Telehealth as a Care Solution for Homebound People: Systematic Review and Meta-Analysis of Healthcare Utilization, Quality of Life, and Well-Being Outcomes
Abstract
Homebound individuals residing in community settings with severe health conditions and disabilities could arguably benefit from telehealth interventions. However, the effectiveness of telehealth compared to in-person care remains underexplored, considering the diversity of these groups. This systematic review and meta-analysis aimed to evaluate the effectiveness of telehealth in reducing healthcare utilization and improving health-related quality of life (HRQOL) and well-being in homebound populations. Adhering and expanding on a published protocol, we conducted comprehensive search across multiple databases: MEDLINE, Embase, PsycINFO, CINAHL, Cochrane Central Register of Controlled Trials (CENTRAL), Scopus, LILACS, and the Web of Science, with no restrictions on language or publication date, and experimental and quasiexperimental studies considered. Eleven independent reviewers were responsible for study selection, and three for data extraction. The methodological quality of the included studies was assessed using JBI checklists. A meta-analysis was then performed using Stata software, which reported standardized mean differences (SMDs) as the effect measure, with the quality of evidence evaluated using the GRADE approach. From an initial screening of 3289 articles, ten studies met our inclusion criteria, with eight suitable for meta-analysis. These studies encompassed data from 2245 participants. Our findings revealed that telehealth interventions significantly reduced healthcare utilization (SMD: −0.49; 95% CI: −0.76 to −0.22; p < 0.01, GRADE: low certainty), significantly enhanced HRQOL (SMD: 0.18; 95% CI: 0.01 to 0.35; p = 0.04, GRADE: moderate certainty), and significantly improved well-being (SMD: −0.31; 95% CI: −0.47 to −0.15; p < 0.01, GRADE: moderate certainty) compared to in-person care. Thus, telehealth emerges as a viable alternative to conventional care, significantly reducing healthcare utilization and enhancing both HRQOL and well-being for homebound people. These findings underscore the potential of telehealth to mitigate healthcare disparities and emphasize the need for accessible, equitable telehealth services codeveloped with end users and relevant stakeholders to save resources and maximize health outcomes for vulnerable populations in community settings.
1. Introduction
Telehealth, defined as the use of digital technologies to deliver healthcare services and information remotely, has significantly transformed medical care delivery, particularly for individuals with limited access to traditional health facilities [1]. Its application is especially vital for homebound people who, due to health conditions, disabilities, or other barriers, are unable to leave their homes [2]. These individuals often face a combination of social isolation, limited healthcare access, economic difficulties, and mental health challenges, all of which profoundly impact their health, quality of life, and well-being [3, 4]. Given these complexities, telehealth presents a promising opportunity to address the multifaceted care needs of homebound people, as traditional healthcare models are not equipped to support them effectively [2, 5]. However, a systematic investigation is necessary to determine whether telehealth can serve as a comprehensive care solution for this population, as the concept of homeboundness is not fully explored in all its dimensions worldwide.
In most countries, the size and magnitude of homebound challenges and their effects on community care management are increasing; for instance, in America, between 2011 and 2020, the prevalence of homebound adults aged 70 years or older more than doubled, with significant disparities among Hispanic/Latino and Black non-Hispanic people, who were more likely to experience poor health, lack of technology access, and crowded living conditions compared to White non-Hispanic individuals [6]. This reported increased prevalence continued in 2021 as the COVID-19 pandemic subsided, but its psychological, social, and physical effects continue to be poorly understood [6].
The COVID-19 pandemic accelerated the global uptake of telehealth to maintain care continuity and reduce in-person healthcare visits, particularly for individuals with chronic conditions [7]. In Europe, these digital transitions were generally well received by patients and providers, although most implementations were developed as short-term responses and lacked long-term integration into health systems [8]. In Japan, demographic aging prompted the expansion of telehealth as a strategy to support older adults and reduce caregiver burden through home-based remote care [9], monitoring and health education [10]. These developments reflect shared structural challenges in health systems worldwide, including social isolation, psychological distress, and increased risk of suicide among those with limited mobility or access to care [11]. Nonetheless, access to home-based care continues to be influenced by systemic and social factors, such as the configuration of social networks and family support structures [9].
Despite these advances, nationwide homebound population data remain scarce in many countries. In Australia, for example, the Australian Bureau of Statistics (ABS) does not collect or report data specific to homebound individuals [12]. However, the 2018 Survey of Disability, Ageing and Carers (SDAC) estimated that approximately 596,800 people with disabilities were unable to leave home as often as they would like. Of these, 383,500 were aged 5–64 years and 212,800 were 65 years or older [12, 13]. A more severely affected subgroup, approximately 37,700 individuals, reported never leaving their homes, including 20,000 aged 5–64 and 18,000 aged 65+, with 19,500 indicating that their inability to leave was due primarily to a disability or health condition [12].
In the absence of contemporary data, a 2020 Australian Survey was conducted to explore the experiences of frail, homebound, and bedridden people (FHBP) [14]. This study revealed a population with characteristics that significantly diverged from those commonly reported in international literature. Among the 306 respondents, the majority were women (81%), people with disabilities (72%), and individuals who either lived alone (33%) or were single (42%) [14]. Unlike traditional assumptions that homebound populations are primarily elderly, this sample was predominantly younger or middle-aged. The largest age group represented was 41–45 years (18%), followed by 46–50 and 31–35 years (13% each), then 36–40 and 51–55 years (9% each). Seven percent of participants were in each of the following age brackets: 21–25, 26–30, 56–60, and 61–65 years. A smaller number were aged 18–20 (4%) and 66–70 (3%), and only 1% were aged 71–75 or over 85 [14]. These findings challenge international trends, particularly in the United States, where research on homebound populations typically focuses on older adults and highlights risk factors such as advanced age, cognitive impairment, multimorbidity, malnutrition, and income disparity [15, 16].
The FHBP study also revealed complex health and care needs. Thirty-eight percent of respondents held a bachelor’s degree, yet 91% reported physical difficulties, 75% experienced brain or nervous system conditions, and 66% lived with three or more long-term conditions [17]. The most reported illness was myalgic encephalomyelitis/chronic fatigue syndrome (ME/CFS), affecting 78% of participants—a chronic, disabling condition that affects roughly 1% of the global population and is often poorly understood by clinicians [14, 18]. The impact on mobility was profound: 78% of respondents were unable to leave their homes most or all of the time, and 53% were confined to bed most or all of the time [14]. Furthermore, 85% of participants perceived their health as much worse than that of their peers, and 88% reported experiencing social isolation [14].
Internationally, telehealth has gained momentum as a tool for supporting homebound individuals, particularly older adults. In Southeast Asian countries such as Brunei, Cambodia, Indonesia, Laos, Malaysia, Myanmar, the Philippines, Singapore, Thailand, and Vietnam, telehealth and digital innovation are increasingly promoted to strengthen long-term care systems for aging populations [19]. Globally, research has examined telehealth in the management of cardiovascular diseases and diabetes [20, 21], Alzheimer’s disease, depression [22], and the mitigation of social isolation among older adults [23]. In some contexts, telehealth has also been positioned as a tool to reduce discrimination and address barriers to care for people with disabilities [24].
Despite these promising developments [22, 25], most existing studies focus on older adults, specific diseases, or narrow service delivery outcomes. As such, they do not adequately represent the full diversity of the homebound population, which includes younger people, as observed in the Netherlands [26], and those with complex or medically unexplained conditions [27], or individuals experiencing intersecting forms of disadvantage [28]. To date, no systematic review has evaluated the effectiveness of telehealth across all types of homebound individuals, regardless of age, diagnosis, or reason for confinement. This review addresses that critical gap by synthesizing global evidence on telehealth interventions for homebound populations of all ages and profiles.
1.1. The Research Gap: Comprehensive Solutions
Homebound individuals in Australia have actively collaborated with academics to research their unique challenges and advocate for telehealth as a critical solution to healthcare disparities [29, 30]. In 2025, telehealth access is still restricted only to people who have had an in-person consultation with their general practitioner within the preceding year, a limitation that affects the most vulnerable Australians [31], notably those homebound and bedridden because of ME/CFS, autoimmune conditions, frailty, or psychosocial ailments [29, 30]. This indicates that current policies and strategies may not adequately address the needs of these prominent groups, particularly when considering potential care solutions like telehealth [14].
Through initiatives such as the socioscientific exhibition “ENLIGHTEN” and related awareness scholarly outputs, the FHBP groups call for new models of care that use telehealth to improve health outcomes and quality of life for homebound populations [32, 33]. These efforts align with broader research on rare diseases and uncover the specific physical and mental health challenges community-based populations face globally [2, 14]. They stress the importance of investigating telehealth innovation to address the complexities of homeboundness [34, 35], especially in light of the increased risks posed by long COVID and reported growing challenges in community care related to dementia [36, 37].
