Combined excision and ablation of ampullary tumors with biliary or pancreatic intraductal extension is effective even in malignant neoplasms
Abstract
Background
The feasibility and outcome of endoscopic resection in ampullary tumors with intraductal growth remains unclear.
Objective
To assess the safety, feasibility and outcomes of these patients treated by thermal ablation.
Methods
Retrospective observational study. All consecutive patients who underwent an endoscopic snare papillectomy with a 6-month minimum follow-up were included. Ablation was performed with cystotomes and soft/forced coagulation. Successful endoscopic treatment was defined as no adenomatous residual tissue or recurrence observed at follow-up.
Results
Of 86 patients presenting with an ampullary tumor, 73 (58 ± 14 years old, 49% men, 34% familial adenomatous polyposis) (median tumor size: 20 mm, range: 8–80) were included. En bloc and curative resection rates were achieved in 46.6% and 83.6%, respectively.
Intraductal ingrowth was seen in 18 (24.7%) patients and histologically confirmed in 12 (16.4%). Intraductal ablation achieved a 100% success rate, with a 20-month median follow-up. Most of these patients had malignant forms (n = 8, 66.7%), with a higher adenocarcinoma rate (33.3% versus 3.3%, p = 0.001) compared to extraductal tumors.
Overall, there was a 20.5% complication rate with no significant differences between both groups (p = 0.676).
Conclusions
Intraductal ablation achieves a high therapeutic success rate in ampullary tumors with ≤20 mm ductal extension, even in malignant forms or biliary and pancreatic involvement. The technique is feasible, cheap and safe and may avoid major surgery.
Key summary
- Summary of the established knowledge on this subject
- Endoscopic papillectomy can offer a curative resection in 67–92% of cases.
- Intraductal extension has been described as a relative contraindication for endoscopic resection and is associated with lower curative resection rates and incomplete adenoma removal.
- There is no consensus on the indications for endoscopic papillectomy in intraductal extension of ampullary neoplasms and the maximum intraductal involvement able to be resected endoscopically is unknown.
- What are the significant and/or new findings of this study?
- Combined endoscopic snare papillectomy and intraductal ablation using cystotomes in patients with an ampullary tumour and biliary or pancreatic intraductal extension achieves a high success rate with a 20-month median follow-up.
- Thermal ablation is safe and may be effective even in malignant forms with intraductal extension.
Introduction
Endoscopic papillectomy performed by experienced endoscopists can offer a curative resection in 67–92% of cases.1-3 Most adenomas of the duodenal papillae without intraductal extension and no evidence of malignancy on endoscopic findings can be fully resected by snare papillectomy.4,5 Tumor recurrence of benign lesions occurs in up to 20% of patients and depends on tumor size, final histology, presence of intraductal tumor, coexisting familial adenomatous polyposis and the expertise of the endoscopist.6
Intraductal extension has been described as a relative contraindication for endoscopic resection, associated with lower curative resection rates and incomplete adenoma removal.7 Endoscopic snare resection may be technically challenging in these cases and submucosal injection may lead to an adenoma central depression around biliary and pancreatic orifices.
Thus, there is no consensus on the indications for endoscopic papillectomy in intraductal extension of ampullary neoplasms and the maximum intraductal involvement able to be resected endoscopically is unknown. Access to the intraductal extension can be obtained by balloon dilation or by using a balloon catheter to better expose the neoplasm.8,9 Recently, radiofrequency ablation has been reported as effective therapy with various probes.10,11 Most of these studies are short case series and case reports, and therefore the endoscopic approach in these patients remains unestablished.
The aim of our study was to assess the safety, feasibility and outcomes of patients with ampullary tumors and intraductal ingrowth treated by snare resection and thermal ablation using a cystotome, respectively.
Methods
Patients and previous procedures
This is an observational and retrospective study. All consecutive patients presenting with a tumor of the major papilla from January 2000 to May 2017 who underwent an endoscopic snare papillectomy with curative intent and a 6-month minimum follow-up were included. They were identified from a prospectively collected database. Age, sex and relevant backgrounds such as familial adenomatous polyposis status were collected. Symptoms at diagnosis were also noted. Patients with tumors that had endoscopic features of invasive malignancy and those proven to have distant (M1) or regional lymph node metastasis (N1) were excluded. Patients with less than 6 months of endoscopic follow-up were also excluded. We have not excluded patients with lesions deemed unresectable at the time of endoscopic ultrasound (EUS) or endoscopic retrograde cholangiopancreatography (ERCP) because of intraductal involvement. Intrabiliary and intrapancreatic ingrowths were defined as the evidence of intraductal tumor tissue by EUS, cross-sectional imaging, visual inspection or ductography during ERCP, and proven by histopathological analysis, on the post-resection specimen.
