Comparison of the Optical Biometry Based on Swept-Source Optical Coherence Tomography and Ultrasound-Based Biometry Device in Patients With Mature Cataract
Abstract
Objectives: To compare the agreement and reliability values between an optical biometry based on swept-source optical coherence tomography (OCT) (IOLMaster 700; Carl Zeiss, Germany) and an ocular ultrasound-based biometry device (Nidek; US-4000 Echoscan, Japan) for axial length (AL), anterior chamber depth (ACD), and lens thickness (LT) measurements.
Methods: In this cross-sectional study, 101 eyes of 101 consecutive patients with mature cataract underwent routine eye examinations. Then, ocular biometry measurements through optical biometry and contact ultrasound biometry were carried out. The intraclass correlation coefficient (ICC) for reliability and Bland–Altman plots for the agreement between the mean findings of the two devices were analyzed.
Results: The mean age of patients was 61.6 ± 13.1 (range, 27–94) years. For AL, the mean differences were small (0.10 mm), but with a very strong correlation and excellent agreement (r = 0.999, ICC = 0.999, p < 0.001) between the two devices. Similarly, for ACD, the correlation was very high with excellent reliability (r = 0.958, ICC = 0.974, p < 0.001), though the ultrasound biometer reported a slightly deeper mean ACD (by 0.13 mm). For LT, the agreement and correlation were lower (r = 0.508, ICC = 0.663, p < 0.001), with the optical biometer reporting a thicker mean LT (0.31 mm) than the ultrasound biometer.
Conclusion: AL and ACD measurements from the optical biometry based on swept-source OCT and ultrasound can be used interchangeably in patients with mature cataract. However, LT measurements from the two devices should not be considered interchangeable.
1. Introduction
Advancements in phacoemulsification cataract surgery have transformed the procedure from a vision restoration operation to a refractive surgery aimed at minimizing postoperative refractive error and maximizing spectacle independence [1, 2]. Achieving optimal refractive outcomes relies upon calculating the correct intraocular lens (IOL) power based on precise preoperative biometric measurements, particularly axial length (AL), anterior chamber depth (ACD), and lens thickness (LT) [3–5].
Traditionally, ocular ultrasound A-scan technology was utilized to quantify AL and ACD, albeit with limitations arising from operator dependency and the potential for corneal compression errors [3, 6]. Beginning in 1999, noncontact optical biometry was introduced via the IOLMaster (Carl Zeiss, Germany), purportedly offering superior reproducibility and accuracy compared to ultrasound [7, 8]. Optical biometry modalities such as partial coherence interferometry measure ocular dimensions using invisible near-infrared light instead of ultrasound waves [9].
While establishing optical biometry as the new “gold standard,” early validation studies still demonstrated equivalency between skilled ultrasound versus optical techniques [10–13]. However, initial IOLMaster versions encountered difficulties precisely measuring eyes with dense cataracts or other intraocular opacities impeding adequate signal acquisition [14, 15]. Newer swept-source optical coherence tomography (SS-OCT) integrated biometers such as the IOLMaster 700 (Carl Zeiss, Germany) aim to surmount prior limitations through enhanced imaging capabilities [16, 17].
Despite advantages, the higher costs and specialized equipment requirements of optical biometry limits widespread global accessibility, whereas ultrasound remains prevalent in resource-constrained settings due to lower expenses and practitioner skill [18]. When optical technology proves unavailable, establishing measurement concordance allows confidently substituting one modality’s values for the other [19]. However, few studies have explicitly assessed parameter agreement between newer optical versus ultrasound biometry, especially in dense cataracts necessitating surgery [20, 21]. On the other hand, a recently published study reported that when the quality of optical biometry measurements is low, some parameters may not be interchangeable with ultrasound due to poorer agreement [22]. Therefore, the purpose of this study was to evaluate the agreement between IOLMaster 700 optical biometry and US-4000 Echoscan ultrasound for AL, ACD, and LT measurements in patients with mature cataracts scheduled for surgery. Comparatively assessing biometric findings from both techniques may validate their interchangeable usage and support either approach reliably guiding preoperative planning.
2. Methods
2.1. Study Design and Participants
This prospective comparative study was conducted at Farabi Eye Hospital, Tehran, Iran. The ethical committee of Tehran University of Medical Sciences approved the research protocol (IR.TUMS.FNM.REC.1402.036), which adhered to the tenets of the Declaration of Helsinki. Written informed consent was obtained from all participants prior to enrollment.
The study included 101 eyes of 101 consecutive patients presenting for routine cataract surgery. Inclusion criteria specified a clinical diagnosis of mature cataract necessitating extraction as determined by a fellowship-trained ophthalmologist. Mature cataract was defined as totally opacified lens matter with poor or absence of red reflex [23].