The existing research on telehealth for homebound people [38] often illustrates a disease-fragmented approach, where solutions are tailored to specific conditions; therefore, there is a lack of a holistic perspective on the diverse needs of all homebound populations [6, 39]. For instance, studies focusing on telehealth interventions for younger individuals affected by hikikomori syndrome—a severe social withdrawal condition associated with suicidal thoughts, stigma, and reluctance to seek help—highlight the necessity of solutions for this group [40, 41]. However, while these studies effectively look at the unique challenges specific homebound sectors face, they often do so in isolation from broader telehealth strategies that could benefit all homebound individuals, regardless of age or condition [42, 43]. Thus, current studies may overlook the varied characteristics of the broader homebound population, narrowing the scope of the evidence. Consequently, it is necessary to produce studies encompassing a more comprehensive evaluation of telehealth to address the full spectrum of homebound’ needs according to the latest clinical trials or reproducible and generalizable findings, so the calls and feedback from those wanting new telehealth models of care can be backed up or rejected [44, 45].
This study aims to provide evidence-based insights that address the complex care needs of all homebound populations by shifting from a fragmented, disease- and age-specific perspective to a more inclusive approach. The objective is to determine whether telehealth can effectively support the fundamental care needs of homebound individuals across different life stages [46]. To ensure telehealth interventions are both effective and equitable, offering comprehensive solutions that meet the diverse needs of these communities [47, 48], an innovative method of investigation is required [30, 49], one that involves homebound individuals as coresearchers alongside clinicians and experts from various fields [29, 30]. To that end, this study integrates such a group (n = 21 coresearchers) to conduct a systematic literature review and meta-analysis of all the published literature on the topic to assess whether telehealth is a viable care solution for homebound communities overall, regardless of health conditions or age. The findings will inform policies, interventions, and strategies that address the diverse needs of homebound people living in the community [29, 30, 49].
2. Methods
This section builds upon the research protocol published in the JBI Evidence Synthesis [30] focusing specifically on the results of the systematic review and meta-analysis of telehealth’s effectiveness compared to standard in-person care regarding healthcare utilization, health-related quality of life (HRQOL), and well-being among homebound populations [30]. Adhering strictly to PRISMA guidelines, this revision enhances the original protocol’s methodological rigor to ensure thorough integration and comprehensive coverage of the methods utilized beyond the protocol. It outlines the specific modifications made during the research process to adapt to the evolving scope and requirements of the study [30].
2.1. Study Design and Participants
The systematic review included experimental and quasiexperimental studies such as randomized controlled trials (RCTs), nonrandomized controlled trials (NRCTs), before-and-after studies, and interrupted time series. Observational studies, grey literature, and qualitative investigations were excluded to prioritize high-quality, quantifiable data. Concerning participants, the systematic review included studies of homebound individuals facing severe mobility limitations due to chronic or acute health and psychosocial conditions. These individuals resided within community settings and required assistance for mobility or were entirely confined to their homes. Studies involving temporarily homebound individuals (less than 6 months) who had access to regular care and could manage without telehealth were excluded [30].
2.2. Interventions and Comparators
The interventions included telehealth services facilitated through digital platforms, telephone, wearable devices, and other telecommunication tools delivered by healthcare professionals and trained nonpractitioners [30]. The comparator was standard in-person care, excluding any services or data that incorporated mixed delivery methods [30].
2.3. Outcomes
Three primary outcomes were assessed: healthcare utilization, focusing on direct and indirect healthcare costs, and patient engagement and use measures [30]. HRQOL, using validated tools that measure impacts on health status [30]. And, well-being, which is evaluated through self-report instruments capturing its associated dimensions [30].
2.4. Search Strategy and Study Selection
Without language and time restrictions, a detailed search was conducted across multiple databases, including MEDLINE, Embase, PsycINFO, CINAHL, Scopus, LILACS, and the Web of Science. Full details of all database search strategies, translation methods, and summary results are provided in Appendix A (A1–A9), including database-specific strategies, results, and supplementary search approaches. Title and abstract screening followed by full-text reviews were performed by eleven independent reviewers, with discrepancies resolved through consensus or a third reviewer’s input [30]. The methods and inclusion criteria were registered in PROSPERO (CRD42021289578) and published elsewhere [30].
2.5. Methodological Quality Assessment, Data Extraction, and Synthesis
The quality of included studies was critically appraised using the JBI critical appraisal checklists for randomized and quasiexperimental studies as described elsewhere [30]. The critical appraisal results for RCTs are shown in Appendix B1 Table A6, and for quasiexperimental studies in Appendix B2 Table A7. Data were independently extracted using the JBI standardized data extraction tool [30] and managed in Excel. Adjustments and modifications from the protocol involved a detailed subgroup meta-analysis addressing the diversity of study designs and populations, focusing on different stages to capture the dynamic effects of telehealth irrespective of disease-specific limitations and other heterogeneity factors, as explained next.
2.6. Narrative Synthesis, Evidence Integration, Certainty of the Evidence
In addition to quantitative synthesis, a narrative approach was used to integrate and discuss the findings within the context of existing literature. This synthesis involved a collaborative effort among a team of 21 multidisciplinary researchers, consumers, and practitioners, who innovated by codesigning the study and providing a comprehensive review of the implications and gaps identified through the review of evidence [45, 50]. To that end, the GRADE approach was utilized by two reviewers to evaluate the certainty of the evidence, considering factors like methodological consistency, precision, and potential biases. The GRADE certainty assessment is summarized in Appendix C Table A8 [51]. To respond to methodological heterogeneity in study design, outcome tools, and reporting formats, we implemented a hybrid synthesis strategy. Meta-analysis was conducted only where outcome measures were conceptually aligned, tools were psychometrically validated, and statistical independence could be preserved by including only one measure per outcome, per study, and per time point. This approach ensured internal validity and minimized duplication within the pooled estimates. Studies that did not meet these criteria (due to incompatible formats, incomplete variance data, or atypical timelines) were analyzed narratively to capture their substantive contributions while maintaining methodological rigor.
2.7. Statistical Analysis
A random-effects subgroup meta-analysis was conducted using the restricted maximum likelihood (REML) method to account for within-study and between-study variabilities [52]. Separate analyses were conducted for each of the three primary outcomes—healthcare utilization, HRQOL, and well-being. These were modelled independently to avoid conflation of distinct constructs. Within each outcome, analyses were stratified by time point (baseline, first follow-up, and second follow-up) where data allowed. The effects were quantified using standardized mean differences (SMDs) [53] and presented through forest plots displaying the effect sizes and 95% confidence intervals for individual studies and the aggregated effect [54]. Heterogeneity among the studies was assessed using the I2 statistic, and publication bias was evaluated through Egger regression test [55] to detect any potential smaller studies with negative or nonsignificant results that could reflect publication bias [30]. All analyses were done via STATA SE 18.0.
3. Results
3.1. Study Inclusion/Search Result
The database searches yielded a total of 3289 articles across MEDLINE (402 records), PsychINFO (264 records), CINAHL (334 records), Embase (856 records), SCOPUS (700 records), Web of Science (375 records), LILACS (33 records), and CENTRAL (301 records). Following removing duplicates using Endnote and manual methods (MAPP, SB), 2001 articles were uploaded to JBI SUMARI for the initial screening of titles and abstracts by two sets of independent reviewers (M.A.P.d.P., R.A.-C., L.N.B., V.P., B.L., T.M., L.G., S.B., H.D., S.S., N.B., M.T.). After excluding irrelevant articles, two sets of independent reviewers (M.A.P.d.P., R.A.-C., L.N.B., V.P., B.L., T.M., L.G., S.B., H.D., S.S., N.B., M.T.) and two people solving disagreements (M.A.P.d.P., J.M.H.) screened 98 for full-text eligibility criteria. An additional set of 9 studies were manually identified as of 13/08/2023 (MAPP, RAC), but none met the eligibility criteria. Figure 1 provides detailed information on the selection process and inclusion and exclusion criteria.