Tumor characteristics by cross-sectional imaging (computed tomography scan and/or magnetic resonance imaging) and linear-array EUS were considered when these techniques were carried out up to 3 months before papillectomy. Notably, tumor size, TNM staging, extra-papillary and intraductal extension (biliary or pancreatic) and pancreas divisum status were collected. Preliminary biopsy results prior to papillectomy were also considered if performed. The study protocol was approved by our local review board (2017/03JUL/353) and conforms to the ethical guidelines of the 1975 Declaration of Helsinki.
Papillectomy technique and outcomes
Papillectomy was performed by four endoscopists with experience in interventional endoscopy using a duodenoscope with a working channel of 3.7–4.2 mm (Olympus, Berchem, Belgium). The number of sessions required to achieve the complete resection of the tumor were considered. Endoscopic papillectomy was performed using an asymmetric (Snaremaster, Olympus) or symmetric polypectomy single-use snare (Captivator, Boston Scientific, Zaventem, Brussels) and electrosurgical current in Endocut I mode Effect 1 (ERBE, Zaventem, Belgium). The piecemeal approach was performed when en bloc resection was not feasible. Lifting by a mixture of epinephrine (dilution 1:1000), fluid gelatin and methylene blue was also performed in tumors with wide extraductal extension at the choice of the endoscopist. ERCP was carried out in all cases to identify biliary and pancreatic orifices and intraductal ingrowth. Endoscopic biliary and/or pancreatic sphincterotomy was decided on an individual basis at the discretion of the endoscopist.
Intraductal thermal ablation by a wire-guided cystotome from 6 to 10 French (Endo-flex, Voerde, Germany) was performed in cases of intraductal ingrowth identified by visual examination, cholangiography during ERCP or previous EUS procedures. The cystotome diameter was decided individually based on the respective biliary and pancreatic duct diameter. Soft coagulation (effect 4–5) or forced coagulation (effect 3, 80 W) was applied during intraductal ablation by the cystotome using monopolar current (VIO3/VIO300D generators, ERBE). Repeat cholangiography or pancreatography to ensure complete ablation was also decided individually. Biliary stenting was performed as prophylaxis in selected patients to prevent bile leakage, delayed perforation and stricture formation. A pancreatic prosthesis was indicated in all cases without pancreas divisum to prevent post-papillectomy pancreatitis, and rectal or intravenous non-steroidal anti-inflammatory drugs were administered prior to the procedure. Hemostasis was performed by cautery, clipping or stenting with self-expanding metal stents. No direct cholangioscopy was performed in this series.
Intraprocedural and early complications (<30 days) were noted. Post-papillectomy acute pancreatitis was defined as the suggestive clinical syndrome (intense abdominal pain newly developed or exacerbated) accompanied by lipasemia over three times the normal range for at least 24 hours or compatible radiological examination and requesting more than an overnight hospitalization. Delayed bleeding was defined as any significant procedure-related hemorrhage requiring endoscopic, surgical or radiological therapy. Preventive hemostasis following papillectomy was not considered as a bleeding complication. All patients had given informed consent prior to the procedure and all procedures were carried out under general anesthesia.
Pathological analysis
A prospective re-read of all ampullary resections and biopsies was performed by three dedicated pathologists (MK, HD, AJM) to assess the intraductal invasion and histomolecular profile. High-grade dysplasia and adenocarcinoma were considered as malignant. Resection margin status of the specimen was collected. Curative resection or successful endoscopic treatment was defined as no adenomatous residual tissue or recurrence observed in follow-up biopsy sampling, with a minimum of 6 months follow-up from the last endoscopic session. The need for surgical resection after endoscopic papillectomy was considered as a non-successful endoscopic treatment, if it confirmed the presence of residual or recurrent lesion.
