Latent Profiles of Nighttime-Specific Smartphone Use and Smartphone Addiction Among Medical Students: Associations With Bedtime Procrastination and Sleep Disturbance
Abstract
Objective: This study explored heterogeneity patterns of co-occurrence between nighttime-specific smartphone use and smartphone addiction as well as their relationships with bedtime procrastination and sleep disturbance.
Methods: A total of 2052 medical students were asked to complete the questionnaires. Latent profile analysis was used to determine the potential profile of nighttime-specific smartphone use and smartphone addiction.
Results: Four unique profiles for nighttime-specific smartphone use and smartphone addiction in medical students were identified: low, low-moderate, moderate-high, and high profile. Medical students in higher grades were prone to exhibit nighttime-specific smartphone use and smartphone addiction. The results revealed that those with high levels of nighttime-specific smartphone use and smartphone addiction reported severe bedtime procrastination and more sleep disturbance.
Conclusions: The overlap and heterogeneity of nighttime-specific smartphone use and smartphone addiction existed in medical students. Early identification of the patterns of nighttime-specific smartphone use and smartphone addiction could be an effective strategy to prevent sleep problems.
1. Introduction
The popularity of smartphones has skyrocketed due to the convenience they offer with their diverse range of functions. People nowadays are deeply immersed in a technological world, constantly using smartphones at all times and in various locations [1]. Roughly a third of youths between 16 and 24 years of age engage with their smartphones during sleeping hours [2]. An Australian longitudinal study found that only a few adolescents mentioned not using their phones after turning off the lights [3]. Bedtime smartphone usage means adolescents and young adults, after getting into bed, do not close their eyes to fall asleep promptly but instead engage in excessive smartphone activities (e.g., scrolling through social media and playing games) [4, 5].
Smartphone overuse also brings a risk of addictive behaviors for individuals [6]. Smartphone addiction is defined as compulsive and problematic behavioral patterns of smartphone use and uncontrolled use of smartphones [7]. In the context of China, medical students often face extended study periods, rigorous professionalism, heightened academic demands, and significant clinical pressure [8]. Compared with students pursuing other disciplines, medical students in China tend to be more vulnerable to smartphone addiction [9]. Epidemiologic studies have shown relatively high rates of smartphone addiction among medical students, ranging from 22% to 52.8% [10, 11].
1.1. Identifying Specific Patterns of Nighttime-Specific Smartphone Use and Smartphone Addiction
Problematic use and use before sleep are the important dimensions of smartphone use behaviors [2]. Prior research has indicated that excessive smartphone use before bedtime significantly leads to smartphone addiction [12]. Individuals who struggle with smartphone addiction often find it challenging to refrain from using their devices or manage distractions before sleeping [13]. This directionality suggests that nighttime-specific smartphone use and smartphone addiction may occur simultaneously. However, few studies have directly combined night-specific smartphone use with smartphone addiction, and research on their co-occurrence remains limited. Previous research has predominantly employed a variable-centered approach to investigate the relationship between nighttime-specific smartphone use and smartphone addiction [12]. This approach provides a better understanding of the relationships among study variables based on the assumption that all individuals are from a sample [14, 15]. However, the above variable-centered approach failed to consider individual differences, potentially leading to overly generalized conclusions drawn from the sample [16]. To address this limitation, latent profile analysis (LPA), an extension of latent class analysis of observed continuous indicators, is a person-centered method that concentrates on the individual level and allows for the differentiation of meaningful patterns of characteristics in subgroups [17, 18]. This method categorizes participants into mutually exclusive classes or profiles based on item responses to illustrate the heterogeneity of the target population [17]. It may be the best method to identify class heterogeneity when clinical interviews are not available.
Some scholars have initiated the application of LPA to investigate the heterogeneity of smartphone usage. The number of subgroups identified in their studies varied significantly, encompassing a range from three to seven distinct categories [19, 20]. For instance, a three-class latent group model regarding problematic smartphone use was found among college students, including mild, moderate, and severe classes [19]. Smartphone users were also classified into four latent profiles based on their level of smartphone impact and interaction preferences [21]. However, the above studies were limited to exploring nighttime-specific smartphone use. Given the co-occurrence of nighttime-specific smartphone use and smartphone addiction, LPA could be used to better understand the patterns of nighttime-specific smartphone use and smartphone addiction.
