Effects of Transcatheter Arterial Embolization for Chronic Intractable Shoulder Pain: A Prospective Clinical Study
Abstract
Objectives: Based on the idea that the neovessels and nerves are a possible cause of pain, transcatheter arterial embolization (TAE) has been reported as a novel adjunctive treatment with good outcomes. Purpose of this was to examine the short-term outcomes of TAE including 1-day follow-up results in patients with chronic shoulder pain using patient-reported outcome measures.
Study Design: Prospective study.
Methods: TAE was performed with a suspension of imipenem/cilastatin sodium in contrast agent. Subjects were assessed before, 1 day after, and 1 month after the procedure using the visual analogue scale (VAS, 0–10), shoulder pain and disability index (SPADI, 0–100), and Constant–Murley score (CMS, 0–100).
Results: A total of 10 patients were enrolled. All procedures were technically successful with the radial artery approach. Abnormal neovessels with angiographic blushes were identified in all cases, with a mean of 3.3 abnormal neovessels per patient (range, 2–4) and a total of 41 arteries embolized, averaging 4.1 vessels per patient (range, 3–5). Baseline VAS, SPADI, and CMS were 3.5, 50.0, and 47.4, respectively. The 1-day follow-up (VAS, 2.0; SPADI, 26.3; CMS, 68.1; p ≤ 0.001 compared to baseline) and 1-month follow-up (VAS, 1.7; SPADI, 24.3; CMS, 72.8; p ≤ 0.002 compared to baseline) demonstrated significant improvements. The 1-day and 1-month follow-up results were not significantly different.
Conclusions: Substantial pain relief and functional scales improvement were observed both immediately and 1 month after TAE in chronic intractable shoulder pain. TAE may be an effective alternative treatment for patients with shoulder pain who do not respond to conservative or surgical treatment.
Trial Registration: Korean Registry of Clinical Trials: KCT0004720
1. Introduction
Chronic shoulder pain is one of the most common musculoskeletal disorders, with an annual cumulative incidence of 2.4% for adults aged 45–64 years [1]. It can cause upper extremity dysfunction that limits the ability to perform activities of daily living (ADL). Moreover, it is associated with high medical costs [2]. Thus, it is an important medical as well as socioeconomic problem that can result in a low quality of life.
There are a variety of diseases that cause shoulder pain, including rotator cuff injury, adhesive capsulitis, glenohumeral osteoarthritis, tendinitis, and bursitis. Since chronic shoulder pain is commonly multifactorial, [2, 3] various treatment strategies are used. Physical therapy is the standard treatment for chronic shoulder pain, which includes heat therapy, cryotherapy, hydrotherapy, electrotherapy (transcutaneous electrical nerve stimulation, iontophoresis, interferential current, and microcurrent), and other alternative therapies (intramuscular stimulation, vibration, laser therapy, and extracorporeal shock wave therapy) [4–7]. Injection therapy is commonly used as adjunctive treatment, including prolotherapy, intraarticular injection, stem cell injection, and platelet-rich plasma injection [8–12]. Although various methods have been implemented for chronic shoulder pain, there are still many patients who are refractory to these conservative treatments. Adjunctive treatment using a different approach is needed for these patients.
Transcatheter arterial embolization (TAE) has been reported as a novel adjunctive treatment with good outcomes [13, 14]. Based on the idea that neovessels and nerves are a possible cause of pain, Okuno et al. proposed TAE to reduce chronic shoulder pain by blocking neovessels [15]. Since their first study, good short-term and mid-term results have been reported [16, 17]. Nevertheless, up to now, short-term outcomes within a month after TAE rarely have been reported. Only one study has reported postoperative day 1 outcomes, but that study showed no significant pain reduction; in addition, no functional assessment was performed [18]. Therefore, the purpose of our study was to examine short-term pain and functional outcomes of TAE, including 1-day follow-up results, in patients with chronic shoulder pain using patient-reported outcome measures.
