Major Etiologies of Male Infertility Among Couples Attending Fertility Clinics in Osun State, Nigeria: Findings From a Mixed-Method Study
Abstract
Male infertility accounts for nearly half of the infertility cases globally. Seminal fluid analysis (SFA) is a critical diagnostic tool in the evaluation of male infertility. This study aimed to assess the implications of SFA on male infertility among patients attending fertility clinics in Osogbo, Nigeria. The study employed a mixed-method approach of both qualitative (key informant interview [KII]) among 10 participants and quantitative methods (cross-sectional survey) using a pretested structured questionnaire among 305 respondents. The respondents in the cross-sectional survey were also made to undergo SFA. The data from the qualitative study were analyzed using ATLAS.ti, while the data from the quantitative study were analyzed using IBM Statistical Product for Service Solution (SPSS) version 27.0. Descriptive statistics was carried out for all variables. The univariate, bivariate, and multivariate analyses were done using p < 0.05 as the level of significance. The SFA of the respondents revealed that 241 (79.0%) had normal sperm counts (> 32 million per ejaculation), while 64 (21.0%) had abnormal sperm counts. Only 101 (33.1%) had sperm cells with normal progressive motility (> 32%), while 204 (66.9%) had abnormal (Athenospermia) progressive motility. One hundred and ninety-five (63.9%) were found to have abnormal morphology (Teratospermia, i.e., < 4%). The analysis of the data from the KII further explained the implications of SFA parameters on infertile males, and these were substantial, extending beyond physical health to encompass psychological, emotional, and social well-being. The study concluded that lifestyle modifications, early diagnosis, and prompt treatment of medical conditions can help reduce the high prevalence of SFA abnormalities and, consequently, decrease male infertility in our environment. This study recommends that advocacy programs, early screening, and public health education will further reduce the burden of infertility among the men.
1. Introduction
Seminal fluid plays a crucial role in the fertilization process, providing a supportive environment for sperm transport, nourishment, and protection against the female reproductive tract’s hostile conditions [1]. Seminal fluid analysis (SFA) is a critical diagnostic tool in the evaluation of male infertility. It involves the examination of various semen parameters, such as sperm concentration, motility, morphology, and seminal plasma composition, to assess a man’s fertility potential [2]. Male infertility accounts for nearly half of the infertility cases globally [3]. In Southwest Nigeria, there is limited research on the SFA and its implications on male infertility among patients attending fertility clinics. Investigating this relationship can help identify factors contributing to infertility in this region and inform the development of targeted interventions to improve reproductive outcomes for affected couples. Understanding the connection between SFA findings and male infertility could have significant implications for clinical practice, public health policies, and patient counseling. Therefore, this study aimed to assess the implications of SFA on male infertility among patients attending fertility clinics in Osogbo, Nigeria.
2. Materials and Methods
This study employed a mixed-method approach of both qualitative (key informant interview [KII]) among 10 participants and quantitative methods (cross-sectional survey) among 350 respondents. The study population for the quantitative study was male patients attending fertility centers in Osogbo, Osun State, while participants for the qualitative study were some wives of the infertile male patient and specialized experts in male fertility, including nurses, and medical practitioners working in fertility clinics located in Osogbo. Fisher’s formula (n = z2 pq/d2) was used to determine the sample size. The respondents for the quantitative study were selected using the multistage sampling technique; at the first stage, five centers were randomly selected out of the 10 major fertility centers in Osogbo. The names of the fertility centers are as follows; UNIOSUN Teaching Hospital Osogbo, Halleluyah Specialist Hospital, Osogbo, Ayomide Fertility Center, Osogbo, SW Aqua Fertility Center, and Crystal Medical and Specialist Center. At stage two, proportional allocation was used to determine the number of respondents from each center. The total number of infertile male from the five centers was 1510; to get the number to be selected in each center, the total infertile males from each center was divided by the total number from the five centers, multiplied by the calculated sample size. At stage three, male patients aged 18–50 years were randomly selected in each center.