Statistical analysis
Categorical variables were compared using χ2 test. Normally distributed continuous variables were analyzed by Student t test and non-normally distributed variables by the Mann–Whitney U test. They were presented as mean (±SD) or median (range) respectively. A comparative analysis between extraductal and intraductal tumors was carried out. We have also considered tumors below and above 20 mm in a qualitative way, as piecemeal resection with electrocautery is often performed for lesions ≥ 2 cm.12 A p value < 0.05 was considered statistically significant. The SPSS version 24 was used (IBM, SPSS Inc, Illinois, USA).
Results
Patients
Of 86 patients who underwent endoscopic papillectomy, those with malignant invasive forms but not fit for surgery (n = 3) and insufficient follow-up data (n = 10) were excluded. Finally, 73 patients (58.3 ± 14.8 years old, 49.3% men) presenting with an ampullary tumor (median size: 20 mm, range: 8–80) were included in the study. Most of them were asymptomatic at diagnosis (n = 58, 79.5%), or presented with abdominal pain (n = 7, 9.6%), jaundice (n = 6, 8.2%) or acute pancreatitis (n = 2, 2.7%). Baseline characteristics of these cases comparing patients with and without intraductal involvement are shown in Table 1.
| Feature | All patients | Intraductal ingrowth groupa | Non-intraductal ingrowth group | p value |
|---|---|---|---|---|
| Patient characteristics, n (%) | ||||
| Number of patients | 73 (100) | 12 (16.4) | 61 (83.6) | – |
| Age (years), mean ± SD | 58 ± 15 | 61 ± 16 | 58 ± 15 | 0.666 |
| Male gender | 36 (49.3) | 10 (83.3) | 26 (42.6) | 0.01b |
| Familial adenomatous polyposis | 25 (34.2) | 3 (25) | 22 (36.1) | 0.460 |
| Lesion characteristics, n (%) | ||||
| Tumor size (mm), median (range) | 20 (8–80) | 20 (11–80) | 20 (8–50) | 0.548 |
| Tumor size ≥20 mm | 42 (57.5) | 7 (58.3) | 35 (57.4) | 0.951 |
| Extra-papillary extension | 32 (43.8) | 7 (58.3) | 25 (41) | 0.268 |
| Submucosal lifting | 68 (93.2) | 12 (100) | 56 (91.8) | 0.583 |
- a Histologically proven.
- b Statistically significant.
Preoperative histology was available in 29 cases (39.7%), showing high-grade dysplasia in 11 patients (37.9%) and low-grade in 18 (62.1%). EUS was carried out in 64.4% of cases. All tumors were graded as T1N0M0. There were 42 patients (57.5%) presenting with a tumor ≥20 mm, and extra-papillary extension was described in 32 cases (43.8%). Extra-papillary extension was correlated to tumor size (p < 0.001). En bloc resection was achieved in 34 lesions (46.6%) and a median of 1 (range: 1–5) session was required for removal.
Eighteen patients required two or more endoscopic sessions to achieve a complete resection (24.7%) (Table 2). Piecemeal approach was much more frequent in tumors ≥20 mm (73.8 versus 25.8%, p < 0.001) (Figure 1). There were 28 patients with R0 status (82.4% of en bloc resected, 38.4% of total), 6 (24.4%) with R1 status and 39 (53.4%) with resection margins status non-feasible due to piecemeal resection. Hemostatic thermal ablation was performed in 41 cases (56.2%) and one or more hemostatic clips were used in 63%.
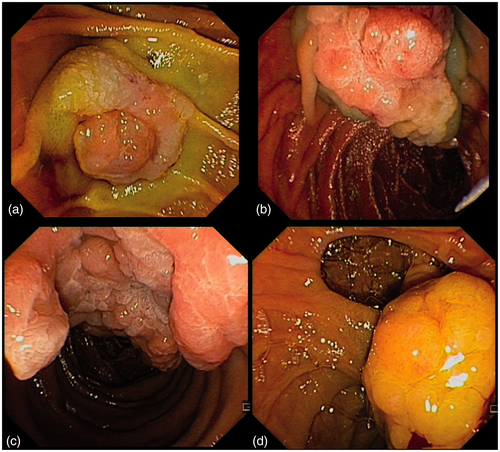
Different presentations of ampullary tumors. (a) A 15-mm, well-delimitated ampullary tumor resected by en bloc endoscopic resection. (b) Malignant ampullary tumor with extra-papillary extension after submucosal injection by a mixture of gelatin fluid, diluted epinephrine and methylene blue. (c) Large extra-papillary extension of an ampullary adenoma resected in piecemeal fashion. (d) Juxta-ampullary duodenal diverticulum.
