Predictive value of the Diverticular Inflammation and Complication Assessment (DICA) endoscopic classification on the outcome of diverticular disease of the colon: An international study
Abstract
Background
Diverticular Inflammation and Complication Assessment (DICA) endoscopic classification has been recently developed for patients suffering from diverticulosis and diverticular disease.
Aims
We assessed retrospectively the predictive value of DICA in patients for whom endoscopic data and clinical follow-up were available.
Methods
For each patient, we recorded: age, severity of DICA, presence of abdominal pain, C-reactive protein and faecal calprotectin test (if available) at the time of diagnosis; months of follow-up; therapy taken during the follow-up to maintain remission (if any); occurrence/recurrence of diverticulitis; need of surgery.
Results
We enrolled 1651 patients (793 M, 858 F, mean age 66.6 ± 11.1 years): 939 (56.9%) patients were classified as DICA 1, 501 (30.3%) patients as DICA 2 and 211 (12.8%) patients as DICA 3. The median follow-up was 24 (9–38) months. Acute diverticulitis (AD) occurred/recurred in 263 (15.9%) patients; surgery was necessary in 57 (21.7%) cases. DICA was the only factor significantly associated to the occurrence/recurrence of diverticulitis and surgery either at univariate (χ2 = 405.029; p < 0.0001) or multivariate analysis (hazard ratio = 4.319, 95% confidence interval (CI) 3.639–5.126; p < 0.0001). Only in DICA 2 patients was therapy effective for prevention of AD occurrence/recurrence with a hazard ratio (95% CI) of 0.598 (0.391–0.914) (p = 0.006, log rank test). Mesalazine-based therapies reduced the risk of AD occurrence/recurrence and needs of surgery with a hazard ratio (95% CI) of 0.2103 (0.122–0.364) and 0.459 (0.258–0.818), respectively.
Conclusions
DICA classification is a valid parameter to predict the risk of diverticulitis occurrence/recurrence in patients suffering from diverticular disease of the colon.
Introduction
Diverticulosis of the colon is the most frequent structural alteration of the colon diagnosed at colonoscopy.1 It describes the presence of diverticula without any endoscopic sign of inflammation or clinical symptom and it becomes ‘diverticular disease’ (DD), if symptoms develop.2 DD of the colon is not only a growing clinical problem for national health systems since its prevalence is high in developed countries, but also it is increasing in countries where it was thought to be lower.3, 4
To date, there is no consensus about the proper classification of DD. Some classifications are based on imaging, i.e. appearance of the disease at abdominal computerised tomography (CT) (e.g. Buckey, Ambrosetti or Hinchey’s modified classification).5-7 Other classifications focus on clinical features of DD (e.g. the classification of the Scientific Committee of the European Association for Endoscopic Surgery, Sheth classification and, in particular, the Hansen-Stock classification which is widely used in northern Europe).8-10
An endoscopic classification of diverticulosis and DD has only been developed recently. This is surprising if we consider the high number of colonoscopies performed worldwide, that diverticulosis is the most frequently recognised alteration at colonoscopy,1 and that endoscopic signs of diverticular inflammation are found in 0.48–1.7% of patients undergoing colonoscopy.11, 12 Furthermore, some characteristics of the colon harbouring diverticula have already been identified as predictive of the outcome of the disease. For example, radiology has shown diverticulosis extension as one of the strongest predictors of recurrence of diverticulitis.13 However, little is known whether specific endoscopic findings are able to influence the outcome of DD, and patients may differ from each other. For example, having scattered sigmoid diverticula may be different from having diffuse diverticulosis and rigidity of the colon at inflation, but whether this difference has a prognostic significance is little known.
We recently implemented and validated a more specific endoscopic classification of DD of the colon: Diverticular Inflammation and Complication Assessment (DICA). DICA classification takes into account few endoscopic findings of the colon with diverticula,14 and hopefully DICA will better predict the course of the disease. In a first retrospective analysis examining the outcome of DD according to DICA classification, DICA 2 score was associated with a higher risk of diverticulitis and DD recurrence than DICA 1 score. The study, however, was limited by the scant number of patients enrolled and by the absence of cases with the DICA 3 score, the most severe score. Thus, we sought to perform a larger retrospective study on the predictive role of all DICA scores.