Exclusion criteria comprised any prior ocular surgery (e.g., refractive surgery), trauma, presence of retinal pathologies (e.g., detachment), or other ocular comorbidities potentially impacting biometric measurement accuracy (e.g., lens subluxation and corneal opacity).
2.2. Clinical Examinations
All patients underwent a comprehensive ophthalmic examination including measurement of uncorrected distance visual acuity (UDVA) and best-corrected distance visual acuity (BCVA) using a Snellen chart, objective refractive error determination using a Topcon KR-800 autorefractor (Tokyo, Japan), slit-lamp biomicroscopy, and dilated fundus examination, when possible, through clear media. B-scan ultrasonography (Nidek Echo Scan Model US-4000, Gamagori, Japan) was additionally performed to exclude retinal abnormalities in eyes with dense cataracts prohibiting fundoscopy.
Optical biometry was firstly performed on all eyes using an IOLMaster 700 swept-source OCT biometer (Carl Zeiss Meditec AG, Jena, Germany) according to the manufacturer guidelines. Three consecutive measurement sets were automatically captured and averaged, directly providing AL, ACD, LT and keratometry. In patients with mature cataract, there is a possibility that IOLMaster 700 will not be able to finalize the measurement, or do a quality measurement. So low-quality measurements with the SD value record AL > 0.027 mm, LT > 0.038 mm, and ACD > 0.021 mm were excluded [16]. Whenever all indicators were green for all measurements of a patient, they were included in the study.
Subsequently, contact A-scan ultrasonic biometry was undertaken employing a Echoscan US-4000 (Nidek Inc, Japan) by an experienced optometrist masked to optical biometry results. Ten repeated measurement sets were recorded and averaged electronically for AL, ACD, and LT values to minimize operator-induced variability, ensure procedural consistency, and enhance reliability of the contact-based technique. All examinations were conducted in the same session between 9 and 11 a.m. to control for diurnal variations.
2.3. Statistical Analysis
Statistical analysis was conducted using SPSS 24.0 software (IBM, Armonk, NY). Categorical data were summarized as frequencies and percentages. Continuous variables were analyzed for normality and reported as mean ± SD (range) as appropriate. The comparison of means between the two devices was conducted using paired-samples t-test for each biometric parameter (AL, ACD, and LT).” Intraclass correlation coefficients (ICCs) assessed reproducibility between devices. Correlation between modalities was evaluated using Pearson’s coefficient. Bland–Altman plots graphically depicted limits of agreement. Statistical significance was set at p < 0.05.
3. Results
Hundred and one eyes of 101 patients with mature cataract were included in the study. The mean age was 61.6 ± 13.1 (range, 27–94) years. Of these patients, 51 (50.5%) were males and 50 (49.5%) cases were females. All cases had BCVA equal to or less than 1.00 logMAR.
The comparison of measured AL, ACD, and LT with IOLMaster 700 optical biometer (Carl Zeiss Meditec AG, Jena, Germany) and Echoscan US-4000 ultrasound biometer (Nidek Inc, Japan) in patients with mature cataract is shown in Table 1.
| Range | Minimum | Maximum | Mean ± SD | Correlation | ICC | p value∗ | |||
|---|---|---|---|---|---|---|---|---|---|
| r | p value | ||||||||
| AL | IOLMaster 700 | 12.91 | 20.86 | 33.77 | 24.02 ± 2.18 | 0.999 | < 0.001 | 0.999 | < 0.001 |
| Ultrasound | 12.90 | 20.85 | 33.75 | 23.92 ± 2.12 | |||||
| ACD | IOLMaster 700 | 2.59 | 1.87 | 4.46 | 3.31 ± 0.44 | 0.958 | < 0.001 | 0.974 | < 0.001 |
| Ultrasound | 1.92 | 2.53 | 4.45 | 3.44 ± 0.38 | |||||
| LT | IOLMaster 700 | 3.79 | 2.41 | 6.20 | 4.25 ± 0.53 | 0.508 | < 0.001 | 0.663 | < 0.001 |
| Ultrasound | 3.16 | 1.89 | 5.05 | 3.94 ± 0.66 | |||||
- Abbreviations: ACD, anterior chamber depth; AL, axial length; ICC, intraclass correlation coefficient; LT, lens thickness; N, number; SD, standard deviation.
- ∗Paired samples t-test.