2. Materials and Methods
This prospective study was approved by the Institutional Review Board of Korea (number: 2019-09-039). All subjects provided written informed consent and were given a detailed explanation of the study, its purpose, and any potential ethical issues. The study was conducted in accordance with the Declaration of Helsinki.
2.1. Subjects
All patients were selected by a multidisciplinary team that included rehabilitation physicians, an orthopedic surgeon, and an interventional radiologist. The screening evaluation, based on a medical history and physical examination, was completed during the first visit. Inclusion criteria for patients were: (1) age over 19; (2) persistent shoulder pain refractory to conservative treatment, including pharmacologic treatment, corticosteroid injection, and physiotherapeutic treatment; (3) diagnosis of rotator cuff tendinopathy with or without calcific tendinitis as the primary indication for embolization; and (4) ability to accurately express the degree and location of their pain. Exclusion criteria for patients were: (1) suspicion of cervical radiculopathy during physical examination; (2) shoulder surgery within the last 6 months; (3) injection and/or ESWT procedures within the 1 month; (4) inability to stop taking anticoagulants before the procedure; (5) chronic kidney disease with GFR (ml/min/1.73 m2) less than 30 (stages 4-5); (6) allergy to contrast agent; (7) uncontrolled diabetes mellitus; and (8) pregnant and lactating, positive urine test for pregnancy, or planning pregnancy during the study period. If a patient was eligible for TAE, target sites were marked through physical examination and ultrasound examination on the first day of admission.
2.2. Outcome Measures
The visual analogue scale (VAS, subjective pain scale) was used as the primary efficacy endpoint. The VAS is a scale of 0 to 10, with 0 indicating no pain and 10 indicating the most severe pain [19]. As secondary endpoints, the shoulder pain and disability index (SPADI) and Constant–Murley score (CMS) were evaluated. SPADI is a useful index for assessing SPAD. It has a total of 13 items, 5 related to pain (SPADI-pain: the worst, when lying on side with pain, when lifting arm to reach for high-shelf objects, when catching back of the neck, and when pushing something with pain in arm), and 8 related to physical disabilities (SPADI-disability: when washing the face or back, when wearing underclothes or a jacket, when wearing a shirt with buttons in the front, when wearing trousers, when placing something on a high shelf, when carrying a heavy object, and when taking something out of the back pocket) [20]. The more severe the pain and disability, the higher the SPADI score.
CMS has a total of 100 points, including pain severity (CMS-pain), ADL (CMS-ADL), range of motion (ROM) (CMS-mobility), and muscle strength of the shoulder joint (CMS-strength) [21]. CMS and symptoms are inversely proportional; a lower score indicates the patient suffers from the most severe pain and cannot perform daily activities. It consists of simple and intuitive questions the patient can easily answer. CMS is a widely used scoring system that includes measuring ROM. Pain and ADL scores are recorded using Likert scales in the CMS. The mobility score is calculated by checking the pain-free range of elevation, and strength is calculated by measuring maximal withstanding force to weights measured at 90° lateral abduction of the arm. The time needed to complete the CMS test is only between 5 and 7 min. It is a very intuitive and easy tool for both patients and clinicians.
2.3. Embolization Procedure
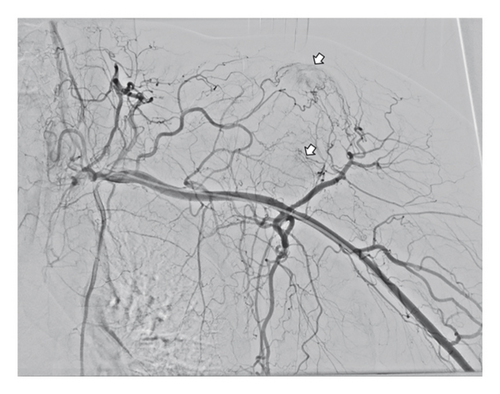
A physical examination of marked sites was performed to identify target areas prior to TAE. Under local anesthesia, ultrasound-guided radial artery access of the ipsilateral side was gained using a 5–F introducer sheath (Prelude; Merit Medical Systems, Inc, Utah, USA). Selective catheterization of the subclavian artery and digital subtraction angiography was performed to depict abnormal neovessels (Figure 1). According to previous reports [15, 17, 18], an ill-defined area of enhancement in the joint capsule during the arterial phase with variable early venous drainage (i.e., “angiographic blush”) was considered to be an abnormal neovessel. In addition, a feeder to the painful area on physical examination was considered pathologic despite an absence of abnormal neovessels. Superselection of these abnormal vessels was performed using a 2.0-F swan-neck-designed microcatheter (Pursue; Merit Medical Systems, Inc, Utah, USA). After superselection, angiographies were carried out with slow manual injection of contrast media to confirm the location of the catheter tip for embolization.