Methods
Study design
This was a multicentre, international retrospective cohort study. In order to have results coming from real life, patients with DD were identified from tertiary, secondary and primary clinical centres. Twenty-one centres were in Italy, two in Brazil, one in Venezuela and one in Norway. From 31 December 2014, patients with endoscopic diagnosis of DD were selected if they met the following criteria: (a) cases were at the first endoscopic diagnosis of diverticulosis/DD; (b) cases were properly recorded on electronic database; (c) complete clinical and endoscopic data were available. If clinical follow-up data were incomplete, they could be completed by telephone interview.
The following information was recorded from each patient: age at the time of diagnosis of DD; DICA score at diagnosis; presence of abdominal pain; months of follow-up; C-reactive protein (CRP) > 5 mg/l and faecal calprotectin test positivity at diagnosis (if available); therapy (if any) during follow-up to maintain remission; time to occurrence/recurrence of diverticulitis; need for colonic surgery.
DICA classification
- Diverticulosis extension: left, right colon. Two points are assigned to diverticulosis located in the left colon because diverticulosis (and therefore diverticulitis) occurs more frequently in the left than in the right colon in the Western world.
- Number of diverticula (in each district): up to 15 (grade I), more than 15 (grade II).
- Presence of inflammation: oedema/hyperaemia; erosions; segmental colitis associated with diverticulosis. When different degrees of inflammation were detected, the most severe grade of inflammation had to be reported.
- Complications: rigidity of the colon – poor distension of the diverticular district to inflation, also including a mild stenosis allowing a standard colonoscope to pass through the narrowed lumen; stenosis – a stenosis not allowing a standard colonoscope to pass or narrowed lumen with elevated risk of perforation due to presence of some anatomical characteristics (e.g. a several diverticula at the splenic flexure); pus – purulent material passing from the diverticular opening; bleeding.
Therefore, DICA was classified as DICA 1 (up to three points); DICA 2 (four to seven points); DICA 3 (more than seven points).
The DICA score appears to be associated with the severity of abdominal pain, erythrocyte sedimentation rate (ESR) and CRP levels.14 Thus, DICA 1 may be considered a simple diverticulosis, DICA 2 may range between a severe diverticulosis and a milder diverticulitis, DICA 3 may be considered as a more severe diverticulitis or as a complication following diverticulitis (i.e. stenosis).
Endpoints
We assessed whether DICA classification may relate to the natural history of DD, looking at primary and secondary end points.
Primary endpoints were: (a) occurrence/recurrence of acute diverticulitis (AD), defined as detection of acute left lower quadrant pain associated with thickening of colonic wall harbouring diverticula (at ultrasonography or at abdominal computerised tomography) and/or increased white blood cells count and/or CRP and/or fever.15 Since DICA 1 is diverticulosis without sign of inflammation, and DICA 2 and 3 indicate diverticulosis with a sign of present (DICA 2) or present/past inflammation (DICA 3), we defined as ‘occurrence’ the AD detected in DICA 1 during the follow-up, and as ‘recurrence’ the AD detected in DICA 2 and 3 during the follow-up. We also assessed the occurrence of complicated AD, defined as detection of acute left lower quadrant pain associated with thickening of colonic wall harbouring diverticula and presence of abscesses and/or stenosis and/or fistulas (at ultrasonography or abdominal CT) and/or increased white blood cells count and/or CRP and/or fever;15 (b) need for surgery, as a consequence of DD. In those patients, we assessed also the rate of urgent surgery (defined as surgery for acute obstruction or for free perforation).
The secondary aims of the study were to assess whether DICA classification may have an impact on scheduled therapies for preventing AD occurrence/recurrence. Hence, we recorded if the patient was taking the scheduled therapy or not, and which type of treatment was prescribed.
Several therapies are currently prescribed in clinical practice for control of symptoms and prevention of diverticulitis occurrence/recurrence, ranging from fibre to mesalazine, and doses are quite different.1, 2 Hence, in order to have groups as homogeneous as possible, we classified therapies as follows: rifaximin-based, mesalazine-based, mesalazine + rifaximin, and other (including any other treatment, i.e. fibre, probiotics, spasmolithics, systemic antibiotics).
Statistical analysis
Categorical variables were expressed as absolute values and percentages in the text and tables, whereas continuous variables were expressed as mean with 95% confidence interval (CI). Pearson χ2 was used for categorical data.