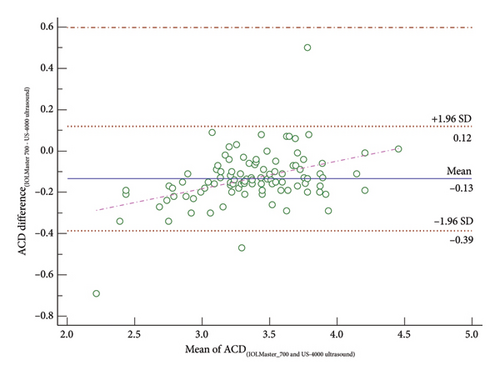
The mean values of AL with IOLMaster 700 optical biometer (Carl Zeiss Meditec AG, Jena, Germany) and Echoscan US-4000 ultrasound biometer (Nidek Inc, Japan) in patients with mature cataract were 24.02 ± 2.18 and 23.92 ± 2.12, respectively (p < 0.001). Also, the mean values of ACD with IOLMaster 700 optical biometer (Carl Zeiss Meditec AG, Jena, Germany) and Echoscan US-4000 ultrasound biometer (Nidek Inc, Japan) in these patients were 3.31 ± 0.44 and 3.44 ± 0.38, respectively (p < 0.001). In addition, the mean values of LT with IOLMaster 700 optical biometer (Carl Zeiss Meditec AG, Jena, Germany) and Echoscan US-4000 ultrasound biometer (Nidek Inc, Japan) in patients with mature cataract were 4.25 ± 0.53 and 3.94 ± 0.66, respectively (p < 0.001). Excellent agreement was observed for AL and ACD measurements, with AL demonstrating a very strong correlation (r = 0.999, ICC = 0.999, p < 0.001) and ACD also showing a very strong correlation (r = 0.958, ICC = 0.974, p < 0.001). The mean differences were small, 0.10 mm for AL and 0.13 mm for ACD, suggesting that the two devices may be used interchangeably for these parameters. In contrast, LT exhibited only moderate correlation between devices (r = 0.508, ICC = 0.663, p < 0.001), with the IOLMaster 700 consistently reporting slightly higher LT values compared to the Echoscan (mean difference: 0.31 mm).
The Bland–Altman plot comparing AL measurements from the IOLMaster 700 optical biometer and the Echoscan US-4000 ultrasound biometer can be seen in Figure 1. This figure also includes a scatter plot that compares the mean AL values obtained from these two biometers for all patients with mature cataracts. The Bland–Altman plot in this figure demonstrates a small mean difference between the two measurement techniques of 0.04 mm (p < 0.001), indicated by the solid horizontal line. This suggests that there is a negligible systematic difference on average between the devices. Moreover, the limit of agreement (95% CI), represented by the dotted lines, is narrow (0.33 mm) which confirms excellent agreement between measurements of each device.
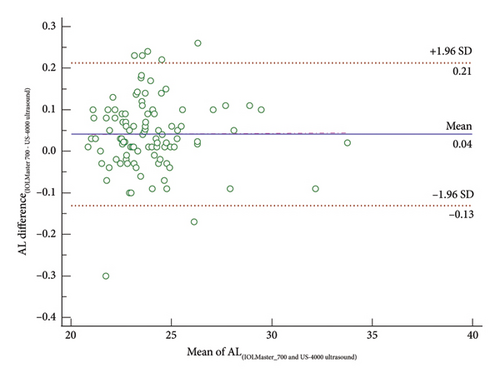
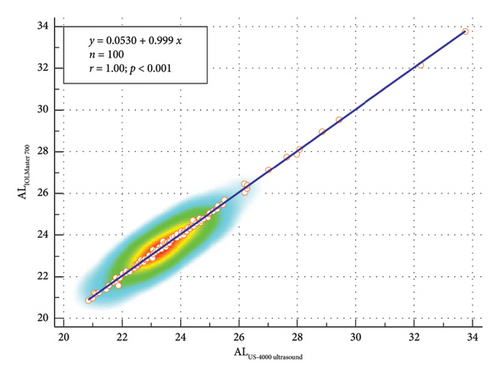
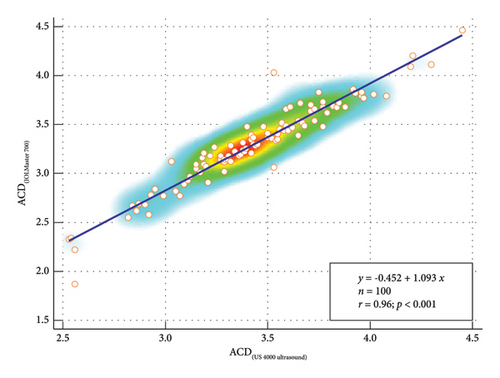
Figure 2 presents a Bland–Altman plot that compares the ACD measurements taken with the IOLMaster 700 optical biometer to those taken with the Echoscan US-4000 ultrasound biometer. In the same figure, a scatter plot illustrates the comparison of mean ACD values measured by these two biometers in all patients diagnosed with mature cataracts. The Bland–Altman plot shown in this figure demonstrates a small mean difference of 0.13 mm between the two techniques, as indicated by the solid horizontal line. This mean difference suggests that there is a negligible systematic error on average between the devices when measuring ACD. The 95% limits of agreement (dashed lines) indicate a relatively narrow band (between +0.12 and −0.39 mm). This shows a high degree of agreement between the two methods across the range of ACD measurements sampled. Additionally, the data points are evenly dispersed above and below the mean line with no apparent pattern. This implies there is no relationship between the magnitude of measurement difference and true ACD values.