1.2. Consequences of Nighttime-Specific Smartphone Use and Smartphone Addiction on Bedtime Procrastination and Sleep Disturbance
Prolonged smartphone use at night increases the risk of bedtime procrastination and sleep disturbance, leading to reduced sleep quality [22, 23]. The blue light emitted by the screens may disrupt the circadian rhythm cycle and potentially impact the alternation of sleep quality, particularly resulting in a reduction in deep sleep [24]. Problematic smartphone use positively predicted later bedtime procrastination [25] and had a significant indirect effect on sleep disturbance [26]. From the perspective of healthy behavior, temporal self-regulation theory (TST) [27] sheds light on how the frequency of past behaviors and the availability of environmental cues for action shape an individual’s healthy habits. The constant and excessive use of smartphones, particularly at night, transforms their usage into a potent behavioral trigger that contributes to sleep problems [3, 28]. This, subsequently, can exacerbate the reduction in sleep duration and worsen bedtime procrastination [29]. However, a systematic review indicates that the relationship between smartphone use and delayed bedtime, as well as poor sleep quality, remains inconclusive [30]. Besides, a diary study revealed that adolescents who use their smartphones for a longer period before bedtime compared to their usual routine tend to go to sleep later [31]. It is imperative to explore whether distinct subgroups of medical students exist, each exhibiting different patterns of nighttime smartphone usage and addiction, to determine their correlation with bedtime procrastination and sleep disturbance.
1.3. The Present Study
Previous research on nighttime-specific smartphone use and smartphone addiction have mainly focused on specific variables while overlooking the heterogeneity in smartphone use patterns among medical students. Clarifying the heterogeneity in nighttime-specific smartphone use and smartphone addiction provides a better understanding of how students use smartphones. To the best of our knowledge, no study has yet explored the heterogeneity in nighttime-specific smartphone use and smartphone addiction through a person-centered approach, nor has it explored their associations with bedtime procrastination and sleep disturbance. Therefore, this research will employ LPA to identify distinct patterns of nighttime smartphone usage and addiction among medical students and to delve into the correlation between these patterns and bedtime procrastination, as well as sleep disturbance. Our findings will serve as a valuable guide for precision interventions addressing related sleep problems.
2. Methods
2.1. Study Design and Participants
We selected participants from one university in Shanxi, China, during November 2022. A stratified sampling method was used to recruit students from Grade 1 to Grade 4. A total of 2052 participants aged from 17 to 25 years old (M = 20.00 and SD = 1.53) were included in the present study. Because the ratio of male to female for this university was about 7:1, over two-thirds of students were females (n = 1403, 68.4%) in this study. The majority of students were sophomores (n = 618, 30.1%), followed by seniors (n = 561, 27.3%), freshmen (n = 476, 23.2%), and juniors (n = 397, 19.3%). A little over half of students came from rural areas (n = 1042, 50.8%). About one-fifth of the participants came from one-child families (n = 488, 23.8%). A little more than half of students self-identify as coming from low-income families (n = 1162, 56.6%). More details are presented in Table S.1.
Prior to the research, we received informed consent from all participants. All responses to the survey would be confidential and informed to all the students. Participants were asked to complete structured questionnaire via online platforms, Sojump. Each questionnaire takes approximately 30 minutes to complete. All study procedures were approved by Research Ethics Committee of the School of Public Health, Shandong University and it has been conducted in accordance with the ethical standards of 1964 Declaration of Helsinki.
2.2. Measures
2.2.1. Nighttime-Specific Smartphone Use
The measure of nighttime-specific social media use was adopted in our study [32]. According to the purpose of the present study, we revised the original measure. Social media use was changed to smartphone use for each item. This scale consisted of 7 questions and each item was rated on a 6-point scale. Higher scores indicated higher levels of nighttime-specific smartphone use. This scale had a good reliability in the current sample, with Cronbach’s alphas of 0.85.
2.2.2. Smartphone Addiction Scale
The Smartphone Addiction Scale-Short Version (SAS-SV) was used to assess the level of smartphone addiction [33]. The SAS-SV contains 10 items and each item was rated on a 6-point scale ranging from 1 (strongly disagree) to 6 (strongly agree). Higher scores reflected more addiction to smartphone addiction. This scale had a good reliability in the current sample, with Cronbach’s alphas of 0.93.
2.2.3. Bedtime Procrastination Scale (BPS)
The Chinese Version of BPS was used to assess bedtime procrastination [34]. The BPS contains 9 items and each item was rated on 5-point scale ranging from 1 (never) to 5 (always). Higher scores reflected more severity of bedtime procrastination. This scale had a good reliability in the current sample, with Cronbach’s alphas of 0.87.