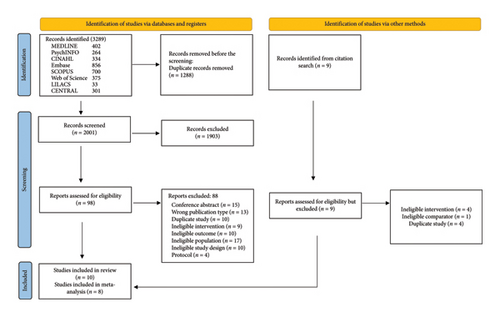
As Figure 1 indicates, 10 articles met the eligibility criteria, and 8 were ultimately included in the meta-analysis (by M.A.P.d.P., R.A.-C., A.G.). The included studies are as follows: Gellis et al. studied the impact of telehealth on homebound older adults with heart or chronic respiratory failure, finding reductions in depression, fewer emergency department visits, and improved quality of life, highlighting telehealth’s potential for integrated care delivery [47]. Gellis et al. explored telehealth’s role in managing chronic illness and comorbid depression in older adults, observing reductions in depression severity and healthcare utilization, further supporting its use in home health settings [56]. Choi et al. looked at telehealth as a treatment modality for depression in homebound older adults, noting significant reductions in depression and improved access to mental health services [57]. Similarly, Choi et al. examined the effectiveness of tele-delivered psychotherapy, finding it not only reduced depression but also improved disability levels, suggesting its potential for cost-effective mental health interventions [58]. Choi et al. investigated telehealth’s impact on social interaction and social isolation, finding positive outcomes for homebound older adults, underscoring its importance for addressing emotional and mental health needs [59].
Other included studies were Kahlon et al., which looked at an empathy-oriented telephone call program, finding reductions in loneliness, depression, and anxiety among isolated adults, which highlighted telehealth’s role in mitigating emotional distress [60]. Milosevic et al. studied videoconference interventions for anxiety and related disorders, providing preliminary evidence that they could be an effective alternative to face-to-face cognitive behavioral therapy [61]. Kobulnik et al. investigated nurse-assisted virtual visits for frail, older patients with heart failure, finding significant reductions in hospitalization rates, hospital days, and emergency department visits, suggesting telehealth’s practical benefits for those with barriers to specialized care [62]. While studies like Rees and Bashshur [63] and Zahoransky and Lape [64] explored the potential of telehealth in managing chronic conditions and home care, despite their contributions to the field, they were excluded from the meta-analysis due to specific methodological considerations.
3.2. Methodological Quality
The critical appraisal results for RCTs and quasiexperimental studies are provided in Appendix A. Some studies had specific limitations: In the RCTs, Choi et al. [58] had unclear randomization and no blinding. Kahlon et al. [60] had unclear allocation concealment and issues with treatment consistency, and Gellis et al. [47] did not blind participants. Kobulnik et al. [62], from the quasiexperimental studies, had unclear follow-up details. However, among the RCTs, Choi et al. [59] demonstrated excellent methodological rigor, achieving a perfect score of 100.0%. Kahlon et al. [60] and Gellis et al. [56] also exhibited high methodological quality, scoring 76.9% and 92.3%, respectively. Gellis et al. [47] attained a score of 76.9%, and Choi et al. [57] and Choi et al. [58] studies scored lower at 61.53% and 53.8%, respectively. In quasiexperimental studies, Milosevic et al. [61] and Zahoransky and Lape [64] demonstrated robust methodological quality, achieving 88.8%. Kobulnik et al. [62] and Rees and Bashshur [63] attained scores of 77.7%. These findings illustrate variations in methodological rigor across the included studies, but an overall quality assessment of ≈79.54% indicates a high methodological rigor level across both RCTs and quasiexperimental studies (refer to Appendix A).
3.3. Characteristics of Included Studies
Each study selected employed different time points, outcomes, measures, and timelines to assess the impact of telehealth interventions in homebound populations, as presented in Table 1. Gellis et al. [47] conducted a (RCT) study with baseline and first follow-up assessments over 3 months, involving 57 subjects in the intervention group (IG) and 58 in the control group (CG) in the United States. The study aimed to assess the impact of telehealth interventions on well-being, utilizing measures such as the Center for Epidemiologic Studies Depression (CES-D) Scale and the Patient Health Questionnaire (PHQ-9). Gellis et al. [56] (RCT) extended this investigation in the United States to assess the effects of integrated telehealth care on well-being among older adults with chronic illness and comorbid depression. Baseline, first follow-up, and second follow-up assessments were conducted over 3, 6, and 12 months, with 46 subjects in the IG and 48 in the CG. Outcome measures included depression severity measured by the PHQ-9 and Hamilton Depression Rating Scale (HAM-D), and HRQOL of life using the Medical Outcomes Study Short Form Health Survey (SF-36).
| Study | Time points | Outcomes | Measures | Timeline | Total subjects (baseline) | Total subjects (follow-up) | Results (intervention group) | Recommendation |
|---|---|---|---|---|---|---|---|---|
| Studies included in the meta-analysis (a) | ||||||||
| Gellis et al. [47] | Baseline; 1st follow-up | Well-being | Center for Epidemiologic Studies Depression (CES-D) Scale | Baseline, 3 months | 57 (IG); 58 (CG) | 57 (IG); 58 (CG) | Reduction in depression over time | Telehealth may be an efficient and effective method of systematically delivering integrated care in the home health sector |
| Patient Health Questionnaire (PHQ-9) | Increase in general health | |||||||
| Healthcare utilization | No. of ER visits | Fewer visits to the emergency department | ||||||
| Rehospitalization days | Fewer hospital days | |||||||
| No. of episodes of home care | Fewer episodes of home care | |||||||
| Health-related quality of life | Medical Outcomes Study Short Form Health Survey (SF-36) bodily pain | Lower level of perceived pain | ||||||
| Medical Outcomes Study Short Form Health Survey (SF-36) general health | Increase in general health | |||||||
| Medical Outcomes Study Short Form Health Survey (SF-36) social functioning | Increase in social functioning | |||||||
| Gellis et al. [56] | Baseline; 1st follow-up; 2nd follow-up | Well-being | Depression severity (PHQ-9) | Baseline, 3 months, 6 months | 46 (IG); 48 (CG) | 46 (IG); 48 (CG) | Decrease in depression severity | Integrated telehealth care for older adults with chronic illness and comorbid depression can reduce symptoms and postdischarge ED use in home health settings |
| Hamilton Depression Rating Scale (HAM-D) | Reduction in depression over time | |||||||
| Health-related quality of life | Medical Outcomes Study 12-item Short Form Survey (SF) mental component | Improvement in mental health component | ||||||
| Baseline; 1st follow-up | Healthcare utilization | Emergency department visits | Baseline, 12 months | Fewer visits to the emergency department | ||||
| Episodes of care | Fewer episodes of care | |||||||
| Hospital days | Fewer hospital days | |||||||
| Choi et al. [57] | Baseline; 1st follow-up; 2nd follow-up | Well-being | 24-item Hamilton Rating Scale for Depression (HAMD) | Baseline, 12 weeks, 24 weeks | 106 (IG); 106 (CG) | 106 (IG); 106 (CG) | Reduction in depression over time | Telehealth appears to be an efficacious treatment modality for depressed homebound older adults and to have significant potential to facilitate their access to treatment. |
| Choi et al. [58] | Baseline; 1st follow-up; 2nd follow-up; 3rd follow-up | Well-being | 24-item Hamilton Rating Scale for Depression (HAMD) | Baseline, 12 weeks, 24 weeks, 36 weeks | 56 (IG); 63 (CG) | 1st follow-up: 49 (IG), 54 (CG); 2nd follow-up: 41 (IG), 52 (CG); 3rd follow-up: 40 (IG), 45 (CG) | Reduction in depression over time | The efficacy and potential low cost of tele-delivered psychotherapy show its potential for easy replication and sustainability to reach a large number of underserved older adults and improve their access to mental health services |
| Disability score on the WHO Disability Assessment Schedule (WHODAS) | Improvement of disability level | |||||||
| Choi et al. [59] | Baseline; 1st follow-up; 2nd follow-up | Well-being | PROMIS Social Isolation Scale | Baseline, 6 weeks, 12 weeks | 43 (IG); 46 (CG) | 43 (IG); 46 (CG) | Positive impact on social interaction. | Telehealth is a promising intervention for the growing numbers of homebound older adults lacking social connectedness. |
| Depression severity (PHQ-9) | Decrease in depression severity | |||||||
| Disability (WHODAS 2.0) | Maintenance or improvement of the level of disability | |||||||
| Loneliness (PROMIS-L) | Reduction in social isolation over time | |||||||
| Kahlon et al. [60] | Baseline; 1st follow-up | Well-being | 3-Item UCLA Loneliness Scale | Baseline, 4 weeks | 120 (IG); 120 (CG) | 120 (IG); 120 (CG) | Improvement of perceived loneliness | An empathy-oriented telephone call program could reduce loneliness, depression, general mental health, and anxiety in isolated adults. |
| 6-Item De Jong Giervald Loneliness | Improvement of perceived loneliness | |||||||
| Generalized Anxiety Disorder Scale | Decrease in anxiety level | |||||||
| Personal Health Questionnaire for Depression (PHQ-9) | Decrease in depression severity | |||||||