Data were collected from the respondents of the quantitative study using a pretested interviewer-administered questionnaire written in English language. A pilot study was carried out with a limited sample size to evaluate the questionnaire’s reliability, which was carried out at the University College Hospital, Gynecological Clinic, Ibadan, among 10% of total sample size (31) participants, and the internal consistency of the questionnaire was assessed through the utilization of Cronbach’s alpha. After informed written consent had been obtained from the participants and the details of the study had been explained to them, the questionnaire was administered by research assistants and the health workers in the fertility centers used in the study. The questionnaire contained questions about the sociodemographic characteristics of respondents, lifestyle, and medical history of the respondents. After which the semen of the respondents who agreed to participate in the study were collected by the laboratory technicians in the diagnostic laboratory of each fertility center under sterile conditions after an abstinence period of 2–7 days using sterilized universal bottles, following WHO procedures [2]. This was carried out in a private room near the laboratory in order to reduce the exposure of the semen to fluctuations in temperature and to control the time between collection and analysis. The semen was then analyzed for sperm count, motility, and morphology. The study was carried out over a period of nine months from September, 2023, to May, 2024.
The respondents were selected for a qualitative study using a purposive sampling technique. Data were collected by trained research assistants through the utilization of KIIs. A semistructured KII guide was used, while voice recording was also done which was later analyzed using a thematic content analysis approach. All information gathered was confidential, and privacy and confidentiality of the respondents in both quantitative and qualitative study were guaranteed.
The data from the questionnaire were analyzed using IBM Statistical Product for Service Solution (SPSS) version 27. Descriptive statistics was used for all variables. Bivariate and multivariate analyses were done at p < 0.05 as the level of significance.
3. Results and Discussion
3.1. Results
3.1.1. Quantitative Study
3.1.1.1. Sociodemographic Characteristics
All the respondents were married male attending the infertility clinic in Osogbo. More than half, 204 (58.3%), of the respondents were within the ages of 30–45 years, while the majority, 333 (95.4%), were Yoruba. Two hundred and twenty-two (63.6%) had tertiary level of education. More than half, 207 (59.0%), were skilled workers.
3.1.1.2. SFA of Male Patients Attending Fertility Center
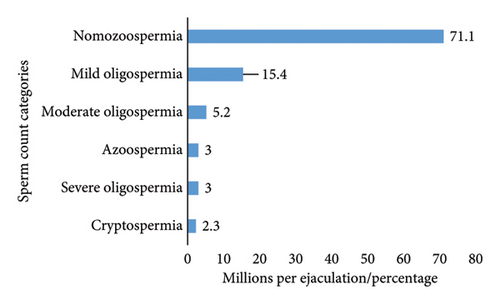
Majority of the respondents, 249 (71.0%), had normal sperm count (> 32 million per ejaculation), while 101 (29.0%) had abnormal sperm count in different categories (Figure 1). Only 116 (33.1%) had normal progressive motility (> 32%), while 234 (66.9%) had abnormal (Athenospermia) progressive motility. Two hundred and twenty-four (63.9%) were found to have abnormal morphology (Teratospermia, i.e., < 4%) (Table 1). Overall, 321 (91.8%) of the respondents had at least one abnormality in the semen analysis.