2.2.4. Sleep Disturbance
The short form of sleep disturbance scale was used to assess sleep disturbance [35]. This scale consisted of 8 questions and each item was rated on a 5-point scale. Higher scores indicated more sleep disturbance and poorer sleep quality. This scale had a good reliability in the current sample, with Cronbach’s alphas of 0.85.
2.3. Statistical Analyses
Descriptive analysis and Spearman’s correlation coefficient were used to analyze the relationship between the studied variables. LPA was used to identify the latent subpopulations within a heterogeneous sample for nighttime-specific smartphone use and smartphone addiction. Based on the individual item means, latent profiles were interpreted. Latent profile prevalence specified how many people can be classified into groups with patterns of similar characteristics. A series of model fit indices were used to select the fitted model. The lowest values on AIC, BIC, and aBIC indicate the preferred model [36]. Higher value of entropy indicates a better fit with the cutoff of 0.80 or higher reflecting better classification accuracy [37]. The significant p values of Lo–Mendell–Rubin likelihood ratio test (LMR-LRT) and bootstrapped likelihood ratio test (BLRT) signify a better fit of the κ-class model than the (κ-1)-class model [17]. Considering spurious groups and overextraction, profiles with a small number of members with less than 5% of the sample will be excluded [38]. In the final step, we adopted equality tests of means across classes using the BCH procedure with 3 degree(s) of freedom for the overall test to compare differences across latent profile in the continuous outcome variables (bedtime procrastination and sleep disturbance). All the statistical analyses were analyzed in Mplus 8.3 and SPSS 25.0. A two-tailed probability value of < 0.05 was considered statistically significant.
3. Results
3.1. Descriptive Statistics and Correlations of Studied Variables
The results of descriptive statistics and correlations of studied variables are presented in Table 1. Nighttime-specific smartphone use and smartphone addiction were positively related to bedtime procrastination and sleep disturbance (p < 0.01).
| Variables | 1 | 2 | 3 | 4 |
|---|---|---|---|---|
| 1. Nighttime-specific smartphone use | 1 | 0.543∗∗ | 0.589∗∗ | 0.211∗∗ |
| 2. Smartphone addiction | 0.543∗∗ | 1 | 0.478∗∗ | 0.228∗∗ |
| 3. Bedtime procrastination | 0.589∗∗ | 0.478∗∗ | 1 | 0.348∗∗ |
| 4. Sleep disturbance | 0.211∗∗ | 0.228∗∗ | 0.348∗∗ | 1 |
| M | 24.02 | 34.21 | 27.61 | 18.96 |
| SD | 6.57 | 10.27 | 6.36 | 6.06 |
- Note: M = mean.
- Abbreviation: SD = standard deviation.
- ∗∗p < 0.01.
3.2. Latent Profile Analysis of Nighttime-Specific Smartphone Use and Smartphone Addiction
The model fit indices for solutions with one to five latent profiles of nighttime-specific smartphone use and smartphone addiction by LPA (see Table 2). Specifically, as the number of profiles increased, the value of AIC, BIC, and aBIC decreased. Due to the entropy values with greater than 0.80, models are good classification precision for two-, three-, four-, and five-profile selection. The LMR and BLRT were statistically significant for the two-profile, three-profile, and four-profile models. However, the results of LMR-LRT for 5-profile was not significant, indicating that the 4-profile solution fit the data better than the 5-profile solution. Finally, the four latent profiles were considered the optimal model.
| Model | AIC | BIC | aBIC | Entropy | LMR-LRT (p value) | BLRT (p value) |
|---|---|---|---|---|---|---|
| 1 profile | 116965.471 | 117156.774 | 117048.754 | — | — | — |
| 2 profile | 107511.663 | 107804.245 | 107639.037 | 0.900 | < 0.001 | < 0.001 |
| 3 profile | 103147.727 | 103541.587 | 103319.191 | 0.927 | < 0.001 | < 0.001 |
| 4 profile | 101308.390 | 101803.528 | 101523.945 | 0.903 | < 0.001 | < 0.001 |
| 5 profile | 100180.202 | 100776.619 | 100439.848 | 0.889 | 0.519 | < 0.001 |
- Note: The bold values represent the final model.