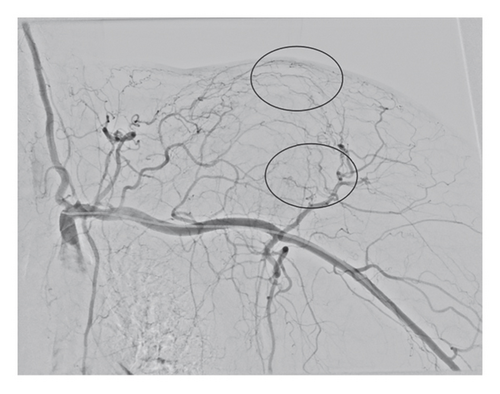
A mixture of 500 mg IPM/CS with 7 mL of iodinated contrast agent (Visipaque 270; GE Healthcare, NJ, USA) was infused until there was complete stasis of blood flow. Repeat angiography was performed to determine successful embolization. Embolization was also performed on painful areas even in the absence of a visible pathologic arterial blush, provided the pain site corresponded with the target vessel. Technical success was defined as superselective catheterization and embolization of at least 1 feeding artery to the abnormal neovessels. Hemostasis was achieved by applying an external compression device (PreludeSYNC Radial Compression Device; Merit Medical Systems, Inc, Utah, USA).
All patients were asked to provide answers regarding their VAS, SPADI, and CMS at 1 day after TAE before discharge and at 1 month after TAE. Adverse events were recorded according to the classification by the Society of Interventional Radiology [22].
2.4. Statistical Analysis
Statistical analysis was performed using SPSS ver.22 for Windows (SPSS Inc., Chicago, IL, USA). Repeated measures analysis of variance (RM-ANOVA) was performed to compare primary and secondary outcome variables. Data that do not follow a normal distribution were analyzed using Friedman’s test. Statistical significance was set at p < 0.05. Variables that were found to be significantly different in the RM-ANOVA underwent a post hoc analysis using a paired t-test. Data that were not normally distributed were analyzed using the Wilcoxon signed-rank test. p < 0.05 was considered statistically significant.
3. Results
3.1. Subjects
A total of 12 patients signed informed consent to participate between June 2020 and March 2022. One patient did not meet the eligibility criteria due to being unable to discontinue anticoagulant use, and one patient voluntarily withdrew. Thus, 10 patients were enrolled and treated by TAE. There were 8 women and 2 men. The mean age was 59.4 ± 12.4 years old. The mean VAS before TAE was 3.5 ± 0.9. The mean SPADI was 50.0 ± 18.4 (SPADI-pain, 24.6 ± 4.9; SPADI-disability, 25.4 ± 14.8). The mean CMS was 47.4 ± 17.0 (CMS-pain, 6.0 ± 2.4; CMS-ADL, 7.6 ± 3.2; CMS-mobility, 21.8 ± 5.8; CMS-strength, 12.0 ± 9.7). The etiologies of shoulder pain were rotator cuff tendinopathy with (n = 6) or without (n = 4) calcific tendinitis.
