The Impact of Hand Edema on Weaning From Mechanical Ventilation in ICU Patients: A Single Center Nested Case-Control Study
Abstract
Objective: To investigate the impact of hand edema on weaning from mechanical ventilation among ICU patients.
Methods: A nested case-control study was conducted, collecting data from mechanically ventilated patients admitted to the ICU of Wuxi People’s Hospital from October 1, 2023, to January 31, 2024. Patients were monitored for the occurrence of hand edema within the first 7 days of ICU stay and their weaning outcomes were recorded to analyze the impact of hand edema on weaning success.
Results: The study included 124 patients, 97 successfully weaned while 27 failed. The failed weaning group had higher ages (70.8 ± 10.5 years), SOFA scores (17.7 ± 3.1), and levels of hand edema (Grade 0 in 6 patients, Grade 1 in 9, Grade 2 in 6, Grade 3 in 3, and Grade 4 in 3) compared with the successful weaning group (ages 61.1 ± 9.8 years, SOFA scores 14.3 ± 3.1, hand edema levels: Grade 0 in 78, Grade 1 in 15, Grade 2 in 3, Grade 3 in 1, and Grade 4 in 0). Multivariable binary logistic regression analysis indicated that the level of hand edema is an independent risk factor for weaning failure within 1 week in ICU patients on mechanical ventilation (OR = 3.209, 95% CI: 1.641–6.274, and p < 0.05).
Conclusion: The occurrence of hand edema in ICU patients on mechanical ventilation increases the risk of weaning failure.
1. Introduction
Edema has long been recognized as a poor prognostic indicator in critical illnesses, consistently correlating with adverse outcomes across a wide range of disease processes [1]. Peripheral edema typically arises from several interrelated pathophysiological mechanisms, including elevated capillary hydrostatic pressure, reduced plasma colloid osmotic pressure, increased capillary permeability, and impaired lymphatic drainage [2]. In critically ill patients, edema can significantly contribute to respiratory failure through its effects on alveolar diffusion, ventilation-perfusion mismatch, and decreased lung compliance [3, 4]. Various forms of pulmonary edema—such as alveolar edema, interstitial edema, pleural effusion, and chest wall edema—exacerbate respiratory dysfunction by impairing gas exchange and disrupting pulmonary mechanics. Common underlying causes of edema in the ICU setting include heart failure, renal failure, volume overload, hypoalbuminemia, and infections. Critically ill patients in the ICU, especially those with severe conditions, frequently experience a combination of these factors, all of which contribute to the development and progression of edema [5]. This complex interplay of factors further complicates the weaning process from mechanical ventilation, often delaying recovery and prolonging critical care [6–15].
Peripheral edema is a common manifestation of edema, and as the most directly observable form, it is frequently encountered in ICU patients. Notably, hand edema is more prevalent than lower limb edema in the ICU setting [16], and it can be easily detected at the bedside. However, the specific impact of hand edema on the weaning process from mechanical ventilation in critically ill patients remains unclear. To address this gap in the literature, this study utilizes a nested case-control design to investigate the potential role of hand edema in influencing the weaning process.
2. Methods
2.1. Inclusion Criteria
Patients on mechanical ventilation admitted to the ICU of Wuxi People’s Hospital between October 1, 2023, and January 31, 2024.
2.2. Exclusion Criteria
Patients were excluded if they presented with hand edema upon ICU admission, had one or both hands missing, had venous thrombosis in the upper limbs, had upper limb trauma or skin soft tissue infections, used restraints improperly (when restraining hands, it is advisable to put two fingers in. For patients who need long-term restraint protection, the restraint should be relaxed every 2-3 h to avoid prolonged local compression), were admitted with a tracheostomy, or left the ICU while still on mechanical ventilation within 7 days.
2.3. Experimental Methods
2.3.1. Patient Data Collection and Weaning Success Criteria
The severity of bilateral hand edema was monitored daily for the first 7 days. For patients who left the ICU within this period, measurements were taken until the day of departure. The highest recorded level of edema during this period was considered the patient’s edema level. Patients who remained free from mechanical ventilation support for 48 h after weaning were categorized as successfully weaned; others, including deceased patients, were classified as weaning failures.