| Feature | All patients | Intraductal ingrowth group | Non-intraductal ingrowth group | p value |
|---|---|---|---|---|
| Endoscopic therapy, n (%) | ||||
| Number of sessions for ampullary resection, median (range) | 1 (1–5) | 1 (1–5) | 1 (1–5) | 0.358 |
| Several (≥2) endoscopic sessions | 18 (24.7) | 4 (33.3) | 14 (23) | 0.446 |
| Piecemeal resection | 39 (53.4) | 8 (66.7) | 31 (50.8) | 0.314 |
| Complications | 15 (20.5) | 3 (25) | 12 (19.7) | 0.676 |
| Indication for surgery | 4 (5.5) | 1 (0.8) | 3 (4.9) | 0.521 |
| Histopathological analysis, n (%) | ||||
| Malignancy (high-grade dysplasia or adenocarcinoma) | 33 (45.2) | 8 (66.7) | 25 (41) | 0.101 |
| Adenocarcinoma rate | 6 (8.2) | 4 (33.3) | 2 (3.3) | 0.001a |
| Curative resection | 61 (83.6) | 12 (100) | 49 (80.3) | 0.093 |
- a Statistically significant.
Half of the patients with a dilated common bile duct or Wirsung duct (50%) had intraductal extension. Metallic (n = 12) or plastic (n = 18) biliary stents were placed in 41.1% of cases, whereas pancreatic stenting was performed in 90.4% of cases. Reasons for not stenting the pancreatic duct were pancreas divisum (n = 6) or failure of pancreatic cannulation (n = 1).
The short-term (<30 days) complication rate was 20.5%, as follows: delayed bleeding (n = 4), acute pancreatitis (n = 6), perforation (n = 4) and pancreatic duct stricture (n = 1). Among patients presenting with bleeding, clipping was attempted in all cases, and hemostatic powder (Hemospray, Cook Medical, Winston-Salem, North Carolina, USA) was used in three cases. Perforation was diagnosed during the procedure (n = 2) or in early (<48 hours) postoperative (n = 2). Endoscopic therapy by standard or over-the-scope clips to close the perforation was successfully carried out in all cases, with no need of surgery and a satisfactory clinical evolution. The median length of hospitalization in these patients was 7 days (range: 3–15).
Regarding histological analysis, there were 33 malignant adenomatous forms including high-grade dysplasia (n = 27, 37%) and adenocarcinoma (n = 6, 8.2%). Most of adenocarcinomas measured more than 20 mm (n = 5, 83.3%) and had extra-papillary (n = 4, 66.7%) and/or intraductal extension (n = 4, 66.7%). Low-grade dysplasia was confirmed in the remaining 39 patients (53.4%).
Overall, the curative resection rate was 82.2% during a median of 20 months follow-up (range: 6–83). Further duodenopancreatectomy was performed in three cases without intraductal involvement and one case with intraductal presentation (5.5% of the whole population). The histopathological analysis showed adenocarcinoma (n = 2), high-grade dysplasia (n = 1), and no lesion (in the intraductal extension group, n = 1).
Intraductal ablation
Intraductal ingrowth was observed in 18 patients and histologically proven in 12 cases (16.4%). All patients with intraductal extension underwent a median of one session for ampullary resection and one simultaneous session (range: 1–3) of biliary and/or pancreatic ablation by a cystotome (Figure 2).