| Lubben Social Network Scale (LSNS) | Similar levels of the perception of social support networks | |||||||
| Milosevic et al. [61] | Baseline; 1st follow-up | Well-being | Illness Intrusiveness Rating Scale (IIRS) | Baseline, 12 weeks | 50 (IG); 129 (CG) | 50 (IG); 129 (CG) | Similar levels of illness intrusiveness | Results provide preliminary evidence that videoconference intervention for anxiety and related disorders may be a promising and effective alternative to face-to-face cognitive behavioral therapy |
| Depression, Anxiety, and Stress Scales (DASS-21) | A slight reduction in anxiety levels | |||||||
| Kobulnik et al. [62] | Baseline; 1st follow-up | Healthcare utilization | Annualized hospitalization rate | Baseline, 1 year | 49 +(IG) | 49 (IG) | Statistically significant pre–post differences were obtained in the annualized hospitalization rate compared to the previous year. | Nurse-assisted virtual visits may be a preferable strategy for homebound, frail, and older patients with HF to receive longitudinal care. This approach may represent a plausible strategy to care for other patients with significant barriers to accessing specialized cardiac care. |
| Hospitalization days | Statistically significant pre–post differences were obtained in the hospitalization days compared to the previous year. | |||||||
| Emergency department visits | Statistically significant pre–post differences were obtained in the emergency department visits compared to the previous year. | |||||||
| Studies excluded in the meta-analysis (b) | ||||||||
| Rees and Bashshur [63] | Baseline; biweekly visits | Healthcare utilization | Emergency department visits | Baseline, 2 years | 21 (IG); 19 (CG) | 21 (IG); 19 (CG) | Fewer visits to the emergency department | The results of this clinical study strongly encourage that a single provider can affect positive clinical outcomes using a telemedicine wound care program. Tele-wound was a credible modality for managing pressure ulcers and improving health outcomes. |
| Inpatient hospitalization | Fewer inpatient hospitalizations | |||||||
| Length of stay | Shorter length of stay | |||||||
| Outpatient clinic contacts | Fewer outpatient clinic contacts, but differences are not statistically significant | |||||||
| Zahoransky et al. [64] | Baseline; 1st follow-up | Health-related quality of life | Canadian Occupational Performance Measure (COPM) | Baseline, 8 weeks | 9 participants (IG) | 9 participants (IG) | Statistically significant pre–post differences were obtained in the occupational performance | This study suggests that using telehealth for the traditional home care population and on-site and virtual visits may serve as a viable service delivery model for home care agencies and clients. |
| Outcome and Assessment Information Set (OASIS) | Statistically significant pre–post differences were obtained in the outcome and assessment information | |||||||
Choi et al. (RCT) [57] investigated in the United States the impact of telehealth interventions on the well-being of depressed homebound older adults. They conducted assessments at baseline, first follow-up, and second follow-up over 12 and 24 weeks, with 106 subjects in both the IG and CG. Outcome measures included depression severity measured by the 24-item Hamilton Rating Scale for Depression (HAMD). Choi et al. [58] (a) (RCT) assessed the efficacy of tele-delivered psychotherapy on the well-being of underserved older adults in the United States. Their study involved baseline, 12-, 24-, and 36-week assessments, with varying subject numbers across follow-up points. Outcome measures included depression severity measured by the 24-item Hamilton Rating Scale for Depression (HAMD) and disability scores using the WHO Disability Assessment Schedule (WHODAS).
Choi et al. (RCT) [59] examined in the United States the telehealth interventions’ impact on older adults’ well-being using baseline, first follow-up, and second follow-up assessments over 6 and 12 weeks, with 43 subjects in the IG and 46 in the CG. Outcome measures included the PROMIS Social Isolation Scale and depression severity measured by the PHQ-9. Kahlon et al. (RCT) [60] conducted a study in the United States to assess the impact of an empathy-oriented telephone call program on the well-being of isolated adults. Baseline and first follow-up assessments were performed over 4 weeks, with 120 subjects in both the IG and CG. Outcome measures included perceived loneliness measured by the three-item UCLA Loneliness Scale and anxiety levels assessed by the Generalized Anxiety Disorder Scale.
Milosevic et al. [61] (quasiexperimental) examined the impact of videoconference intervention on the well-being of individuals with anxiety and related disorders in Canada. Baseline and first follow-up assessments were conducted over 12 weeks, with 50 subjects in the IG and 129 in the CG. Outcome measures included the Illness Intrusiveness Rating Scale (IIRS) and the Depression, Anxiety, and Stress Scales (DASS-21). Kobulnik et al. [62] (quasiexperimental) assessed the impact of nurse-assisted virtual visits on healthcare utilization among older patients with heart failure in Canada. Baseline and first follow-up assessments were conducted over 1 year, with 49 subjects in the IG. Outcome measures included the annualized hospitalization rate and emergency department visits.
The excluded studies from the meta-analysis but included in the narrative review were Rees and Bashshur [63] (quasiexperimental), who conducted a study with baseline and biweekly follow-up assessments over two years, focusing on healthcare utilization among individuals with pressure ulcers in the United States. The IG comprised 21 subjects, while the CG had 19 subjects. Outcome measures included emergency department visits, inpatient hospitalization, length of stay, and outpatient clinic contacts. Zahoransky and Lape [64] (quasiexperimental) assessed HRQOL of life among participants receiving traditional home care with on-site and virtual visits in the United States. Baseline and first follow-up assessments were conducted over 8 weeks, involving 9 participants in the IG and the same in the control. Outcome measures included the Canadian Occupational Performance Measure (COPM) and the Outcome and Assessment Information Set (OASIS).
3.4. Review Findings
Findings regarding the three outcomes—healthcare utilization, HRQOL, and well-being—were analyzed and synthesized, considering different screening tools from different studies and conditions at varying points in time [30]. Pooling tools from various studies was feasible and necessary because the review prioritized assessing the overall effect of telehealth versus standard care on each primary outcome’s broad definition and a comprehensive homebound demographic [30]. Therefore, rather than examining specific diseases or events, we investigate their effectiveness, when possible, across three-time stages: baseline, first follow-up, and second follow-up, and assess the longitudinal/overall effects on each outcome as follows. To address potential outcome dependency, we included only one validated measurement tool per outcome per study at each time point. This ensured statistical independence and avoided duplication of data in pooled estimates. A random-effects approach that accounts for within-subject dependence or repeated measures in subgroup analyses was used rather than fixed effect approach. No study contributed more than one data point per outcome per time point in quantitative synthesis, ensuring statistical independence across all pooled effect estimates.
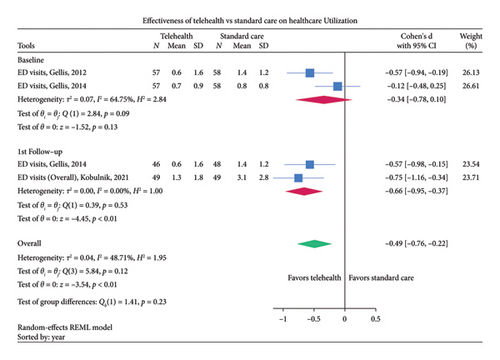
3.4.1. Healthcare Utilization
Examining healthcare utilization in Figure 2, the effect size showed a significant reduction in healthcare utilization for the IG [SMD = −0.66, 95% CI: −0.95, −0.37, p < 0.01] at first follow-up compared to usual care, with no difference in effects at baseline as expected from a RCT. The overall SMD score was −0.49 (SMD: −0.49 95% CI: −0.76, −0.22, p < 0.01, I2 = 48.71%, low certainty evidence) was less for the telehealth group compared to standard care, indicating a significant reduction in healthcare utilization. The moderate heterogeneity (I2 = 48.71%, Q (3) = 5.84, p < 0.12) indicates some variability in the effect-size estimates. The test of subgroup differences had shown no significant differences (p < 0.23). The Egger test found some small study effects or publication bias (z = −1.52, p < 0.13) that could be due to the exclusion of smaller studies with nonsignificant results that were not published and, therefore, not included in the meta-analysis.
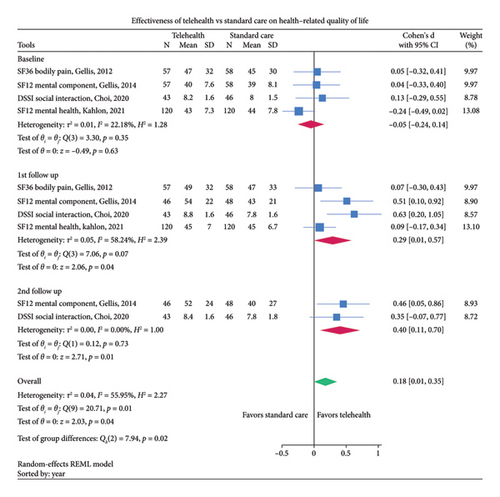
3.4.2. HRQOL
Concerning HRQOL, Figure 3 shows that telehealth interventions led to a significant improvement in HRQOL such as improvement in mental health or bodily pain than standard care [SMD: 0.29, 95%CI: 0.01, 0.57, p < 0.04] at first follow-up and even at second follow-up and overall [SMD: 0.18 95% CI: 0.01, 0.35, p < 0.04, I2 = 56%, moderate certainty evidence]. Higher the score reflects lower bodily pain or better the mental health, indicating improved HRQOL. The test of group-specific differences had shown significant differences (p < 0.02) in scores over time. Overall medium heterogeneity (I2 = 55.95%, p < 0.01) was observed; however, the Egger test reported some publication bias (z = 3.03, p < 0.002).