3.2. Procedural Outcome
One interventional radiologist with more than 5 years of experience in TAE performed all the procedures. All procedures were technically successful using the radial artery approach without conversion to the femoral approach. The abnormal neovessels with angiographic blushes were identified in all procedures. The mean number of abnormal neovessels was 3.3 (range, 2–4). All abnormal neovessels were successfully embolized by superselection. The mean number of embolized vessels was 4.1 (range, 3–5). Vascular findings and embolized vessels are summarized in Table 1. Abnormal neovessels were found from feeders of the thoracoacromial artery in 10 of 10 (100%), anterior circumflex humeral artery in 6 of 10 (60%), posterior circumflex humeral in 6 of 10 (60%), suprascapular artery in 4 of 10 (40%), circumflex scapular artery in 2 of 10 (20%), and coracoid branch of the subclavian artery in 5 of 10 (50%) patients. Embolized vessels included the thoracoacromial artery in 10 of 10 (100%), anterior circumflex humeral artery in 7 of 10 (80%), posterior circumflex humeral in 10 of 10 (100%), suprascapular artery in 7 of 10 (70%), circumflex scapular artery in 2 of 10 (10%), and coracoid branch of the subclavian artery in 5 of 10 (50%) patients. The mean procedure time was 77.2 ± 21.5 min.
| Target artery | Patients with abnormal neovessels | Embolized vessels |
|---|---|---|
| Thoracoacromial artery | 10/10 (100) | 10/10 (100) |
| Anterior circumflex humeral artery | 6/10 (60) | 7/10 (80) |
| Posterior circumflex humeral artery | 6/10 (60) | 10/10 (100) |
| Suprascapular artery | 4/10 (40) | 7/10 (70) |
| Circumflex scapular artery | 2/10 (20) | 2/10 (20) |
| Coracoid branch of the subclavian artery | 5/10 (50) | 5/10 (50) |
- Note: Numbers in parentheses means percentage.
3.3. Pain and Shoulder Functional Scores
No patient reported increased pain after TAE. At 1-day follow-up, all patients showed improvement in VAS, SPADI-pain, and CMS-pain compared to baseline. Likewise, at 1-month follow-up, all patients showed improvement in VAS, SPADI-pain, and CMS-pain compared to baseline (Figure 2). However, one patient showed worse SPADI-pain and CMS-pain at 1 month compared to 1-day follow-up; one patient showed a worse CMS-pain score compared to 1-day follow-up; and one patient showed worse SPADI-pain compared to 1-day follow-up.

Regarding shoulder disability scores compared to baseline, all patients showed improved SPADI-disability at 1 day, while nine patients showed improved SPADI-disability at 1 month. One patient showed a decline in SPADI-disability between the 1-day and 1-month follow-ups. For CMS-ADL scores, 7 of 10 patients showed improvement at 1 day and 9 of 10 patients showed improvement at 1 month. For CMS-mobility scores, all patients showed improvement at 1 day and 9 of 10 patients showed improvement at 1 month. For CMS-strength scores, 9 of 10 patients showed improvement at 1 day and all patients showed improvement at 1 month (Figure 2).
In the total score, all patients showed improvement in SPADI at 1 day, while nine patients showed improvement in SPADI at 1-month follow-up compared to baseline. Two of those 9 patients showed a decline in 1-month SPADI compared to 1-day follow-up. All patients showed an improved CMS at 1-day and 1-month follow-ups compared to baseline. Three patients showed a decline in CMS at 1-month follow-up compared to 1-day follow-up.