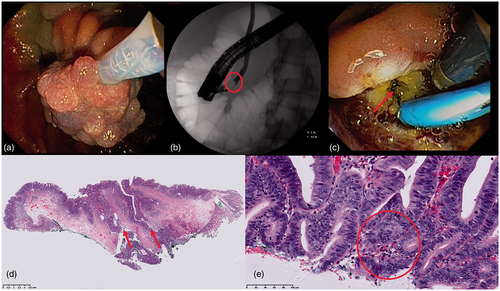
Combined excision and ablation of an ampullary tumor with intraductal extension (a) Endoscopic en bloc resection of a low-grade dysplasia ampullary tumor using a symmetric medium-size snare. (b) A 20-mm intraductal biliary involvement (circle) identified by the cholangiogram during endoscopic retrograde cholangiopancreatography procedure. (c) Intraductal pancreatic thermal ablation of main pancreatic duct (arrow) using a 6Fr cystotome in soft coagulation mode (Effect 4). Biliary plastic stent. (d) Histopathological analysis of an ampullary tumor presenting with biliary involvement (left arrow). Main pancreatic duct (right arrow). (e) High-grade dysplasia (circle), in the same specimen.
As shown in Table 3, cross-sectional imaging detected 4 patients with intraductal involvement also confirmed by EUS, half of them presenting with infra-centimetric extension. EUS detected infra- (n = 7) or supra-centimetric (n = 5) intraductal extension in 12 (66.7%) patients. The maximum intraductal adenoma was 20 mm. ERCP detected 6 patients with <1 cm intraductal ingrowth only. Overall, there were ampullary tumors with only biliary invasion (n = 6), biliary and pancreatic (n = 4), and only pancreatic involvement (n = 2) confirmed by histopathological analysis.
| Diagnostic procedures | Intraductal ingrowth (n = 18) | Intraductal presentation |
|---|---|---|
| EUSa | 12 | 3 biliary and pancreatic, 8 biliary, 1 pancreatic |
| Radiological examinations (CT/MRI)a | 4 | 2 biliary and pancreatic, 2 biliary |
| ERCP | 6 | 1 biliary and pancreatic, 4 biliary, 1 pancreatic |
- a There is an overlap. Intraductal extension detected in four patients by cross-sectional imaging was also confirmed by EUS. Six patients with <1 cm intraductal ingrowth were only diagnosed by ERCP procedure.
- CT: computed tomography; ERCP: endoscopic retrograde cholangiopancreatography; EUS: endoscopic ultrasound; MRI: magnetic resonance imaging.
Most of these patients had high-grade dysplasia or cancer from histological analysis (66.7%). There were 4 patients with adenocarcinoma (33.3%), 4 with high-grade dysplasia and 4 with low-grade dysplasia, all of them presenting an intestinal type. Interestingly, the adenocarcinoma rate was significantly higher in patients with intraductal involvement.
The intraductal therapy was successful in all cases. In one patient, who presented with a 20-mm partially ulcerated ampullary tumor and 20-mm intraductal biliary and 10-mm pancreatic involvement, piecemeal papillectomy and two sessions of intraductal ablation were performed. However, a residual adenocarcinoma was suspected at endoscopic follow-up, but not confirmed on the surgical specimen after duodenopancreatectomy.
The complication rates in intraductal and non-intraductal ablation groups were not statistically different. There were two complications (pancreatitis, pancreatic stenosis) related to intraductal ablation.
Discussion
In our study, we report that combined endoscopic snare papillectomy and intraductal ablation using cystotomes in patients with an ampullary tumor and biliary or pancreatic intraductal extension achieves a high success rate with a 20 months median follow-up. Although the adenocarcinoma rate in those selected cases is significantly higher, this procedure is feasible and safe, with a similar complication rate compared to tumors without intraductal involvement.
There is no consensus on the indication for endoscopy or surgery in patients with intraductal extension. Napoleon et al.,5 in a multicenter prospective study, concluded that endoscopic papillectomy could be considered the first-line treatment for early tumors of the ampulla of Vater without intraductal invasion. Bohnacker et al.7 reported a curative resection rate of 83% in tumors with extraductal location compared to 46% with intraductal extension, as this feature has been reported a risk factor for incomplete resections.13 Conversely, in our series, we observed a high therapeutic success and curative resection rates with intraductal ablation, even if most of our patients presented with high-grade dysplasia or adenocarcinoma.