Two types of events were considered as endpoints: (a) occurrence/recurrence of diverticulitis, and (b) need for colonic surgery, as a consequence of DD. The prognostic/predictive value of several parameters (DICA classification, therapies, age and gender) was evaluated using time-to-event methods for censored observations, because of the varying length of follow-up. Follow-up times were calculated from the date of diagnosis to the date of event or censorship. Time-to-event analysis was carried out using Kaplan–Meier estimates to draw the cumulative incidence curves, compared by logrank tests, as well as by univariate and multivariate Cox’s proportional hazards models of prognostic variables. Different models were designed for each of the endpoints. The hazard ratio (HR) or relative hazards are presented with 95% CIs and p -values. A ratio higher than unity implies a higher probability of an event compared to the reference group. Values of p < 0.05 were considered to be statistically significant. All statistical tests were two-sided. SPSS 13.0 (SPSS, Inc., Chicago, Illinois, USA) was used for the statistical analyses.
Research ethics and patient consent
The study has been conducted according to the World Medical Association Declaration of Helsinki. It was reviewed and approved after a meeting of all the authors, and was also approved by the Institutional Review Board. All study participants provided informed written consent prior to endoscopic investigation.
Results
Characteristics of the study group
The study enrolled 1651 patients according to the above reported criteria. No differences were found in diverticulosis location between European and South American patients, since it was mainly located in the left colon in all of them. According to DICA score, patients were distributed as follows: 939 (56.9%) patients were DICA 1, 501 (30.3%) patients were DICA 2 and 211 (12.8) patients were DICA 3. However, in the subgroup of 68 coming from Brazil and Venezuela 52 (76.5%) patients were DICA 1, 13 (19.1%) patients were DICA 2 and three (4.4%) patients were DICA 3. A significant difference was present in this subgroup compared with the entire study group (p = 0.005).
Mean age did not differ between the three groups, while males were significantly fewer in DICA 3 (p = 0.003). Presence of abdominal pain, CRP positivity and faecal calprotectin positivity were significantly related to the DICA score. In particular, abdominal pain ranged from less than 40% of DICA 1 to more than 85% of DICA 3, CRP positivity ranged from about 18% of DICA 1 to about 90% of DICA 3, faecal calprotectin positivity ranged from less than 49% of DICA 1 to more than 93% of DICA 3 (p < 0.0001 for each parameter). The characteristics of the study group are summarised in Table 1.
| Characteristics | DICA 1 (939 pts) | DICA 2 (501 pts) | DICA 3 (211 pts) | p a |
|---|---|---|---|---|
| Mean age, years (95% CI) | 66.7 (66.0–67.4) | 66.3 (65.4–67.3) | 66.6 (65.2–68.3) | |
| Sex, male | 454 (48.3) | 259 (51.7) | 80 (37.9) | 0.003 |
| Abdominal pain | 367 (39.1) | 386 (77.0) | 182 (86.2) | <0.0001 |
| C-reactive protein >5 mg/L | 92/502 (18.3) | 247/385 (64.1) | 171/189 (90.5) | <0.0001 |
| Faecal calprotectin, positive | 141/290 (48.6) | 218/246 (88.6) | 152/163 (93.2) | <0.0001 |
- CI: confidence interval; DICA: Diverticular Inflammation and Complication Assessment; pt: patient.
- Values are expressed as n (%) of patients, unless otherwise specified.
- a Chi-square test, two degrees of freedom.
Primary endpoints
The median (interquartile range) follow-up was 24 (9–38) months. AD occurred/recurred in 263 (15.9%) patients. At each level of DICA classification a significant increase of AD occurrence/recurrence was detected (Figure 2 ). In particular, AD occurred in 34 (3.8%) patients in DICA 1, and recurred in 110 (21.9%) patients in DICA 2, and in 119 (56.4%) patients in DICA 3. Acute complicated diverticulitis occurred in 23 (1.4%) patients, and was significantly more frequent in DICA 3: it occurred in one of the DICA 1 patient group, in seven of the DICA 2 patient group, and in 15 of the DICA 3 patient group (p = 0.038).
