidence—equivocal for reducing systemic levels of inflammatory cytokines.
3.6. Brain Natriuretic Peptide (BNP) Levels
-
Evidence unequivocal that B-type natriuretic peptides are reduced following exercise training, moreover a minimum weekly energy expenditure (circa 400 Kcal · week-1) may be required to elicit changes in B-type natriuretic peptides.
A summary of clinical markers of heart failure prognosis can be seen in Figure 3.
3.7. Public Health Issues
3.7.1. Number Needed to Teat (NNT) to Prevent 1 Death
-
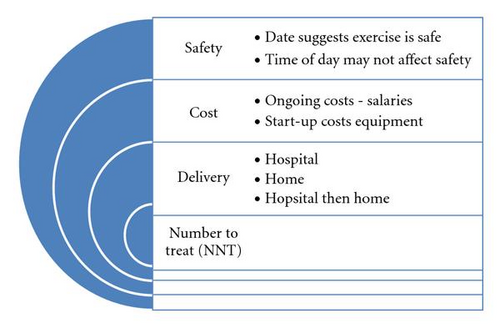
Evidence suggests that 34 heart failure patients need to be provided with exercise training for 12 months to prevent one death from exercise training over this period.
3.7.2. Cost-Effectiveness
-
Evidence suggests exercise training, especially home-based, is a cost effective adjunct treatment.
3.7.3. Safety
Exercise may increase the risk of sudden cardiac death [38]. While both exercise training and the heart failure condition each convey an increased risk of sudden death or adverse event, the published works in this field are yet to identify as single death that could be directly linked to exercise exertion in over 100,00 patient-hours of exercise training [4]. For this reason odds ratios for heart failure patients have not been calculated. Data from the HF-ACTION trial were zero deaths per 1,000 exercise tests and 0.45 nonfatal major CV events per 1,000 exercise tests (95% CI 0.11–1.81). Recent data suggest that although, sudden cardiac death (SCD) and cardiac events are more prevalent in the morning hours, data do not exist to suggest the time of day exercise training is conducted may not increase the risk of SCD or other adverse events [38].
-
Evidence suggests exercise training is safe for heart failure patients, but home exercise is most beneficial when it follows a supervised, hospital-based program.
A summary of public health issues related to heart failure exercise training can be seen in Figure 4.
4. Discussion
A chronological history of exercise training for heart failure patients makes interesting reading. Prior to the 1990’s the advice almost unequivocally given to heart failure patients was to avoid physical exertion. A handful of studies prior to the 1990’s suggested exercise training was safe and possibly beneficial in reducing dyspnea and improving mood. In the 1990’s and 2000’s numerous studies and several meta-analyses have highlighted the importance of regular physical activity in improving not only improving physical fitness and quality of life, but also cardiac and blood vessel function and systemic inflammatory and neurohormonal markers of heart failure. Moreover exercise appears to be safe and most people with heart failure, with the exception of New York Heart Association class IV and some other high risk-heart failure patient categories, should be advised to regularly exercise.
The change in consensus of opinion towards safety and efficacy of exercise training was based upon data synthesis from many small- to medium-sized trials. Notably, meta-analysis [1] had suggested significant mortality and hospitalization benefits could be derived from exercise training heart failure patients, however closer analysis of the data suggested statistical significance of mortality and hospitalization was absent if the study of Belardinelli [15] was removed from the meta-analysis. Then, in late 2008 data was released from the HF-ACTION study [8] the largest (2,300 patients) exercise training study of heart failure patients to date. HF-ACTION reported nonsignificant reductions in mortality and hospitalization. After adjusting for highly prognostic predictors, exercise training was associated with modest significant reductions for both mortality and heart failure hospitalization. These findings together with the cost and efficacy data presented in this paper suggest exercise has a beneficial role in the nonpharmacological management of heart failure.
5. Conclusions
Differences exist in the demographics of participants of prevalence and exercise training studies in heart failure patients. Exercise training is safe, effective, and not cost prohibitive. Evidence shows exercise training-induced improvements are possible in many indicators of heart failure patient prognosis; functional capacity, quality of life, systolic and diastolic function, BNP and NT-pro-BNP expression. Nevertheless it remains questionable whether exercise training reduces cardiac deaths and hospitalisation and whether disease severity predicts which patients are most likely to benefit.