2.3.2. Hand Edema Assessment Method
-
0 points—no edema.
-
Ultrasound characteristics: normal echogenicity of subcutaneous tissues with no signs of fluid accumulation.
-
Tissue structure: clear visibility, good continuity, no separation, or abnormal gaps.
-
1 point—Mild edema.
-
Ultrasound characteristics: slight fluid accumulation, with a few areas of hypoechoic regions.
-
Tissue structure: largely normal, but with small fluid gaps that generally do not disrupt the overall tissue continuity.
-
2 points—Moderate edema.
-
Ultrasound characteristics: obvious fluid accumulation, with more prominent hypoechoic areas.
-
Tissue structure: tissue separation begins, with widened fluid gaps visible across a larger area.
-
3 points—Severe edema.
-
Ultrasound characteristics: extensive fluid accumulation, with hypoechoic areas widely distributed.
-
Tissue structure: significant disruption of tissue continuity, with large and extensive fluid gaps involving most of the examined area.
-
4 points—Very severe edema.
-
Ultrasound characteristics: extreme fluid accumulation, nearly the entire scanning area appears hypoechoic.
-
Tissue structure: subcutaneous tissue structures are almost indiscernible, with very wide fluid gaps due to extensive fluid accumulation.
2.4. Statistical Methods
Statistical analyses were performed using SPSS 18.0. Quantitative data were expressed as the mean ± standard deviation and categorical data as the median (interquartile range). Group comparisons for quantitative data were conducted using the t-test, while categorical data comparisons utilized nonparametric tests (including chi-square and U tests). A binary logistic regression analysis was used to assess the impact of edema level on weaning outcomes.
3. Results
3.1. Patients
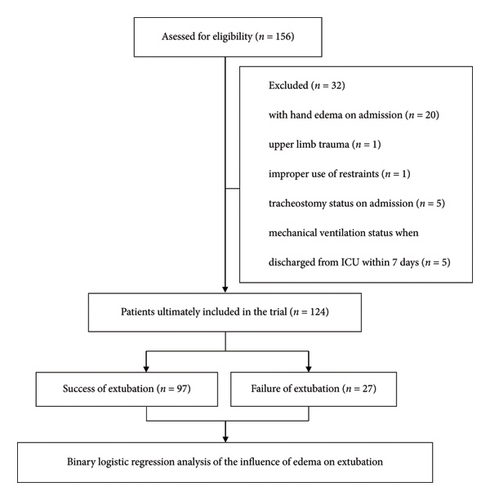
A total of 156 patients met the inclusion criteria. Exclusions were made for patients presenting with hand edema upon admission (20 patients), upper limb injuries (1 patient), improper use of restraints (1 patient), tracheostomy at admission (5 patients), and those who left the ICU while still on mechanical ventilation within 7 days (5 patients). Ultimately, 124 patients were included in the study. The enrollment flowchart is shown in Figure 1. The cohort consisted of 60 males and 64 females with an average age of 63.2 ± 10.7 years and an average SOFA score of 15.1 ± 3.4. Diagnoses included sepsis (38 patients), pneumonia (34 patients), abdominal infections (29 patients), heart failure (13 patients), and others (10 patients). See Table 1 for details.