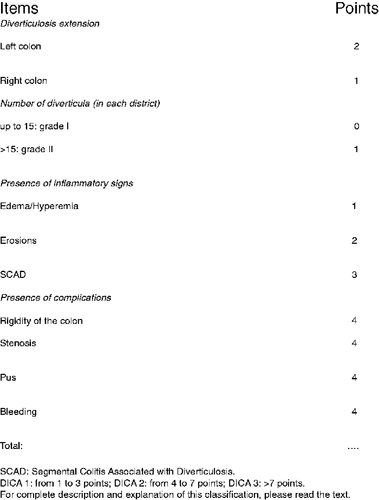
Diverticular Inflammation and Complication Assessment (DICA) endoscopic classification for diverticular disease of the colon.
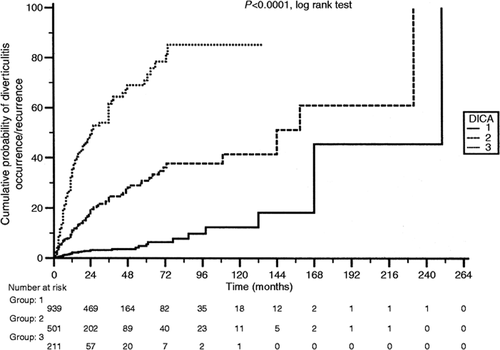
Kaplan-Maier analysis of cumulative rates of diverticulitis occurrence/recurrence during follow-up by Diverticular Inflammation and Complication Assessment (DICA) score.
Surgery was necessary in 57 (3.5%) of those cases. At each level of DICA classification a significant increase of surgery was detected (Figure 3 ). In particular, it was necessary in three (0.3%) patients in the DICA 1 group, in 21 (4.2%) patients in the DICA 2 group, and in 33 (15.6%) patients in the DICA 3 group. The reasons for surgery differed but not significantly between the three groups. In particular, urgent surgery occurred in 32 (1.9%) of cases, and it was necessary in one (33.3%) patient with DICA 1, in 11 (52.4%) patients with DICA 2, and in 20 (60.6%) patients with DICA 3 (p = 0.333).
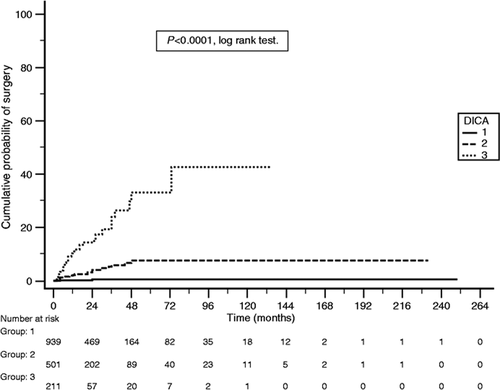
Kaplan-Maier analysis of cumulative rates of surgery during follow-up by Diverticular Inflammation and Complication Assessment (DICA) score.
DICA score was the only factor significantly associated with the occurrence/recurrence of AD and surgery either at univariate or multivariate analysis (Tables 2 and 3 ).
| Univariate Cox PH model | Multivariate analysis Cox PH model | ||||||
|---|---|---|---|---|---|---|---|
| χ2 (DF) | p | HR | 95% CI | HR | 95% CI | p | |
| DICA score | 405.029 (2) | <0.0001 | – | – | 4.319 | 3.639–5.126 | <0.0001 |
| DICA 2 vs DICA 1 | 106.308 (1) | <0.0001 | 5.872 | 4.174–8.261 | – | – | – |
| DICA 3 vs DICA 1 | 459.293 (1) | <0.0001 | 18.992 | 12.267–29.406 | – | – | – |
| DICA 3 vs DICA 2 | 93.648 (1) | <0.0001 | 3.283 | 2.432–4.432 | – | – | – |
| Therapy | 7.135 (1) | 0.0076 | 1.406 | 1.100–1.796 | 1.161 | 0.888–1.518 | 0.2765 |
| Sex | 0.073 (1) | 0.7872 | 1.034 | 0.811–1.318 | 1.105 | 0.862–1.416 | 0.4324 |
| Age < 65 years | 2.911 (1) | 0.0880 | 0.811 | 0.632–1.039 | 1.109 | 0.868–1.418 | 0.4081 |
- CI: confidence interval; DF: degree of freedom; DICA: Diverticular Inflammation and Complication Assessment; HR: hazard ratio; PH: proportional hazard.