- Abbreviations: aBIC, adjusted BIC; AIC, Akaike Information Criterion; BIC, Bayesian Information Criterion; BLRT, bootstrapped likelihood ratio test; LMR-LRT, Lo–Mendell–Rubin likelihood ratio test.
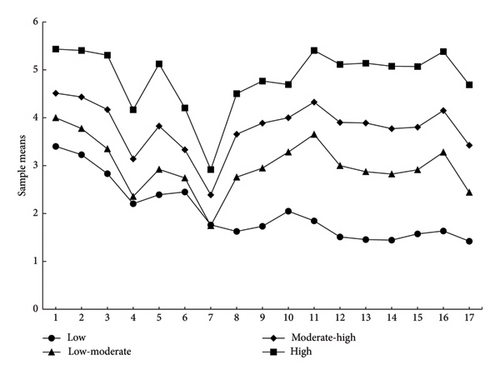
Figure 1 illustrates sample means of nighttime-specific smartphone use and smartphone addiction for each profile. Profile 1 labeled low nighttime-specific smartphone use and smartphone addiction, was characterized by low level of nighttime-specific smartphone use and smartphone addiction. This profile included 284 participants (13.8%). Similarly, based on the sample means, Profile 2, Profile 3, and Profile 4 were labeled low-moderate (n = 666, 32.5%), moderate-high (n = 845, 41.2%), and high nighttime-specific smartphone use and smartphone addiction (n = 257, 12.5%), respectively.
3.3. Proportions of Latent Profiles Across Grades
Table 3 shows the proportions of four latent profiles for nighttime-specific smartphone use and smartphone addiction in different grade groups. Juniors had the lowest proportion of low profile. Freshmen and sophomores accounted for higher proportion than other grades in low-moderate profile. Freshmen had the lowest proportion in moderate-high profile and high profile, and seniors had the highest proportion in high profile.
| Variables | Freshmen | Sophomores | Juniors | Seniors | Total |
|---|---|---|---|---|---|
| Low | 82 (28.9) | 77 (27.1) | 43 (15.1) | 82 (28.9) | 284 |
| Low moderate | 194 (29.1) | 195 (29.3) | 107 (16.1) | 170 (25.5) | 666 |
| Moderate high | 163 (19.3) | 270 (31.9) | 184 (21.8) | 228 (27.0) | 845 |
| High | 37 (14.4) | 76 (29.6) | 63 (24.5) | 81 (31.5) | 257 |
3.4. Relation of Profile Membership to Bedtime Procrastination and Sleep Disturbance
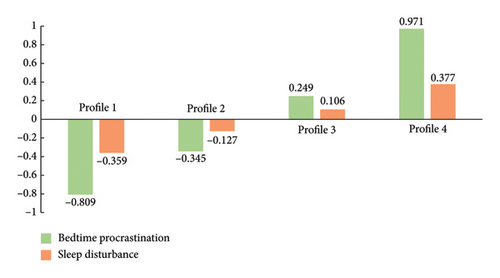
The BCH procedure (Table 4) was adopted to explore the relationship of profile membership with bedtime procrastination and sleep disturbance. Comparisons across latent profiles on the auxiliary outcome variables were conducted separately for each model. The result indicated a significant overall chi-square test for the association of profile membership with bedtime procrastination (χ2 = 657.27, p < 0.001) and sleep disturbance (χ2 = 85.33, p < 0.001). Specifically, higher levels of nighttime-specific smartphone use and smartphone addiction was correlated to severe bedtime procrastination and more sleep disturbance. Figure 2 provides a more visual representation of the relationship of latent profile memberships with bedtime procrastination and sleep disturbance.
| Variables | Profile 1 | Profile 2 | Profile 3 | Profile 4 | χ2 | Group comparison |
|---|---|---|---|---|---|---|
| Bedtime procrastination | 22.37 ± 0.38 | 25.23 ± 0.22 | 29.30 ± 0.19 | 34.00 ± 0.40 | 657.27∗∗∗ | C1 < C2∗∗∗ |
| C1 < C3∗∗∗ | ||||||
| C1 < C4∗∗∗ | ||||||
| C2 < C3∗∗∗ | ||||||
| C2 < C4∗∗∗ | ||||||
| C3 < C4∗∗∗ | ||||||
| Sleep disturbance | 16.75 ± 0.40 | 18.13 ± 0.24 | 19.65 ± 0.21 | 21.33 ± 0.43 | 85.33∗∗∗ | C1 < C2∗∗ |
| C1 < C3∗∗∗ | ||||||
| C1 < C4∗∗∗ | ||||||
| C2 < C3∗∗∗ | ||||||
| C2 < C4∗∗∗ | ||||||
| C3 < C4∗∗ | ||||||
- Note: Profile 1 (C1) represents low nighttime-specific smartphone use and smartphone addiction; Profile 2(C2) represents low-moderate nighttime-specific smartphone use and smartphone addiction; Profile 3(C3) represents moderate-high nighttime-specific smartphone use and smartphone addiction; and Profile 4 (C4) represents high nighttime-specific smartphone use and smartphone addiction.