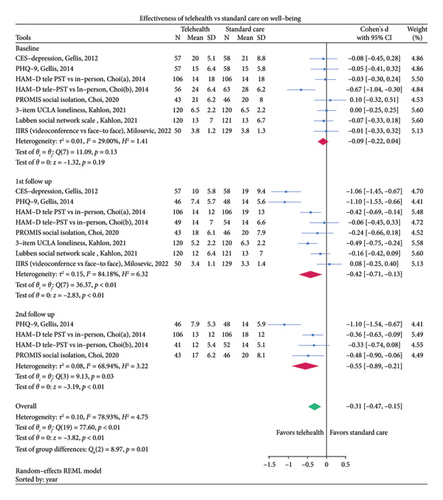
3.4.3. Well-Being
Figure 4 shows that telehealth interventions led to a significant reduction in well-being-related symptomatology (depression, loneliness, and isolation). A significant reduction in score of −0.42 [95% CI: −0.71, −0.13, p < 0.01] was observed at first follow-up, which was reduced further to −0.55 at the second follow-up, with overall reduction of −0.31 points (SMD = −0.31, 95% CI [−0.47, −0.15], p < 0.01, I2 = 79%, moderate certainty evidence). Despite tool heterogeneity, consistent directional effects support moderate certainty evidence favoring telehealth. The test for subgroup differences indicates a significant subgroup effect (p < 0.01). The overall high heterogeneity (I2 = 78.93%, p < 0.01) and no significant effect of small studies (z = −1.96, p < 0.05) were observed.
Due to reporting incompatibility concerning the REML methodology and the SMD calculations, two studies were excluded from the meta-analysis (see Table 1). Nonetheless, they are included in narrative form because of their significant results: Rees and Bashshur [63] conducted a 2-year study focusing on healthcare utilization among patients with pressure ulcers. Their findings revealed significant reductions in ED visits and inpatient hospitalizations, indicative of the effectiveness of telemedicine wound care programs. Similarly, Zahoransky and Lape [64] investigated HRQOL using the Canadian Occupational Performance Measure (COPM) and Outcome and Assessment Information Set (OASIS) over an 8-week period. Despite observing notable improvements in occupational performance, the study’s small sample size and reporting format limited its inclusion.
4. Discussion
Telehealth as a care solution for homebound patients has demonstrated significant benefits, including reduced healthcare utilization, improved HRQOL, and enhanced overall well-being. The decrease in healthcare utilization, with a SMD of −0.49, encompasses reductions in emergency department visits particularly among patients with heart failure, whether they have preserved or reduced ejection fractions. These findings suggest that telehealth can be a viable alternative to conventional healthcare delivery, potentially easing the strain on healthcare systems. However, further research is essential to maximize telehealth’s potential, particularly in refining the technical setup and ensuring effective service monitoring. It is crucial to address the need for targeted training for clinicians [65], caregivers, and patients to effectively utilize telehealth services [3, 66, 67]. Additionally, technical limitations such as data speed interruptions during consultations, suboptimal equipment quality for diagnostics and prognostics, and challenges with interoperability need to be considered and addressed [68].
Telehealth was found to show some positive improvement for HRQOL, including mental health, bodily pain, and social support (SMD: 0.18); this supports its integration into standard care practices and its potential applicability in areas like palliative care for people of all ages [44, 69, 70]. This aligns with studies showing telehealth’s benefits for conditions like chronic obstructive pulmonary disease (COPD), where it improved life quality and physical conditions [71]. This effect is also seen in homebound older adults with heart or chronic respiratory failure [72]. These findings highlight the need for new methods of continuous evaluation to fully understand telehealth and harness its capabilities to enhance patient outcomes over time and care stages [73]. However, publication bias calls for more detailed research to ascertain telehealth’s broader effects on this HRQOL outcome.
Our research also demonstrated the effectiveness of telehealth in enhancing well-being, showing a significant reduction in adverse outcomes related to depression, loneliness, social isolation, anxiety, stress, functionality, and disability while simultaneously improving the quality of personal relationships and the size and closeness of social networks (SMD: −0.31). These findings are reinforced by a related review, which concluded that telehealth modalities could effectively provide educational treatment augmentation and serve as a primary modality in mental health care, particularly after evaluating various factors such as mental well-being, cognitive flexibility, distress, sleep quality, self-efficacy, anger, decision-making conflicts, decision regret, digestive disturbances, pain, and medication adherence [74]. Moreover, including studies with methodological variations and a broad definition of homeboundness [30] has strengthened the evidence for telehealth’s positive impact across diverse homebound populations and primary outcomes. This approach also highlights the need for further research into telehealth’s efficacy, considering standardized evaluation methods across different contexts and characteristics. This need is supported by reviews and studies on loneliness and social connectivity among older adults [48, 63, 64].
The significant findings across the three primary outcomes validate the advantages and effectiveness of telehealth, as supported by similar studies focusing on older adults living in the community [23, 75, 76]. These results highlight that while benefits vary depending on disease characteristics and intervention designs [23, 75, 76], the overall positive impact of telehealth remains clear, even after adjusting for biases and outliers in our review. This consistency underscores telehealth’s role as a versatile and effective care modality. For homebound individuals, telehealth’s significance is further reinforced by literature demonstrating its ability to facilitate a strong therapeutic alliance between clinicians and patients [77], prove its efficacy across various medical disciplines [78], and earn high satisfaction ratings from users [79]. These advantages are echoed in studies presenting telehealth as an effective problem-solving solution for older adults dealing with cognitive impairments [80] and loneliness [81]. Furthermore, individuals suffering from conditions such as myalgic encephalomyelitis/chronic fatigue syndrome [14, 29, 82], heart and/or chronic respiratory failure, cancer, and rare diseases [34] have shown significant benefits from telehealth interventions. Thus, the current literature supports our findings, validating telehealth’s capacity to reduce the stress and costs [83] associated with traditional care modalities, making it a feasible solution for addressing many health challenges and impairments that affect vulnerable populations [72, 84, 85].
To effectively expand telehealth services, addressing the diverse needs of homebound individuals, their carers, and practitioners is crucial, especially in rural settings where challenges are more pronounced, as well as within urban populations as these groups are not identified by community or other care services [14, 29, 30]. Studies emphasize the importance of developing care models considering patients’ varying sociodemographics and impairments [79, 86, 87]. Specifically, they advocate for targeted, patient-centered telehealth interventions tailored to meet the specific needs of different homebound populations, particularly in countryside areas, where there is a strong demand for codesigned, culturally safe services that acknowledge these patients’ unique challenges—for instance, Mather et al. [38] conducted a latent class analysis to explore the heterogeneity among homebound older adults, underscoring the need to understand this population’s diverse needs.
Similarly, Scott Kruse et al. [79] systematically reviewed global barriers to telemedicine adoption, highlighting the critical need for tailored, patient-centered interventions to overcome these challenges. Onseng et al. [88] further emphasized the need for culturally safe and accessible telehealth services through a qualitative study that examined the expectations, attitudes, and barriers to telehomecare among caregivers of homebound or bedridden older adults. Moreover, several studies reinforce the importance of implementing collaborative, innovative codesign approaches in telehealth delivery. Turcotte et al. [89] conducted a rapid review to identify factors influencing older adults’ participation in telehealth interventions, stressing that codesign is vital in enhancing engagement. Ayabakan et al. [90] explored the impact of telehealth and process virtualization on healthcare utilization, noting that co-design plays a pivotal role in developing effective telehealth strategies. Choi and DiNitto [68] examined the digital divide among low-income, homebound older adults, focusing on their internet use patterns, eHealth literacy, and attitudes toward technology, highlighting the necessity for inclusive telehealth solutions tailored to various demographic and socioeconomic backgrounds.