| Total | Successful weaning group | Failed weaning group | X2/U/t | p | |
|---|---|---|---|---|---|
| N | 124 | 97 | 27 | / | / |
| Gender (male/female) | 60/64 | 47/50 | 13/14 | 0.035 | 0.849 |
| Age (years) | 63.2 ± 10.7 | 61.1 ± 9.8 | 70.8 ± 10.5 | 4.487 | < 0.001 ∗ |
| SOFA score | 15.1 ± 3.4 | 14.3 ± 3.1 | 17.7 ± 3.1 | 4.885 | < 0.001 ∗ |
| Diagnosis | 1.202 | 0.878 | |||
| - Sepsis | 38 | 28 | 10 | / | / |
| - Pneumonia | 34 | 26 | 8 | ||
| - Abdominal infection | 29 | 24 | 5 | ||
| - Heart failure | 13 | 11 | 2 | ||
| - Other | 10 | 8 | 2 | ||
| Hand edema grade (n (%)) | 468.0 | < 0.001 ∗ | |||
| 0 | 84 (67.7%) | 78 (92.9%) | 6 (7.1%) | / | / |
| 1 | 24 (19.4%) | 15 (62.5%) | 9 (37.5) | ||
| 2 | 9 (7.3%) | 3 (33.3%) | 6 (66.7%) | ||
| 3 | 4 (3.2%) | 1 (25.0%) | 3 (75.0%) | ||
| 4 | 3 (2.4%) | 0 (0%) | 3 (100%) |
- Note: Gender and diagnosis were analyzed using the chi-square test; age and SOFA score were analyzed using univariate t-tests; hand edema grading was analyzed using the Mann–Whitney U test.
- ∗p < 0.05 indicates statistically significant differences.
3.2. Weaning Outcomes Analysis
3.2.1. Comparison Between Successful and Failed Weaning Groups
Of the 124 patients included in the study, 97 were successfully weaned while 27 failed to wean. The successfully weaned group consisted of 47 males and 50 females, with an average age of 61.1 ± 9.8 years and an average SOFA score of 14.3 ± 3.1. Diagnoses in this group included sepsis (28 patients), pneumonia (26 patients), abdominal infections (24 patients), heart failure (11 patients), and other conditions (8 patients). The distribution of hand edema grades in the successfully weaned group was as follows: Grade 0 in 78 (92.9%) patients, Grade 1 in 15 (62.5%), Grade 2 in 3 (33.3%), Grade 3 in 1 (25%), and Grade 4 in none (0%). In contrast, the group that failed to wean included 13 males and 14 females, with an average age of 70.8 ± 10.5 years and an average SOFA score of 17.7 ± 3.1. Their diagnoses were sepsis (10 patients), pneumonia (8 patients), abdominal infections (5 patients), heart failure (2 patients), and other conditions (2 patients). Hand edema grades in the failed weaning group were Grade 0 in 6 (7.1%) patients, Grade 1 in 9 (37.5%), Grade 2 in 6 (66.7%), Grade 3 in 3 (75%), and Grade 4 in 3 (100%). Statistical analysis revealed that the successfully weaned group had significantly lower ages, SOFA scores, and hand edema grades compared with the failed group (p < 0.05), indicating statistically significant differences. Specific test values and p values are detailed in Table 1.
3.2.2. Multivariable Binary Logistic Regression Analysis of Factors Affecting Weaning Outcomes
In the comparison between groups, significant differences were observed in patient age, SOFA scores, and hand edema grades. Consequently, a binary logistic regression analysis was conducted to assess the impact of gender, age, and hand edema grade on weaning outcomes. The results indicated that age, SOFA score, and hand edema grade are independent risk factors for weaning failure within 1 week in ICU patients on mechanical ventilation. Specific B values, p values, odds ratios, and 95% confidence intervals are provided in Table 2.
| Variable | B | p | OR | 95% CI |
|---|---|---|---|---|
| Age | 0.062 | 0.040 ∗ | 1.063 | 1.003–1.128 |
| SOFA | 0.224 | 0.030 ∗ | 1.251 | 1.022–1.529 |
| Edema grade | 1.166 | 0.001 ∗ | 3.209 | 1.641–6.274 |
- Note: Binary logistic regression analysis was performed using SPSS 18.0, with successful weaning coded as 0 and failure as 1. B,the regression coefficient.
- Abbreviations: CI, confidence interval; ORs, odds ratio.
- ∗p < 0.05 indicates statistically significant differences.
4. Discussion
This study corroborates previous findings that age and SOFA scores are predictors of weaning failure, aligning with earlier research [15, 17–20]. However, through multivariable binary logistic regression analysis, hand edema was identified as an independent risk factor for weaning failure within 7 days in ICU patients on mechanical ventilation. An increase of one grade in edema level was associated with a 220% increase in the risk of weaning failure. This underscores the importance of recognizing hand edema as a significant risk factor in mechanically ventilated patients.