| Univariate Cox PH model | Multivariate Cox PH model | ||||||
|---|---|---|---|---|---|---|---|
| χ2 (DF) | p | HR | 95% CI | HR | 95% CI | p | |
| DICA score | 147.795 (2) | <0.0001 | – | – | 6.826 | 4.526–10.295 | <0.0001 |
| DICA 2 vs DICA 1 | 28.669 (1) | <0.0001 | 12.815 | 5.549–29.597 | – | – | – |
| DICA 3 vs DICA 1 | 159.848 (1) | <0.0001 | 59.538 | 24.196–146.499 | – | – | – |
| DICA 3 vs DICA 2 | 37.919 (1) | <0.0001 | 4.703 | 2.541–8.704 | – | – | – |
| Therapy | 1.370 (1) | 0.2418 | 1.378 | 0.816–2.329 | 1.248 | 0.698–2.231 | 0.458 |
| Sex | 1.461 (1) | 0.2268 | 0.727 | 0.432–1.223 | 1.744 | 1.024–2.872 | 0.052 |
| Age < 65 years | 0.531 (1) | 0.4661 | 0.823 | 0.481–1.407 | 1.031 | 0.609–1.746 | 0.908 |
- CI: confidence interval; DF: degree of freedom; DICA: Diverticular Inflammation and Complication Assessment; HR: hazard ratio; PH: proportional hazard.
Secondary endpoints
Therapy with various regimens was taken by 883 (53.5%) patients during the follow-up. In particular rifaximin-based therapy was taken by 337 (38.1%) subjects, mesalazine-based therapy by 298 (33.7%) subjects, rifaximin combined with mesalazine by 111 (12.6%) subjects and other therapies by 137 (15.5%) subjects. Being on therapy was effective to prevent occurrence/recurrence of AD in those with DICA 2 with a HR (95% CI) of 0.598 (0.391–0.914) (p = 0.006, log rank test). No significant effect was detected either in DICA 1 patients (p = 0.109, log rank test) or in DICA 3 patients (p = 0.437, log rank test). Therapeutic regimens including mesalazine were the only effective therapies to reduce diverticulitis occurrence/recurrence compared to no therapy (Figure 4 ).
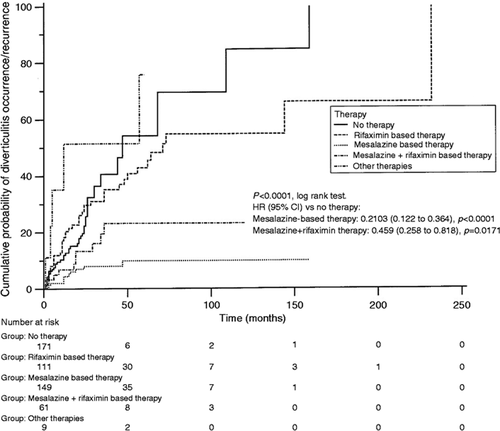
Kaplan-Maier analysis of cumulative rates of diverticulitis occurrence during follow-up by type of therapy in Diverticular Inflammation and Complication Assessment (DICA) 2 group. CI: confidence interval; HR: hazard ratio.
Discussion
The prevalence of diverticulosis and DD is increasing in clinical practice, affecting up to 65% of subjects aged 65 years or more.16 Although colonic diverticulosis remains asymptomatic in most cases, about 20% of patients will develop symptoms, i.e. DD1, 2 and in this group 15% will ultimately develop complications (namely AD).17, 18 DD represents a significant burden on westernised national health systems. In the USA, DD accounts for more than 300,000 hospital admissions, 1.5 million inpatient care days, and US$2.4 billion in direct costs each year.1 The incidence of DD and its complications appears to be increasing and the number of patients with DD can be expected to increase in coming years in accordance with current trends as the population continues to age. In the USA, overall annual age-adjusted admissions for AD increased at a rate of 26% from 1998–2005 and rates of admission increased significantly in both younger and older people. Moreover, elective operations for diverticulitis rose up to 29% in the same time period, especially in younger people (73% in rates of surgery for those individuals).19 Finally, in Europe DD accounts for about 13,000 deaths/year.16
Since diverticulosis is the most common finding at colonoscopy,1 and since endoscopic signs of inflammation may be frequently detected in those patients,11, 12 it is hypothesised that endoscopic characteristics may be predictive of the outcome of the disease. The DICA classification has been developed and validated in order to fulfil the following end-points: to use a common language in describing the colon harbouring diverticula and to identify endoscopic findings predictive of disease outcome. While the first endpoint has already been reached,14 the second endpoint has been reached in this study.