Significant differences were observed in mean VAS, SPADI, and CMS between baseline, 1-day, and 1-month scores in an ANOVA test. CMS-strength scores at 1-day and 1-month follow-ups were not significantly different from baseline. Results are summarized in Table 2.
| Baseline | 1 day after TAE | 1 month after TAE | p value: baseline vs. 1 day | p value: baseline vs. 1 month | p value: 1 day vs. 1 month | |
|---|---|---|---|---|---|---|
| VAS | 3.50 ± 0.85 | 2.00 ± 1.33 | 1.70 ± 1.25 | 0.001+ | 0.002+ | 0.616+ |
| SPADI score | ||||||
| Pain | 24.60 ± 4.90 | 12.30 ± 7.75 | 11.50 ± 6.40 | < 0.001+ | < 0.001+ | 0.767+ |
| Disability | 25.40 ± 14.77 | 14.00 ± 12.34 | 12.80 ± 9.89 | 0.005++ | < 0.001+ | 0.236++ |
| Total score (sum/130∗100) | 38.46 ± 14.15 | 20.23 ± 14.98 | 18.69 ± 12.32 | < 0.001+ | < 0.001+ | 0.731+ |
| Constant-murley score (overall) | ||||||
| Pain | 6.00 ± 2.40 | 10.40 ± 2.84 | 11.00 ± 1.70 | < 0.001+ | < 0.001+ | 0.394+ |
| ADL | 7.60 ± 3.20 | 11.50 ± 4.30 | 13.70 ± 3.20 | 0.002+ | 0.015+ | 0.187+ |
| Mobility | 21.80 ± 5.81 | 27.90 ± 7.16 | 28.60 ± 7.17 | 0.003+ | 0.005+ | 0.466+ |
| Strength | 12.03 ± 9.67 | 18.27 ± 11.44 | 19.45 ± 12.05 | 0.072+ | 0.140+ | 0.136+ |
| Total score | 47.43 ± 17.01 | 68.07 ± 15.67 | 72.75 ± 18.39 | < 0.001+ | 0.001+ | 0.155+ |
- Abbreviations: ADL = activities of daily living, SPADI = shoulder pain and disability index, TAE = transarterial embolization, VAS = visual analogue scale.
- +Paired t-test.
- ++Wilcoxon signed rank test.
3.4. Complications
Immediate complications at 1-day follow-up occurred in 3 of 10 patients (30%) as follows: nausea in 1 patient, puncture site pain in 1 patient, and a transitory change in forearm skin color in 1 patient. All complications were well tolerated and spontaneously resolved within 1 day after TAE without prolonged hospitalization. There were no delayed complications.
4. Discussion
In this study cohort, TAE was performed in patients with refractory shoulder pain that persisted after at least 1 month of conservative treatment including injection treatment. There were no major complications. Pain reduction was demonstrated at 1-day follow-up in all patients and was maintained for almost all patients up to a month after TAE. In addition, there was a significant improvement in 1-day functional outcomes, including disability, ADL, mobility, and shoulder strength, which persisted for almost all patients up to a month after TAE.
One of the most remarkable aspects of our study is the significant improvement observed as early as one day post-embolization. To date, one-day results have been reported in only one study. Hwang et al. [18] found no statistically significant change in VAS scores at one-day follow-up. In contrast, our data showed that one-day results were not only significant but also highly correlated with 1-month outcomes, with no statistically significant differences between VAS scores or SPADI and CMS categories at these two time points. This rapid positive effect aligns with findings in other studies that demonstrated substantial pain relief within the 1-week and sustained improvement by 1-month. Okuno et al. [23] reported that 67% of patients experienced a 50% or greater reduction in pain at 1-week, increasing to 87% by 1-month. Similarly, Martinez et al. [17] reported that median VAS decreased from 8 to 4 at 1-week, and further to 3 at 1-month. Our finding suggests that 1-day follow-up may be a reliable, early indicator of TAE’s efficacy, offering a valuable measure for short-term assessment without added complications between the 1-day and 1-month intervals.