4.1. Limitations
This systematic review involved ten studies with 2245 participants, assessing various outcomes, including follow-ups. The study designs were generally robust, featuring randomized trials and quasiexperimental studies. However, the review’s scope was constrained by strict selection criteria that excluded unpublished, observational, and qualitative studies and gray literature. This exclusion may have contributed to publication bias and limited the breadth of insights, particularly given the variability in interventions, outcomes, and participant demographics, resulting in a certainty of evidence that ranges from low to moderate. Additionally, the findings may not fully represent the diverse needs of specific subgroups or conditions, and their generalizability may apply primarily to the United States and Canada due to the origins of the data. Differences in healthcare systems, population sizes, and research priorities between global regions and other countries, such as Australia, underscore serious gaps in homebound care research. Despite these limitations, the review highlights the significant potential of telehealth as a valuable solution for improving care among homebound populations in developed countries. It calls for further research to strengthen the evidence base and enhance telehealth’s effectiveness across diverse settings, ultimately supporting its broader application in care delivery as suggested by similar studies [35, 44, 91].
4.2. Recommendation for Research
Future research on telehealth for homebound populations should prioritize codesigning interventions that address healthcare disparities, particularly in developed regions like Asia, Europe, and America [92, 93]. It is essential to evaluate, track, and scale telehealth services to ensure they are accessible, equitable, and tailored to consumer-centered demands [44, 45, 94–96]. Research should extend to underdeveloped countries, focusing on longitudinal and comparative studies to identify the most effective aspects of telehealth for different sociodemographics globally. Thus, trialing innovative care models integrating telehealth as comprehensive solutions is required, especially for underserved ethnic groups [94, 95, 97]. This integration requires addressing social determinants of health and intersectionality [98], as these factors influence the success of telehealth programs in areas such as cardiac health [46], peer support [96, 99], and care network integration [100, 101].
Researchers should further investigate telehealth’s broader implementation, particularly overcoming technological and personal barriers for populations that face challenges in participating in telehealth programs. Particular attention should be given to older adults, who often struggle with digital literacy and may prefer in-person interactions [102]. Additionally, the equity disparities in telehealth access across different ethnic and socioeconomic groups require targeted research to understand and mitigate these inequities [95, 103]. Including consumers in research through participatory approaches and examining the impact of policy changes, like telemedicine parity laws, on telehealth use, especially during public health crises such as the COVID-19 pandemic, is also necessary [100, 104], while considering the social and psychological impacts of long-term homebound status, particularly among younger individuals who may experience severe social withdrawal in conditions like Hikikomori [41, 101, 105]. Research should also focus on how telehealth can support home-based care for those with disabilities and residents in remote areas, given its potential to improve quality of life and reduce hospital visits [93, 98]. Expanding the scope of telehealth research [98, 106, 107] to include these homebound connected areas and social work perspectives will help develop comprehensive and inclusive research and practice frameworks that meet the complex needs of all homebound community segments across different life stages, care episodes, and people’s evolving needs [108–110].
4.3. Recommendation for Practice
Integrating telehealth into standard care is crucial for health practitioners to enhance healthcare access and equity, particularly in managing chronic conditions and providing mental health support. Research has highlighted the importance of addressing the digital divide that affects access to primary care, especially in the post-COVID era [100, 104, 111]. Tailored telehealth services are essential for meeting the diverse needs of different populations [105, 112, 113], including neurodiverse patients and those experiencing extreme social withdrawal; accordingly, overcoming barriers to telehealth access for older adults and vulnerable groups [17, 114] is vital to ensure these services are inclusive and widely accessible [105, 112, 113]. Practitioners must focus on developing telehealth adaptable models of care that are responsive to individual patient needs in various situations. This includes equipping all stakeholders [115–117]—caregivers, clinicians, and healthcare providers—with the necessary knowledge and tools to use telehealth effectively and reduce cognitive load during telehealth visits [113]. To that end, culturally sensitive care models [95, 103] that address the specific challenges faced by different patient populations [102] are essential [101, 118–120]. Adopting advanced technologies, including AI [121], machine learning, sensor-based monitoring [122], and other methods [123–125], can further enhance the effectiveness of telehealth. These tools can help monitor functional capacity, manage medication interactions, and strengthen social and care networks, thereby supporting the well-being of homebound individuals and those at risk of becoming homebound [109, 126–129]. By adopting these strategies, practitioners can ensure that telehealth not only meets the immediate needs of patients but also supports their long-term health within their communities and life course [68, 109, 128].
4.4. Recommendation for Policymakers
Policymakers are urged to develop policies that promote telehealth as a standard care modality [15, 16, 23, 130], invest in necessary infrastructure, and set standards for telehealth quality, privacy, and security [14, 33, 131]; this will save resources by reducing emergency department presentations and hospitalizations [114]. Encouraging the involvement of transdisciplinary teams in codesigning and testing telehealth services [100, 132, 133] is essential, especially in countries like Australia, South Korea, and other countries [134], where homebound consumers call for telehealth access beyond fiscal attendance [29, 30, 32, 33]. It is vital for creating sustainable and effective healthcare solutions [95, 106, 107]. Challenges such as legislative barriers, reimbursement issues [23, 130, 135], and the need for a skilled workforce and care navigators highlight the necessity for an evidence-based strategic approach to telehealth policy and implementation [17, 101, 105, 114] to ensure no one is left behind in accessing quality health care and addressing intersectionality when creating the required telehealth new models of care [101, 105, 136].
5. Conclusion
This study underscores the effectiveness of telehealth in meeting the complex needs of homebound individuals, with transdisciplinary analyses advocating for its broader integration into healthcare practices. Our findings reveal that telehealth significantly reduces healthcare utilization, including emergency department visits, episodes of care, hospitalization days, and hospitalization rates. Notably, these reductions extend to cardiovascular-related hospitalizations, offering distinct benefits for patients with heart failure, whether with preserved or reduced ejection fraction. Additionally, telehealth enhances HRQOL by improving mental and physical health, reducing bodily pain, and increasing general health, social functioning, and social interaction. Moreover, telehealth positively impacts overall well-being by reducing depression, loneliness, social isolation, anxiety, stress, and disability while also strengthening personal relationships and expanding the size and closeness of social networks for homebound populations.
These results establish telehealth as a viable alternative to in-person care, particularly for mental health conditions and primary care services, with significant benefits for rural and underserved populations. While telehealth is confirmed as a comprehensive solution regardless of the cause of homeboundness, the codesign of telehealth programs tailored to the specific needs of underserved communities and individuals with chronic diseases is crucial for enhancing healthcare delivery to marginalized populations. Future research should focus on including more diverse study designs and populations, utilizing standardized measures to explore telehealth’s potential and limitations fully. Policymakers, researchers, and practitioners are encouraged to apply these findings in developing telehealth strategies that are accessible, equitable, and codesigned to address the diverse needs of homebound populations, ensuring quality healthcare services and resource savings through reduced reliance on traditional care models and more emphasis in fundamental care across the life course.
Disclosure
The funders had no role in study design, data collection and analysis, decision to publish, or preparation of the manuscript.
Conflicts of Interest
The authors declare no conflicts of interest.
Author Contributions
M.A.P.d.P. led the study design, coordinated the research team, conducted the analysis (with A.G. running the meta-analysis), extracted titles and abstracts, assessed the quality of the studies, extracted data, and drafted the whole manuscript. M.A.P.d.P. oversaw and cocreated all aspects of the project. S.B. created with M.A.P.d.P. searches and translation. A.G. supported data analysis with governance in the meta-analysis and contributed significantly to the manuscript writing. A.G. and L.N.B. with M.A.P.d.P. did the GRADE assessment. R.A.-C. was responsible for full and final data extraction with the support of M.A.P.d.P. and A.G. V.P., B.L., T.M., L.G., S.B., H.D., S.S., L.N.B., R.A.-C., and N.B. contributed to quality assessment, title, abstract screening, and initial data extraction. A.B., K.N., M.T., S.C., and S.H. assisted with the transdisciplinary data analysis (with the rest of the coauthors) and provided recommendations on drafting and revising the manuscript. A.K., S.H., R.C., and J.M.H. were senior authors, with R.C. and J.M.H. serving as clinical leaders. They played a significant role in guiding the research directions and critically revising the manuscript for important intellectual content. P.M. served as a consumer coresearcher, providing unique insights from a community perspective, and participated in the design, analysis, and manuscript revisions. All authors contributed to writing the final document and approved its submission. All authors agree to be accountable for all aspects of the work, ensuring that questions related to the accuracy or integrity of any part are appropriately investigated and resolved.
Funding
This study was supported by the Flinders University Caring Futures Institute (Cardiac Focus Area Research Grant 2021). Salary support for the leading author was provided by the Caring Futures Institute, Flinders University.
Acknowledgments
The authors would like to thank Flinders University Caring Futures Institute, Better Care (College of Nursing and Health Sciences), and leaders: Alison Kitson, and Clinical leaders: Robyn Clark, and Jeroen M. Hendriks for funding and supporting a Systematic Literature Review Group and its training.