- ∗∗ p < 0.01.
- ∗∗∗ p < 0.001.
4. Discussion
Based on a person-centered perspective, the present study examined the co-occurring patterns of nighttime-specific smartphone use and smartphone addiction, as well as the association of latent profile memberships with bedtime procrastination and sleep disturbance. This study revealed four distinct latent profiles for nighttime-specific smartphone use and smartphone addiction using LPA. The results better disentangled the nature and heterogeneity of the patterns of nighttime-specific smartphone use and smartphone addiction among medical students. We have identified distinct differences in latent profile memberships related to bedtime procrastination and sleep disturbance, which in turn offers significant support for the development of interventions designed to mitigate problematic smartphone use among medical students.
Our results align with previous studies that have identified a significant link between smartphone addiction and nighttime smartphone use [12]. However, our study contributes to the existing literature by identifying four distinct profiles of nighttime-specific smartphone use and smartphone addiction, which helps to disentangle the complexity of these behaviors. Different from previous studies that distinguished between individuals with exclusive smartphone addiction and those who solely use smartphones at night, our results primarily aligned with the concept that smartphone addiction often co-occurs with nighttime smartphone use. The high profile, characterized by the highest levels of both nighttime-specific smartphone use and smartphone addiction, comprised 12.5% of the sample. The moderate-high profile accounted for the largest proportion of participants (41.2%), comprising primarily of medical students who exhibited moderate nighttime smartphone use while demonstrating high levels of addiction to smartphones. Early identification and prevention of high-risk smartphone use patterns are essential to minimize the negative effects among medical students. Potential interventions could be tailored to the different latent profiles identified in our study. These interventions may range from educational programs and counseling sessions to mobile app-based tools and self-help resources.
Our findings revealed that a higher percentage of senior students belonged to the high-risk profile compared with other grades, indicating that they are more prone to excessive nighttime smartphone use and addiction. This finding is consistent with the general strain theory, which posits that individuals may use smartphones to cope with stressful events, thereby leading to addictive behaviors [39]. Senior medical students, who are exposed to the clinical environment, face immense pressure, stemming not only from the acquisition of clinical knowledge and skills but also from the demands and expectations of faculty members and patients. To relieve pressure, they may be more likely to develop nighttime smartphone addiction than younger students in lower grades. Results indicated that sophomores made up the greatest percentage of individuals who fell into the moderate-high profile. Prior research has concluded that sophomores are most likely to engage in uncontrolled smartphone use [40], a finding that supports the phenomenon of “sophomore slump” [41]. Compared with freshmen, second-year medical students were more likely to exhibit a diminished sense of professional identity and a certain level of academic burnout, both of which were positively correlated with smartphone addiction [42].
A pivotal finding of our research reveals that medical students with four distinctive profile patterns exhibited diverse traits with regards to bedtime procrastination and sleep disturbance. Specifically, those with higher nighttime-specific smartphone use and smartphone addiction were significantly associated with more severe bedtime procrastination. This finding is consistent with previous research showing that individuals who are more addicted to smartphones report higher levels of bedtime procrastination and poor sleep quality [13]. According to the temporary motivation theory [43], whether a person procrastinates depends on the perceived benefit of the task. For individuals with smartphone addiction, the allure of instant gratification and psychological fulfillment from nighttime smartphone use often significantly outweighs the benefits of a good night’s sleep. This not only supports the notion that nighttime smartphone use contributes to bedtime procrastination but also offers insights into how bedtime procrastination is intricately linked to specific patterns of smartphone usage.