| Variables | Frequency (n = 305) | Percentage |
|---|---|---|
| Sperm count | ||
| Abnormal (> 32 million) | 88 | 28.9 |
| Normal (< 32 million) | 217 | 71.1 |
| Progressive motility | ||
| Normal (> 32%) | 101 | 33.1 |
| Abnormal/athenospermia (< 32%) | 204 | 69.9 |
| Morphology | ||
| Normal (> 4%) | 110 | 36.1 |
| Abnormal/teratospermia (< 4%) | 195 | 63.9 |
| Culture of any organism | ||
| No | 305 | 100.0 |
3.1.2. Qualitative Study
3.1.2.1. Sociodemographic Characteristics of Participants
The participants’ ages ranged from 25 to 44 years. There were 10 participants in the qualitative study, six participants were female and four were male. Seven participants were married and three were single. The predominant ethnicity was Yoruba, with one participant being Nupe. Five participants were Christian and five were Muslim. Educational status varied with three participants having tertiary education, two with Higher National Diploma (HND), one with Senior Secondary School Examination (SSCE), and four with an unspecified level of education. The participant types included three wives married to husbands who are infertile patients, four nurses, and three doctors (Table 2).
| Code | Age range (yrs) | Gender | Marital status | Ethnicity | Religion | Edu. status | Participant type | Years of working experience |
|---|---|---|---|---|---|---|---|---|
| N1 | 36–40 | F | Married | Yoruba | Muslim | SSCE | Wife | NA |
| N2 | 36–40 | M | Married | Yoruba | Christian | Tertiary | Doctor | 10 |
| N3 | 31–35 | F | Married | Yoruba | Christian | HND | Nurse | 5 |
| N4 | 41–45 | F | Married | Yoruba | Muslim | Tertiary | Nurse | 13 |
| N5 | 25–30 | F | Single | Nupe | Christian | Tertiary | Doctor | 1 |
| N6 | 36–40 | F | Married | Yoruba | Christian | Tertiary | Nurse | 10 |
| N7 | 25–30 | M | Single | Yoruba | Christian | Tertiary | Doctor | 3 |
| N8 | 31–35 | F | Married | Yoruba | Muslim | NS | Wife | NA |
| N9 | 41–45 | F | Married | Yoruba | Christian | Tertiary | Wife | NA |
| N10 | 36–40 | M | Single | Yoruba | Muslim | Tertiary | Doctor | 5 |
- Abbreviations: F = female; M = male.
3.1.2.2. Causes of Male Infertility
“I think the lifestyle is one of the main causes, like smoking, taking alcohol, having multiple sexual partners which can predispose them to sexually transmitted infections” … N1. “I think um the causes are diabetes, hypertension as well as obesity there are also risk factors like smoking and alcoholism… and some other dangerous lifestyles like having multiple sexual partners” N2. “I would say maybe smoking and alcohol” … N7. “It can cause by maybe disease” … N5.
“Well, it could be due to infections. Like we were told that in childhood, especially maybe a male child that was infected with mumps. If the mumps is not well treated, it could lead to infertility in future. And, it could be due to sexually transmitted infections that are not well treated” … N4, … “This may be the one contracted during the bad habit of promiscuity by ether the male or female… and thereby causing infertility” … N8
“Well, I think there are different causes of infertility: Ranging from genetics to lifestyle could affect the patient … N6. It can be genetically motivated or it medical related causes…” N10
“Yes, I think lifestyle. like a male that is having so many sexual partners could lead to infections, and if it’s not treated, it could lead to infertility” … N4. “Yes, I think yes, social life is causing it. Social life that can bring a lot of infections and some infections can cause infertility in men” … N5. “Smoking… Alcohol intake”… N6, … “yes like engagement in drinking of alcohol, smoking etc.”…N7. “Most of the times, this infertility is caused by lifestyle factors including smoking, alcohol consumption…” N10.
3.1.2.3. Medical Illness Causing Male Infertility
“I know of diabetes, hypertension, but I’m not sure I have heard obesity being a cause of male infertility…N5. …Obesity…N2, I think especially sexually transmitted infections can cause it…N4. “Some underlying medical conditions such as diabetes, varicocele, that could also cause infertility” …N7 “I really can’t say” …N1. I heard the infections from usually from extra-marital affairs causes it… N9.