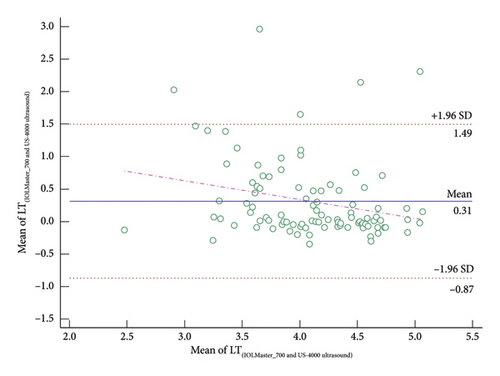
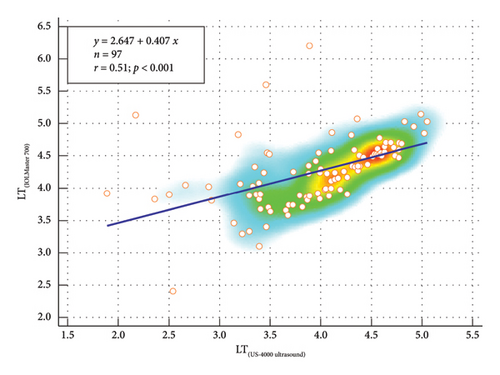
In Figure 3, a Bland–Altman plot is used to compare the LT measurements obtained from both the IOLMaster 700 optical biometer and the Echoscan US-4000 ultrasound biometer. Simultaneously, the figure includes a scatter plot that demonstrates the comparison of average LT values, as measured by these two biometers, in all patients with mature cataracts. This figure presents the Bland–Altman plot assessing agreement between LT measurements obtained using the IOLMaster 700 compared to the Echoscan US-4000. The plot depicts a mean difference of 0.31 mm between the two methods, as indicated by the solid blue horizontal line. This mean systematic variation suggests that the optical biometry typically reports slightly greater LT values. The 95% limit of agreement lies between +1.49 and −0.87 mm which indicates a moderate level of agreement across the range of LT values assessed between the two devices. Therefore, in comparison to ACD and AL, there is a larger mean difference in LT, and the Bland–Altman plot and the regression line show a moderate level of agreement for LT measurements from each technique.
4. Discussion
Ocular biometry, involving anatomical measurements of the AL, keratometry, ACD, and LT, is crucial for accurate postsurgical refractive outcomes. Various technologies are utilized to obtain precise ocular biometric measurements [24, 25]. Ultrasound and optical biometry devices are widely used, with ultrasound often preferred in developing countries due to its cost-effectiveness and familiarity. Optical devices such as the IOLMaster have higher accuracy but may face limitations in certain cases. This study aimed to compare the agreement between the IOLMaster 700 optical biometer and the Echoscan US-4000 ultrasound biometer for AL, ACD, and LT measurements in mature cataract patients. The results showed interchangeability of devices in measuring AL and ACD, while the devices’ findings were not in high agreement for LT measurements.
While the mean AL difference (0.04 mm) between the devices was statistically significant, it is clinically negligible. According to the SRK/T formula and supported by previous studies, a 0.10-mm error in AL measurement typically results in a refractive prediction error of approximately 0.25 diopters (D) [26]. Therefore, a 0.04-mm discrepancy would correspond to an estimated refractive error of around 0.10 D, which is unlikely to influence IOL selection or postoperative visual outcomes.
Regarding LT, the moderate correlation and wider limits of agreement indicate that the two devices should not be used interchangeably for this parameter. A mean difference of 0.31 mm in LT may have a more pronounced effect, particularly when using fourth-generation IOL power calculation formulas, such as Barrett Universal II, Olsen, Holladay 2, and Hill-RBF, which incorporate LT for estimating the effective lens position (ELP). Variations in LT measurements can influence ELP predictions and thus affect the accuracy of the final IOL power determination.