Appendix
This section presents Appendix A: Search Strategies and Translation Methods [30], Appendix B1: Critical Appraisal Results (RCTs), Appendix B2: Critical Appraisal Results (Quasiexperimental Studies), and Appendix C: GRADE Certainty Assessment Table.
Appendix A: Search Strategies and Translation Methods
Details of all database search strategies, results, and translation methods are provided in Appendix A. This includes a summary table (A1), database-specific search strategies, and results (A2–A5), and notable supplementary search strategies for Scopus, Web of Science, Cochrane CENTRAL, and LILACS (A6–A9).
Appendix A1: Summary of Databases and Search Dates
A summary of all bibliographic databases searched, the number of records retrieved, search dates, and deduplication steps is provided in Table A1.
| Database | Result | Date |
|---|---|---|
| MEDLINE | 402 | 26/06/2022 |
| PsychINFO | 264 | 26/06/2022 |
| CINAHL | 334 | 26/06/2022 |
| Embase | 856 | 26/11/2021 |
| Scopus | 700 | 29/11/2021 |
| Web of Science | 375 | 29/11/2021 |
| LILACS | 33 | 29/11/2021 |
| Central | 301 | 29/11/2021 |
| Total | 3289 | 26/06/2022 |
| Duplicates | 1288 | 30/07/2022 |
| Updated manual citation search but excluded | −9 | 13/08/2023 |
| Net total | 2001 | 13/08/2023 |
Appendix A2: Ovid MEDLINE(R) Search Strategy
The full Ovid MEDLINE(R) search strategy and corresponding results are detailed in Table A2.
| Ovid MEDLINE(R) and Epub ahead of print, in-process, in-data-review & other non-indexed citations, daily and versions < 1946 to June 20, 2022 > | ||
|---|---|---|
| 1 | Homebound persons/or agoraphobia/or bedridden persons/ | 3417 |
| 2 | (Homebound or “home-bound” or housebound or “house-bound” or bedbound or “bed-bound” or bedfast or bedridden or “bed-ridden” or “shut in∗” or “shut-in∗” or Hikikomori or agoraphobi∗).tw,kw. | 8833 |
| 3 | or/1-2 | 9821 |
| 4 | exp Telemedicine/ | 40,821 |
| 5 | (telehealth∗ or “tele-health∗” or telemedicine∗ or “tele-medicine∗” or telecare∗ or “tele-care∗” or telematic∗ or telepharmacy or “tele-pharmacy” or telenurs∗ or “tele-nurs∗” or “tele-homecare” or telehomecare or teleconsultation or “tele-consultation∗”).tw,kf. | 30,458 |
| 6 | ((remote∗ or distant or distance) adj2 (consult∗ or monitor∗ or care or treat∗ or therap∗)).tw,kf. | 10,348 |
| 7 | ((mobile∗ or digital∗) adj2 health∗).tw,kf. | 13,626 |
| 8 | (ehealth or “e-health” or mhealth or “m-health”).tw,kf. | 12,508 |
| 9 | exp Technology/ | 476,377 |
| 10 | exp Telephone/ | 33,459 |
| 11 | exp Videoconferencing/ | 2642 |
| 12 | exp Electronic mail/ | 2895 |
| 13 | exp Text messaging/ | 4141 |
| 14 | exp software/ | 177,011 |
| 15 | exp Computers, handheld/ | 11,736 |
| 16 | Computer-assisted instruction/ | 12,408 |
| 17 | exp decision making, computer-assisted/ | 131,109 |
| 18 | Wireless technology/ | 4334 |
| 19 | exp internet/ | 92,888 |
| 20 | (Internet∗ or computer∗ or web∗ or online∗ or telephone or phone∗ or sms or mms or texting or text messag∗ or video∗ or skype∗ or zoom).tw,kf. | 964,978 |
| 21 | (email or “e-mail” or electronic mail or interactive∗ or telecommunication∗ or wireless∗ or bluetooth∗ or telecommunication∗ or smartphone∗ or cellphone∗ or iphone∗ or ipod∗ or podcast∗ or ipad∗ or android∗ or blackberr∗ or “palm pilot∗” or pda∗ or personal digital assistant∗).tw,kf. | 150,676 |
| 22 | ((tablet∗ or “hand-held∗”) adj3 (device or computer)).tw,kf. | 2545 |
| 23 | (social∗ adj2 (media∗ or network∗)).tw,kf. | 48,424 |
| 24 | (“smart?watch” or wearable∗).tw,kf. | 21,412 |
| 25 | or/4–24 | 1,797,231 |
| 26 | 3 and 25 | 856 |
| 27 | Clinical study/or exp clinical trial/or controlled clinical trial/or exp randomized controlled trial/or observational study/or comparative study/or multicenter study/ | 2,805,789 |
| 28 | Control groups/or cross-over studies/or double-blind method/or matched-pair analysis/or random allocation/or single-blind method/or control groups/or matched-pair analysis/or prospective studies/or retrospective studies/ | 2,694,167 |
| 29 | Clinical studies as topic/or clinical trials as topic/or case–control studies/or retrospective studies/or cohort studies/or follow-up studies/or prospective studies/or controlled before–after studies/or cross-sectional studies/or interrupted time series analysis/or multicenter studies as topic/ | 3,051,054 |
| 30 | (“clinical trial” or “clinical trial, phase i” or “clinical trial, phase ii” or clinical trial, phase iii or clinical trial, phase iv or controlled clinical trial or “multicenter study” or “randomized controlled trial”).pt. | 1,131,616 |
| 31 | (randomised or randomized or randomly or random or placebo or mask∗ or blind∗ or trial or placebo or quantitative or cohort or “4 arm” or “four arm” or baseline or consecutive∗ or “case series” or RCT).tw. | 3,875,406 |
| 32 | ((Quasi-experimental or clinical or cluster∗ or “before and after” or “before-and-after” or crossover or “cross-over” or “cross over” or retrospective or cohort or follow-up or “follow-up” or prospective) adj5 (trial∗ or studies or study)).tw. | 1,904,947 |
| 33 | (time∗ adj2 interrupted).tw. | 4843 |
| 34 | (control∗ adj4 (Cohort∗ or group∗)).tw. | 673,558 |
| 35 | or/27–34 | 8,011,429 |
| 36 | 26 and 35 | 452 |
| 37 | exp animals/not humans.sh. | 5,019,716 |
| 38 | (address or autobiography or bibliography or biography or case reports or clinical trial veterinary or comment or congress or consensus development conference or consensus development conference nih or directory or editorial or festschrift or guideline or interview or legal case or letter or meta analysis or news or newspaper article or observational study or observational study veterinary or patient education handout or personal narrative or portrait or practice guideline or randomized controlled trial veterinary or “review” or “systematic review” or technical report or video audio media or webcast).pt. | 7,804,418 |
| 39 | or/37–38 | 12,523,616 |
| 40 | 36 not 39 | 402 |
Appendix A2.1: MEDLINE Guide
-
/ = Subject Heading or MeSH heading
-
∗ = Truncation symbol, will find all variations of the words’ ending—eg therap∗ will find therapist, therapists, therapy, therapies
-
ti,ab. = searching for these words only in the title or abstract of the paper
-
kf. = searching for these words in the author supplied keywords
-
adj3 = Adjacency—words need to be within 3 (can be a different number) words of each other
-
pt. = Publication type
-
or/x-y = Boolean search of OR—used to combine all variations of words within one concept, will make the results bigger
-
and/x,y,z = Boolean search of AND—will tie the concepts together and make the results smaller
Appendix A3: PsycINFO Search Strategy
-
To open the results:
-
Go to Flinders Library
-
Click on Databases
-
Search for PsycINFO—click on Available Online—click PsycINFO (via Ovid)
-
Click on View saved (top right of page). Use name and Password.