Bohnacker et al.7 described the need for surgery in 37% of cases with intraductal invasion following incomplete removal by standard endoscopic papillectomy compared to 12% with extraductal presentation (p < 0.001). Intraductal radiofrequency has been proposed as a feasible approach, with a 70% chance of dysplasia eradication at 12 months after a single session.14 Rustagi et al.10 reported a treatment success of 92% in a multicenter retrospective analysis of 14 patients who underwent radiofrequency ablation for intraductal extension. These results are similar to our outcomes by using a cystotome and conventional cautery settings. However, the overall complication rate after radiofrequency was 43% including 5 strictures (35.7%). A 25% stricture rate was also described in a case series.9 In our study, the overall stricture rate was 1.4%, therefore thermal ablation by using a cystotome may have a safe profile with less post-procedural strictures when compared to radiofrequency. The cost of the device is also much lower when compared with radiofrequency probes (423€ versus 1930€).
Pancreaticoduodenectomy has been traditionally proposed as the first-line approach in patients with pT1 ampullary tumors because they have a high risk for nodal metastases, especially if they are higher-grade lesions.15 Transduodenal local resection may be a less invasive and potentially equally effective alternative for cancers with favorable prognostic features.16 Surgical papillectomy with complete resection of the common bile duct has also been recently described in ampullary tumors with 25- to 70-mm biliary involvement.17 Although endoscopic therapy may need more subsequent treatments or sessions, surgery should only be considered after unsuccessful endoscopic treatment because of high postoperative morbidity and mortality, and longer length of hospital stay.18,19 In our series there was only one patient (8.3%) operated on after suspicion of persistence of adenocarcinoma following endoscopic papillectomy and intraductal ablation; however, no lesion was confirmed in the surgical specimen. Furthermore, the endoscopic therapy has been shown to be successful in local recurrences following papillectomy.20
Risk factors for recurrence following endoscopic snare papillectomy have been largely described.12 In small tumors with no intraductal extension or endoscopic features of malignancy a 92.6% overall curative resection rate has been reported.20 Larger tumors are more likely to be incompletely resected or require multiple endoscopic sessions. Submucosal invasion and tumor size have also been reported as predictive factors of lymph node metastases.21 In our series, we show a high curative resection rate even in the presence of intraductal extension; on the contrary, extraductal extension was often “non-curative” due to recurrences during follow-up. This might be due to the piecemeal resection and the large size of lateral extent in some patients (up to 5 cm).
Papillectomy has been described as a high-risk procedure for bleeding22 and pancreatitis. In our report, the complication rate was 20.5% with no differences in intra-/extraductal groups. Probably the biliary stenting by a metal prosthesis has decreased the rate of perforation as there were no perforations related to the intraductal ablation in our series. In addition, the occurrence of a perforation was not related to the need of several endoscopic sessions in our study. Additionally, duct dilation is not necessary because there are catheters in several calibers allowing an adapted cystotome to be used in each individual case. We only observed one pancreatic stricture and the endoscopic treatment was successful.
This study has several limitations besides its retrospective design. We included a heterogeneous group of patients with different tumor characteristics and the pancreatic duct involvement rate was high. The intraductal extension was not precisely measured during EUS/ERCP procedures but only infra- or supra-centimetric values. In this sense, the real intraductal extension may be underestimated in patients with negative EUS and positive ERCP, where previous papillectomy and sphincterotomy may have influenced the length estimation. On the other hand, we have probably not considered in the study some patients with infra-centimetric intraductal invasion not detected by EUS diagnosis or pathological analysis, as the diagnosis may be challenging. We also excluded patients with visible intraductal extension but not confirmed histology, even when ablation was used based on the morphological data, therefore probably underestimating the real rate of ampullary tumors with intraductal ingrowth.
In conclusion, intraductal ablation using a cystotome is feasible, cheap and safe, achieving high therapeutic success rates. This technique should be considered in ampullary tumors with intraductal extension up to 2 cm, as the curative resection rate seems comparable to patients with extraductal presentation, therefore avoiding major surgery.
Acknowledgments
This study was awarded the United European Gastroenterology (UEG) National Scholar Award at the UEG Week 2017.
Author contributions
EPCR and PD designed and coordinated the study, conducted literature review and drafted the manuscript; EPCR, RY and TM performed the analysis and interpreted the data; TA, HP, HD, PD and AJM contributed to critical revision.
Declaration of conflicting interests
The authors declared no potential conflicts of interest for the research, authorship, and/or publication of this article.
Funding
The authors received no financial support for the research, authorship, and/or publication of this article.
Ethics approval
The study protocol was approved by our local review board (2017/03JUL/353).
Informed consent
Informed consent to participate in the study was not required as this is a retrospective design.