Several studies have compared the biometry measurements of IOLMaster with ultrasound biometry devices [21, 27]. For example, Cho et al. [28] tested 137 eyes with various severities of cataract comparing IOLMaster 700 with five different biometry devices including an ultrasound biometer (Pacscan 300A; Sonomed Inc., Chicago, IL, USA). They found that AL data of IOLMaster 700 and ultrasound biometry could be applied interchangeably, consistent with our results; however, ACD values could not be interchangeable. They reported a shorter mean ACD with contact ultrasound in comparison to noncontact optical biometry IOLMaster 700, possibly due to the inevitable corneal indentation using contact ultrasound biometry. This result is in contrast with our results in dense cataract patients with still observing an excellent level of agreement in measurement of ACD using the IOLMaster 700 optical biometer compared to the Echoscan US-4000 ultrasound biometer. In a prospective study, Nakhli investigated the relationship between the measured AL of the eye with IOLMaster v.4 optical biometer and the A-scan 1000 (Ophthalmic Technologies International, Toronto, Canada) ultrasound unit in 55 consecutive patients (68 eyes) who were referred for cataract surgery [18]. A regression formula was used to convert measurements between devices. Based on the obtained results, there was strong reproducibility (99.4%) and agreement (r = 0.987) between both devices (p < 0.001). The difference between the devices was mainly in short eyes (p = 0.031). They concluded that AL measurement with optical biometry and with ultrasound are well related. In terms of AL measurements in the present study, the Bland–Altman plot demonstrated a small mean difference of 0.04 mm between AL measurements of the two techniques. This suggests that there is a negligible systematic difference on average between the devices. In addition, the upper and lower limits of agreement (95% CI) were between +0.21 and −0.13 mm. Most data points fell within these bounds, showing a high level of agreement between the two methods across the range of AL measurements. Additionally, the data points are evenly distributed above and below the mean difference line, with no discernible pattern, implying there is no relationship between the measurement difference and the true AL. In another study by Rose et al., a comparison of AL measurement using A-scan ultrasound and Zeiss IOLMaster biometer optical system was conducted [29]. Their cross-sectional study was performed on 51 eyes of 46 patients referred for cataract surgery. On average, the AL measured by IOLMaster was 0.15 mm longer (> 0.01) compared to ultrasound biometry. Consistent with their finding, we observed that the mean value of measured AL with IOLMaster 700 optical biometer in patients with mature cataract was 0.10 mm longer than the measurement of Echoscan US-4000 ultrasound biometer (24.02 ± 2.18 mm vs. 23.92 ± 2.12 mm). They concluded that IOLMaster provides accurate AL measurement of the eye, and it is quick and easy to use, provides no contact and no risk of infection or corneal damage. We also used IOLMaster 700, however, a newer version, and agreed on their results for patients with mature cataract.
The primary strength of the present study was its high response rate. In terms of limitation, this cross-sectional study had some limitations. The most important one is lack of classification of patients based on AL and ACD. Another limitation is that we did not compare other biometer devices which calculate IOL power before cataract surgery. Also, we did not include patients with different severities of cataract or healthy noncataractous eyes. Additionally, we did not classify cataract subtypes (e.g., nuclear, posterior subcapsular, and cortical), which limits the generalizability of our findings across different cataract types and severities. Although using automated ultrasound devices or involving multiple examiners could reduce operator bias, our primary aim was to evaluate interdevice agreement under controlled conditions, rather than assessing interoperator repeatability. Another limitation is the absence of a formal sensitivity analysis or IOL power simulation, which could have provided further insight into the clinical relevance of the observed measurement differences and can be explored in future experiments. Lastly, the current study was conducted on two of the most common biometric devices, and the results may not apply to other biometric devices. To compare different eye biometric parameters between different biometric devices, more research is needed in this field.
5. Conclusions
The present study demonstrated an excellent level of agreement and correlation between measurements of AL and ACD obtained using the IOLMaster 700 optical biometer compared to the Echoscan US-4000 ultrasound biometer in patients with mature cataract. However, we observed a moderate level of agreement in measurements of LT using the IOLMaster 700 optical biometer compared to the Echoscan US-4000 ultrasound biometer in patients with mature cataract. This issue is particularly important in IOL calculation for many fourth-generation IOL formulas, including Barrett Universal II and Holladay 2, which utilize LT in the calculation.
Conflicts of Interest
The authors declare no conflicts of interest.
Funding
No funding was received for this research.
Open Research
Data Availability Statement
The data that support the findings of this study are available on request from the corresponding author. The data are not publicly available due to privacy or ethical restrictions.