The first finding of this large, retrospective, multicentre, international study is that the clinical characteristics of people harbouring diverticula are linked to DICA score. In particular, we found that severity of abdominal pain, CRP and faecal calprotectin expression were significantly expressed according to DICA score. Moreover, we found that DICA classification is the only predictor for occurrence/recurrence of AD. Thus, patients with simple diverticulosis, and without signs of active or past inflammation, namely DICA 1 patients, are at lower risk of developing inflammatory complications, while patients having diverticulosis with signs of active or past inflammation, namely DICA 3, are at higher risk. The same seems to occur when we consider surgery for those patients: DICA 1 patients are at lower, while DICA 3 ones are at higher, risk of surgery. An interesting observation is that diverticulosis shows higher prevalence in the left colon in both European and South American patients, while DICA 3 score was significantly less frequent in South American than in European patients. This may be a bias of the retrospective design of the study, since the South American population was significantly smaller than the European population. We can also speculate that high fibre diet in South American patients, such as high consumption of tapioca flour, may be protective from severe inflammatory complication as in DICA 3 but not from diverticulosis. However, this last hypothesis has to be confirmed by prospective studies. Another interesting observation is that DICA 3 patients are predominantly female (62.1%). Since there is not a specific gender-prevalence of diverticular disease,1 we can speculate that this observation may be again a bias of the retrospective design of the study. In this way, it will be interesting to see whether this observation will occur in the prospective study too: if this does occur, gender could be considered as predictor of DICA severity and causes have to be further investigated.
A second finding of this study is that we identified for the first time a specific subgroup of patients having diverticulosis, who require scheduled treatment in order to prevent occurrence/recurrence of complications. Outcomes were not influenced by scheduled treatment in DICA 1 and 3 patients. Hence, to advise scheduled treatment in those patients does not influence the risk of developing occurrence/recurrence of AD or need of surgery: DICA 1 patients persist in being at lower risk while DICA 3 patient persist in being at higher risk. On the contrary, DICA 2 is the only subgroup in which treatment influences the outcome of the disease. These patients showed lower occurrence/recurrence of AD or need of surgery under scheduled treatment than patients under simple clinical observation without therapy.
The third finding of this study is that mesalazine-based therapies were identified as the best treatments to reach these outcomes. The beneficial effect of mesalazine occurs in those patients with signs of mild inflammation (i.e. oedema or hyperaemia), that can be easily managed with an anti-inflammatory drug.20-22 The use of probiotics or rifaximin alone seems less effective because the studies on intestinal microbiota in those patients seems to be inconclusive so far.23, 24 The predictive role of DICA may also explain why the majority of studies found mesalazine ineffective in preventing recurrence of AD.25-30 We know that mesalazine seems to be effective at least in controlling symptoms following AD, but only in patients at the first attack of acute uncomplicated diverticulitis.25, 26 It is hypothesised that those patients have DICA 2 scores. On the contrary, mesalazine is completely ineffective in patients with recurrent attack of acute uncomplicated diverticulitis, patients that are more likely to have DICA 3 scores. We can speculate on this different mesalazine behaviour in these subgroups. In DICA 2, inflammation may be confined in colonic mucosa where mesalazine is able to work.31 On the contrary, in DICA 3 we have past (rigidity/stenosis) or active (pus) inflammation involving the entire colonic wall where mesalazine, a drug working only in the mucosa, is probably no effective.31
The results of this study also open up a discussion on how to manage patients with DICA 3 scores. We know that recurrent uncomplicated diverticulitis may be successfully managed without surgery, and that a small percentage of those patients develop complicated diverticulitis.32 However, if DICA 3 patients are symptomatic and unresponsive to scheduled medical treatment to prevent complication, elective surgery may be an option due the high risk of surgery in those patients. In this way, the debate on how to manage those patients (scheduled therapy vs elective surgery) may be re-opened, and the classical advice to submit patients to surgery after the second attack of AD may be reconsidered.17, 33
Of course, the retrospective design of this study has some limitations on the interpretation of these findings. For example, our results cannot be considered as a complete expression of what happens in the real clinical setting because we enrolled only patients responding to strict criteria. Moreover, clinical characteristics of the enrolled population are absent, and we know that the clinical picture is very important in the decision-making process in these patients.31 Another limitation is that treatments prescribed in order to prevent occurrence/recurrence of AD were not randomised.