Hand edema in ICU patients represents one manifestation of peripheral edema, which is frequently associated with poor prognosis [1]. The causes of peripheral edema are varied, including heart failure, renal failure, volume overload, hypoalbuminemia, and infections. The complexity of weaning failure is similarly multifaceted, involving the respiratory tract, lungs, heart, kidneys, diaphragmatic function, endocrine system, and metabolism [3]. Heart failure is a significant cause of weaning failure, not only due to systolic dysfunction [21] but also as ventricular diastolic dysfunction becomes increasingly common in ICU patients experiencing weaning failure [22]. The issue of fluid balance is crucial, being a common cause of difficult weaning and weaning failure [12, 13], with studies like that of Ghosh S et al., finding that a cumulative fluid balance exceeding 3490 mL increases the risk of extubation failure by 119.1% [11]. Maintaining a positive fluid balance after extubation also predisposes to failure [23, 24] and exacerbates cardiac diastolic dysfunction, further leading to weaning failure [25]. Moreover, renal dysfunction is another key factor affecting weaning in critically ill patients [7], especially as fluid balance increases the risk of weaning failure in patients with acute kidney injury [26]. Sepsis and septic shock also significantly contribute to weaning or extubation failure [9, 10, 27], with large fluid balances increasing the risks of weaning failure and mortality in patients with septic shock [14]. Research by Bruells and Marx suggests that sepsis also impacts diaphragmatic stability, leading to weaning failure [28].
Our findings indicate that hand edema adversely affects weaning, suggesting that minimizing edema in mechanically ventilated patients could potentially improve weaning success rates. Conservative fluid resuscitation can significantly improve oxygenation, shorten the duration of mechanical ventilation, and reduce ICU stay [8]. Studies by Silversides JA et al. have shown that achieving a stepped fluid balance reduction by the third day of ICU admission can improve outcomes in critically ill patients [24]. During specific stages of weaning from mechanical ventilation, a randomized controlled trial demonstrated that a fluid removal strategy guided by plasma B-type natriuretic peptide measurements significantly shortened the duration of mechanical ventilation, particularly in patients with left ventricular dysfunction [29]. Achieving a negative fluid balance before starting a spontaneous breathing trial may reduce the risk of cardiogenic weaning failure [29–31].
Pulmonary edema is a common cause of difficult weaning or weaning failure, with studies by Liu et al. [31] and Bedet et al. [32] showing that nearly 60% of weaning failures are associated with pulmonary edema. Mustafi et al., using B-lines to assess extravascular lung water, found that increased extravascular lung water significantly lengthens weaning duration, mechanical ventilation days, ICU stay, and overall mortality [33]. The relationship between hand edema and pulmonary edema was not explored in this study, which is a limitation. In this study, deceased patients were classified as weaning failures. While death represents an irreversible outcome, the factors leading to death (such as uncontrolled shock and malignant arrhythmias) often overlap with the mechanisms underlying weaning failure. Therefore, including deceased patients in the weaning failure group helps provide a comprehensive assessment of weaning outcomes in critically ill patients. However, it is important to acknowledge that the death of these patients may be influenced by other factors that are not directly related to the weaning process, which could introduce potential bias. Further limitations of our study include its single-center design and the limited number of cases and conditions; the specific physiological mechanisms linking edema to weaning failure still require further investigation. Future research should consider including more physiological and biochemical markers, such as lung compliance, lung water, and inflammatory markers, to analyze in detail how edema impacts weaning.
Nevertheless, this study highlights the critical importance of assessing and managing edema in ICU patients on mechanical ventilation. This has significant clinical implications for shortening the duration of mechanical ventilation, improving patient outcomes, and reducing healthcare costs.
5. Conclusion
The occurrence of hand edema in ICU patients on mechanical ventilation adversely affects weaning outcomes.
Conflicts of Interest
The authors declare no conflicts of interest.
Funding
This work was supported by Taihu-Talent Project of Wuxi Government (2021THRC-TD-ZZYXK-2021).
Acknowledgments
The authors have nothing to report.
Open Research
Data Availability Statement
The data used to support the findings of this study are available on request from the corresponding author.