One plausible reason our study demonstrated significant improvement as early as one day postembolization is the thorough embolization of multiple arteries supplying the shoulder joint. In our study, the average number of embolized vessels was 4.1, compared to only 1–2 vessels in Hwang’s study. Embolizing multiple arteries likely enhanced the treatment’s effectiveness by reducing abnormal vascularization linked to chronic inflammation. Although embolization of multiple vessels might raise concerns about ischemic complications, studies on IPM/CS suggest a favorable safety profile. Yamada et al. [24] demonstrated that IPM/CS particles predominantly dissolve within 48 h postembolization, allowing for recanalization while maintaining reduced blood flow and minimized ischemic risk. Additionally, a rat model study indicated that TAE with IPM/CS decreased both microvessel density and inflammation, which are contributors to pain in joint pathologies [25]. Given these findings, our approach of targeting multiple arteries with IPM/CS may increase efficacy without adding risk for complications, allowing for both rapid and sustained symptom relief. Since the target arteries typically exceed four on average, a sufficient amount of IPM/CS solution may be required. Therefore, we used 7 mL of iodinated contrast agent in our study to ensure an adequate volume for embolization of all target vessels, which typically require 1–3 mL per vessel.
While most studies used VAS as the primary endpoint, as pain relief is the chief goal of TAE, functional outcome has been evaluated as well in recent studies. Martinez et al. [16, 17] and Okuno et al. [23] evaluated ROM, and Okuno et al. additionally used the EuroQol-5D (EQ-5D) for quality of life. However, while ROM can indicate stiffness, it may not be appropriate for all painful shoulder syndromes, such as tendinopathy, where a broader functional assessment is needed. Furthermore, the measurement of ROM is a complex and physician-oriented examination that is time-consuming and potentially biased as well. A simple, standardized patient-reported scoring systems, like SPADI and CMS, offer useful alternatives for evaluating TAE outcomes in the shoulder joint. The SPADI, a 13-item, patient-completed tool, assesses shoulder pain and disability, with lower scores indicating less disability. CMS, another widely used scoring system, includes ROM, pain, ADL, mobility, and strength assessments, and can be completed in 5 to 7 min. By using SPADI and CMS, our study provided a comprehensive measure of disability, pain, and quality of daily life, demonstrating that TAE improves not only pain but also functional outcomes such as ROM and muscular strength in the shoulder joint.
This study has several limitations. First, the sample size was small. This prospective study was designed to confirm the efficacy of TAE in 24 patients based on previous results. However, there were difficulties in patient enrollment due to the coronavirus pandemic. The coronavirus pandemic also prevented patients from returning to the office; thus, mid-term results were not available in many patients. Although we did not reach our target sample size, the efficacy of TAE was confirmed with statistical significance in both 1-day and 1-month follow-ups. Second, there was an absence of a control group. In the future, further studies aiming at comparing the efficacy of TAE and other treatments are needed. Third, this study used IPM/CS, which is not widely used for non-musculoskeletal embolization. The usefulness of other commercially available embolic materials, such as gelfoam or microspheres, is unclear. Fourth, although statistical significance was not found between 1-day and 1-month follow-ups, there was 1 patient who showed aggravation in SPADI and CMS scores during the interval. This implies that early recurrence already occurred before the 1-month follow-up, particularly in that IPM/CS is an absorbable embolic material, which is known to remain in an embolized vessel only for a few hours to days. Further studies are warranted to investigate the relationship between early recurrence and affecting factors, including the type of embolic materials. Additionally, the necessity of the 1-day follow-up as a short-term outcome besides the 1-month follow-up should be validated.
5. Conclusion
Substantial pain relief and functional scales improvement were observed both immediately and 1 month after TAE in chronic intractable shoulder pain. TAE may be an effective alternative treatment for patients with shoulder pain who do not respond to conservative or surgical treatment.
Ethics Statement
This study was approved by the Institutional Review Board of Jeonbuk National University Hospital (number: 2019-09-039).
Consent
All eligible patients provided written informed consent.
Conflicts of Interest
The authors declare no conflicts of interest.
Funding
This research was supported by the Bio&Medical Technology Development Program of the National Research Foundation (NRF) funded by the Korean Government (MSIT) (No. RS-2023–00236157) and by grants from the Biomedical Research Institute of Jeonbuk National University Hospital, Jeonju, Korea.
Open Research
Data Availability Statement
The datasets generated and/or analyzed during the current study are available from the corresponding author on reasonable request.