In conclusion, this study found for the first time that DICA classification has predictive value on the outcome of DD of the colon. Moreover, we found that only DICA 2 patients have benefit from scheduled therapy in preventing occurrence/recurrence of AD. Further prospective studies are welcomed to confirm these results.
Funding
No funding was obtained for this study.
Conflict of interest
Silvio Danese has served as a speaker, a consultant and an advisory board member for Nycomed, Alfa Wasserman, Ferring; Carmelo Scarpignato has served as a speaker and advisory board member for Alfa Wassermann; Francesco Di Mario has served as a speaker and advisory board member for SOFAR Farmaceutici SpA. The other authors have no personal interests to declare.
Acknowledgements
Antonio Tursi is the guarantor of the article. Those who made a substantial contribution to the concept and design, acquisition of data or analysis and interpretation of data were: Antonio Tursi, Giovanni Brandimarte, Francesco Di Mario; Maria L Annunziata, Mauro Bafutto, Maria A Bianco, Raffaele Colucci, Rita Conigliaro, Silvio Danese, Rudi De Bastiani, Luigi Di Cesare, Walter Elisei, Ricardo Escalante, Roberto Faggiani, Luciano Ferrini, Giacomo Forti, Giovanni Latella, Piera G Lecca, Maria G Graziani, Enio C Oliveira, Alfredo Papa, Antonio Penna, Piero Portincasa, Kjetil Søreide, Antonio Spadaccini, Paolo Usai, Costantino Zampaletta, Claudio Cassieri, Alberto Damiani, Kari F Desserud, Serafina Fiorella, Rosario Landi, Elisabetta Goni, Maria A Lai, Flavia Pigò, Gianluca Rotondano, Giuseppe Schiaccianoci, Stefanos Bonovas, Carmelo Scarpinato, Marcello Picchio. Those who drafted the article or revised it critically for important intellectual content: Giovanni Brandimarte, Francesco Di Mario; Maria L Annunziata, Mauro Bafutto, Maria A Bianco, Raffaele Colucci, Rita Conigliaro, Silvio Danese, Rudi De Bastiani, Luigi Di Cesare, Walter Elisei, Ricardo Escalante, Roberto Faggiani, Luciano Ferrini, Giacomo Forti, Giovanni Latella, Piera G Lecca, Maria G Graziani, Enio C Oliveira, Alfredo Papa, Antonio Penna, Piero Portincasa, Kjetil Søreide, Antonio Spadaccini, Paolo Usai, Costantino Zampaletta, Claudio Cassieri, Alberto Damiani, Kari F Desserud, Serafina Fiorella, Rosario Landi, Elisabetta Goni, Maria A Lai, Flavia Pigò, Gianluca Rotondano, Giuseppe Schiaccianoce, Stefanos Bonovas, Carmelo Scarpignato, Marcello Picchio. Those who approved the version to be published: Giovanni Brandimarte, Francesco Di Mario; Maria L Annunziata, Mauro Bafutto, Maria A Bianco, Raffaele Colucci, Rita Conigliaro, Silvio Danese, Rudi De Bastiani, Luigi Di Cesare, Walter Elisei, Ricardo Escalante, Roberto Faggiani, Luciano Ferrini, Giacomo Forti, Giovanni Latella, Piera G Lecca, Maria G Graziani, Enio C Oliveira, Alfredo Papa, Antonio Penna, Piero Portincasa, Kjetil Søreide, Antonio Spadaccini, Paolo Usai, Costantino Zampaletta, Claudio Cassieri, Alberto Damiani, Kari F Desserud, Serafina Fiorella, Rosario Landi, Elisabetta Goni, Maria A Lai, Flavia Pigò, Gianluca Rotondano, Giuseppe Schiaccianoce, Stefanos Bonovas, Carmelo Scarpignato, Marcello Picchio.