In line with previous study [22, 23, 26, 44], we also found that higher levels of nighttime-specific smartphone use and smartphone addiction were correlated with more sleep disturbance. These patterns may contribute to sleep disturbance through several mechanisms. One possible mechanism is that nighttime smartphone use may disrupt brain activity, especially the pineal gland, whose melatonin secretion is inhibited [45–47]. This inhibition thereby disturbs the circadian rhythms. Moreover, direct exposure to blue light from smartphones may also inhibit melatonin production. Another possible mechanism is that smartphone use may induce individuals’ emotional or physiological arousal, thereby prolonging sleep latency and leading to sleep disturbance [48]. Individuals with high levels of smartphone addiction are more likely to use their smartphones uncontrollably before bedtime, resulting in sleep disturbance [13]. Understanding patterns of smartphone use may have the potential to facilitate earlier diagnosis and treatment of individuals with sleep disturbance [49]. More interestingly, prior research has revealed that limiting smartphone usage during nighttime can significantly improve sleep quality [50]. Therefore, both imposing limitations on nighttime smartphone use and discouraging excessive smartphone use are effective strategies to mitigate smartphone-induced sleep problems.
4.1. Practical Implications, Limitations, and Strengths
Our findings inform future research and practice. Future studies are encouraged to further explore the causal relationships between nighttime-specific smartphone use, smartphone addiction, bedtime procrastination, and sleep disturbance. In addition, interventions targeted at the different latent profiles identified in our study could be developed and tested to mitigate problematic smartphone use among medical students. Specifically, the identification of a high-risk group comprising 12.5% of medical students underscores the need for targeted interventions and heightened attention to these subgroups. Furthermore, evaluating problematic smartphone use among medical students and adopting targeted measures to mitigate its detrimental effects are imperative. Among these measures, limiting nighttime smartphone use duration stands out as an effective approach to alleviate the smartphone-related sleep disturbances. In addition, grade-specific interventions should be developed, accounting for the varying patterns of such usage across different academic years, particularly for higher grades. Moreover, the study found a positive link between nighttime-specific smartphone use and addiction with bedtime procrastination and sleep disruption. This underscores the urgency of adopting suitable measures to address these sleep-related concerns stemming from problematic smartphone usage.
This study faces several limitations that are crucial to acknowledge. First, the sample was exclusively drawn from a single medical college located in Shanxi Province, China, potentially limiting the generalizability of our findings. Future studies should incorporate a more diverse and representative sample. Second, relying on self-reported measures introduces potential unreliability due to recall biases or inaccuracies. Lastly, the cross-sectional nature inherently limits our ability to establish a causal relationship between latent profile memberships and bedtime procrastination or sleep disturbance. Longitudinal approach tracking students over an extended period wounld enable a more rigorous examination of the studied relationships.
Despite these limitations, our study underscores the importance of adopting a person-centered approach to examine nighttime-specific smartphone use and smartphone addiction among medical students. In contrast to the variable-centered method, this approach prioritizes the individual perspective, yielding a more intricate understanding of the behaviors and patterns related to smartphone use. Our findings significantly contribute to the comprehension of the characteristics associated with nighttime-specific smartphone use and addiction, as well as their correlation with bedtime procrastination and sleep disturbance. Notably, our study is among the few to employ a person-centered approach to investigate this crucial relationship. As revealed by our research, the coexistence and heterogeneity of these behaviors enable the development of tailored intervention strategies. By acknowledging the diverse patterns and needs of individual students, more effective interventions can be designed to target subgroups or individuals. Furthermore, our findings offer valuable guidance and provide a justification for preventing excessive nighttime smartphone use and addiction among medical students.
5. Conclusion
This study demonstrated the overlap and heterogeneity of nighttime-specific smartphone use and smartphone addiction in medical students. LPA was used to divide the subjects into four distinct latent profiles: low, low-moderate, moderate-high, and high profiles. Medical students in senior grades tend to have high levels of nighttime-specific smartphone use and smartphone addiction. More importantly, the latent profile memberships were positively associated with bedtime procrastination and sleep disturbance. Early detection of the patterns of nighttime-specific smartphone use and smartphone addiction could be an effective strategy to prevent sleep-related problems among medical students. Interventions should be tailored to prevent problematic smartphone use among medical students, especially for those in higher grades.
Ethics Statement
This study was approved by the Ethics Committee of the School of Public Health, Shandong University (LL20210102). All participants who participated had signed an electronic informed consent form.
Conflicts of Interest
The authors declare no conflicts of interest.
Funding
This research was supported by the Natural Science Foundation of Shandong Province (ZR2022QB030).
Supporting Information
Supporting Table S.1 shows the basic characteristics of the included participants.
Open Research
Data Availability Statement
The data that support the findings of this study are available from the corresponding author upon reasonable request.