3.2. Discussion
This study assessed the major etiologies of infertility among couples attending fertility clinics in Osogbo, Osun State, Nigeria. More than half of the respondents were between the ages of 30 and 45 years. More than half of the respondents had tertiary education as their highest educational attainment, and the same proportion were skilled workers. This is similar to the findings of another study conducted among male partners attending an infertility clinic in a tertiary Nigerian hospital where 50.2% were within the ages of 35–44 years [4] but not in tandem with those of a study on SFA in west Ethiopia that reported more (45.8%) of their participants to be within 25–30 age bracket [5].
The findings of this study revealed that seven out of 10 respondents had Normozoospermia, i.e., normal number of sperm counts. This is lower than the findings in the study of Tilahun et al. [5] on SFA in Ethiopia, where more than nine out of 10 respondents had Normozoospermia. However, the result of this study is higher than the findings in a study among the same study population in Sokoto, Northern Nigeria, which reported that just a little above half of the respondents had Normozoospermia [4].
Overall, about nine out of 10 participants had at least one abnormality in their SFA; about seven out of 10 had abnormal progressive motility and three-fifth had abnormal morphology in their semen. This is similar to the findings of Umar et al. [4], where about four-fifth of the respondents were reported to have at least one abnormality in their SFA. A similar study carried out in Port-Harcourt, Nigeria, revealed that four-fifth of the respondents seeking medical assistance for fertility had at least one abnormality in their semen parameters [6]. Similarly, a study conducted in Lagos University Teaching Hospital revealed that more than seven out of 10 respondents had abnormal semen parameters with more than half having abnormal progressive motility [7]. This indicates that abnormality in seminal fluid parameters could be an indication or underlying factor for infertility among men.
The findings of the qualitative analysis in this study assessed the causes of male infertility. The majority referred to certain lifestyles, such as smoking and alcohol consumption, as well as medical conditions, as major contributors to male infertility. This was supported by the findings of Durairajanayagam [8] in a review of lifestyle causes of male infertility. He reported that smoking of cigarettes, drinking alcohol, and medical condition such as obesity are significantly associated with male infertility. Virtually, all the respondents believed that male infertility could be caused by medical conditions. This is in tandem with the submission made by Palmer et al. [9] in his study on the impact of obesity on male fertility and sperm function. Also, the participants noted that having multiple sexual partners that may expose men to STIs can contribute to infertility. This is supported by the findings of Shaker et al. [10], who revealed that HSV infection had a negative impact on seminal fluid parameters among infertile male patients.
4. Conclusion
The findings indicate a prevalence of abnormal seminal fluid parameters (low sperm count, motility, and morphology) among the participants. Lifestyle choices were commonly cited as contributors to infertility, with participants highlighting the detrimental effects of habits such as smoking, STI, and alcohol consumption on reproductive health. In addition, lifestyle factors, including habitual smoking, STI, and alcohol consumption, were recognized as potential predictors of abnormality in SFA and male infertility.
The study recommends advocacy programs focussed on modification of lifestyles for all male and early diagnosis and treatment of medical conditions among men.
Ethics Statement
Ethical approvals for this study were obtained from the Ethics and Research Committee of Uniosun Teaching Hospital. The protocol number is UTH/EC/2024/06/957. All ethical principles guiding the conduct of the research such as informed consent, beneficence, nonmaleficence, confidentiality, justice, and autonomy were strictly taken into consideration. All information gathered was confidential, and privacy and confidentiality of the respondents were guaranteed. All respondents were made to sign the informed consent before filling the questionnaire.
Disclosure
A preprint version has previously been published with reference number MEDRXIV/2024/311725 [11].
Conflicts of Interest
The authors declare no conflicts of interest.
Funding
The authors received no funding for the study.
Acknowledgments
The authors wish to acknowledge the respondents who gave their consent to be part of this study as well as the head of the facility centers for their permission during the course of this study.
Open Research
Data Availability Statement
The data for this study are available on reasonable request from the corresponding author.