-
Click in the little box next to QoL Homebound PsycINFO 24_11_2021
-
Then click the Run button above
-
The full PsycINFO search strategy and results are presented in Table A3.
| APA PsycInfo < 1806 to June week 3 2022 > | ||
|---|---|---|
| 1 | Homebound/or agoraphobia/ | 3473 |
| 2 | (Homebound or “home-bound” or housebound or “house-bound” or Bedbound or “bed-bound” or Bedfast or Bedridden or “bed-ridden” or “shut in∗” or “shut-in∗” or Hikikomori or agoraphobi∗).tw,id. | 6718 |
| 3 | or/1–2 | 7061 |
| 4 | exp telemedicine/ | 11,279 |
| 5 | (telehealth∗ or “tele-health∗” or telemedicine∗ or “tele-medicine∗” or telecare∗ or “tele-care∗” or telematic∗ or telepharmacy or “tele-pharmacy” or telenurs∗ or “tele-nurs∗” or “tele-homecare” or telehomecare or teleconsultation or “tele-consultation∗”).tw,id. | 5703 |
| 6 | ((remote∗ or distant or distance) adj2 (consult∗ or monitor∗ or care or treat∗ or therap∗)).tw,id. | 1221 |
| 7 | exp Telephone systems/ | 9061 |
| 8 | exp computer mediated communication/ | 19,639 |
| 9 | exp computer applications/ | 82,468 |
| 10 | Internet/ | 30,441 |
| 11 | (Internet∗ or computer∗ or web∗ or online∗ or telephone or phone∗ or sms or mms or texting or text messag∗ or video∗ or skype∗ or zoom).tw,id. | 380,975 |
| 12 | (email or “e-mail” or electronic mail or interactive∗ or telecommunication∗ or wireless∗ or bluetooth∗ or telecommunication∗ or smartphone∗ or cellphone∗ or iphone∗ or ipod∗ or podcast∗ or ipad∗ or android∗ or blackberr∗ or “palm pilot∗” or pda∗ or personal digital assistant∗).tw,id. | 61,381 |
| 13 | ((tablet∗ or “hand-held∗”) adj3 (device or computer)).tw,id. | 785 |
| 14 | (social∗ adj2 (media∗ or network∗)).tw,id. | 53,802 |
| 15 | (“smart?watch” or wearable∗).tw,id. | 1999 |
| 16 | or/4–15 | 491,425 |
| 17 | exp clinical trial/or controlled clinical trial/or exp randomized controlled trial/or comparative study/or multicenter study/ | 13,268 |
| 18 | Case–control studies/or Control groups/or matched-Pair analysis/or cohort studies/or follow-up studies/or prospective studies/or retrospective studies/or cross-over studies/or double-blind method/or single-blind method/ | 2862 |
| 19 | clinical studies as topic/or clinical trials as topic/or case–control studies/or retrospective studies/or cohort studies/or follow-up studies/or prospective studies/or controlled before–after studies/or cross-sectional studies/or interrupted time series analysis/or multicenter studies as topic/ | 1919 |
| 20 | (“clinical trial” or “clinical trial, phase i” or “clinical trial, phase ii” or clinical trial, phase iii or clinical trial, phase iv or controlled clinical trial or “multicenter study” or “randomized controlled trial” or trial).pt. | 0 |
| 21 | (randomised or randomized or randomly or random or placebo or mask∗ or blind or trial or placebo or quantitative or cohort or “4 arm” or “four arm” or baseline or consecutive∗ or “case series” or RCT).tw. | 634,622 |
| 22 | ((Quasi-experimental or clinical or cluster∗ or “before and after” or “before-and-after” or crossover or “cross-over” or “cross over” or retrospective or cohort or follow-up or “follow-up” or prospective) adj5 (trial∗ or studies or study)).tw. | 190,926 |
| 23 | (time∗ adj2 interrupted).tw. | 1057 |
| 24 | (control∗ adj5 (Cohort∗ or group∗)).tw. | 122,279 |
| 25 | or/17–24 | 796,463 |
| 26 | 3 and 16 and 25 | 264 |
Appendix A3.1: PsycINFO Guide
-
/ = Subject Heading or MeSH heading
-
∗ = Truncation symbol, will find all variations of the words’ ending—eg therap∗ will find therapist, therapists, therapy, therapies
-
ti,ab. = searching for these words only in the title or abstract of the paper
-
id = searching for these words in the author-supplied keywords
-
lo = geographic location
-
adj3 = Adjacency—words need to be within 3 (can be a different number) words of each other
-
pt. = Publication type
-
or/x-y = Boolean search of OR—used to combine all variations of words within one concept, will make the results bigger
Appendix A4: Embase Search Strategy
-
cross-sectional study/or exp controlled study/or exp controlled clinical trial/or
-
clinical study/or exp case control study/or exp clinical trial/or intervention study/or prospective study/or retrospective study/
-
Saved as homebound quant 26_06_2022
-
The Embase database search strategy and outcomes are summarized in Table A4.
| Embase < 1974 to 2022 June 24 > | ||
|---|---|---|
| 1 | Homebound patient/or agoraphobia/ | 7302 |
| 2 | (Homebound or “home-bound” or housebound or “house-bound” or Bedbound or “bed-bound” or Bedfast or Bedridden or “bed-ridden” or “shut in∗” or “shut-in∗” or Hikikomori or agoraphobi∗).tw,kw. | 12,616 |
| 3 | or/1–2 | 15,517 |
| 4 | exp telemedicine/ | 60,650 |
| 5 | (telehealth∗ or “tele-health∗” or telemedicine∗ or “tele-medicine∗” or telecare∗ or “tele-care∗” or telematic∗ or telepharmacy or “tele-pharmacy” or telenurs∗ or “tele-nurs∗” or “tele-homecare” or telehomecare or teleconsultation or “tele-consultation∗”).tw,kf. | 39,916 |
| 6 | ((remote∗ or distant or distance) adj2 (consult∗ or monitor∗ or care or treat∗ or therap∗)).tw,kf. | 15,468 |
| 7 | ((mobile∗ or digital∗) adj2 health∗).tw,kf. | 13,999 |
| 8 | (ehealth or “e-health” or mhealth or “m-health”).tw,kf. | 12,072 |
| 9 | exp technology/ | 250,883 |
| 10 | e-mail/or exp internet/or exp mobile phone/or telephone/or text messaging/or videoconferencing/or web conferencing/ | 227,337 |
| 11 | exp software/ | 272,370 |
| 12 | exp personal computer/or personal digital assistant/ | 12,773 |
| 13 | Wireless communication/ | 6677 |
| 14 | (Internet∗ or computer∗ or web∗ or online∗ or telephone or phone∗ or sms or mms or texting or text messag∗ or video∗ or skype∗ or zoom).tw,kf. | 1,267,363 |
| 15 | (email or “e-mail” or electronic mail or interactive∗ or telecommunication∗ or wireless∗ or bluetooth∗ or telecommunication∗ or smartphone∗ or cellphone∗ or iphone∗ or ipod∗ or podcast∗ or ipad∗ or android∗ or blackberr∗ or “palm pilot∗” or pda∗ or personal digital assistant∗).tw,kf. | 205,749 |
| 16 | ((tablet∗ or “hand-held∗”) adj3 (device or computer)).tw,kf. | 3787 |
| 17 | (social∗ adj2 (media∗ or network∗)).tw,kf. | 58,308 |
| 18 | (“smart?watch” or wearable∗).tw,kf. | 23,595 |
| 19 | or/4–18 | 2,002,343 |
| 20 | cross-sectional study/or exp controlled study/or exp controlled clinical trial/or clinical study/or exp case control study/or exp clinical trial/or intervention study/or prospective study/or retrospective study/ | 11,102,154 |
| 21 | clinical trial (topic)/or “adaptive clinical trial (topic)”/or exp “controlled clinical trial (topic)”/or “multicenter study (topic)”/or “phase 1 clinical trial (topic)”/or “phase 2 clinical trial (topic)”/or “phase 3 clinical trial (topic)”/or “phase 4 clinical trial (topic)”/ | 394,484 |
| 22 | (randomised or randomized or randomly or random or placebo or mask∗ or blind∗ or trial or placebo or quantitative or cohort or “4 arm” or “four arm” or baseline or consecutive∗ or “case series” or RCT).tw. | 5,611,807 |
| 23 | ((Quasi-experimental or clinical or cluster∗ or “before and after” or “before-and-after” or crossover or “cross-over” or “cross over” or retrospective or cohort or follow-up or “follow-up” or prospective) adj5 (trial∗ or studies or study)).tw. | 2,784,983 |
| 24 | (time∗ adj2 interrupted).tw. | 6061 |
| 25 | (control∗ adj4 (Cohort∗ or group∗)).tw. | 966,339 |
| 26 | or/20–25 | 14,360,300 |
| 27 | 3 and 19 and 26 | 866 |
| 28 | (exp animal/or exp invertebrate/or nonhuman/or animal experiment/or animal tissue/or animal model/or exp plant/or exp fungus/) not (exp human/or human tissue/) | 7,391,148 |
| 29 | (Chapter or editorial or letter).pt. | 2,008,456 |
| 30 | or/28–29 | 9,309,381 |
| 31 | 27 not 30 | 858 |
Appendix A5: CINAHL Search Strategy
-
Database log-in details:
-
To open the results:
-
Go to Flinders Library
-
Click on Databases
-
Search for CINAHL—click on Available Online—click CINAHL
-
Click on View saved (top right of page)
-
Enter username and Password.
-
Click in the little box next to: Telehealth homebound QOL
-
Then click the Run button above
-
The CINAHL database search steps and number of results retrieved are provided in Table A5.
| # | Query | Results |
|---|---|---|
| S30 | S3 AND S21 AND S29 | 356 |
| S29 | S22 OR S23 OR S24 OR S25 OR S26 OR S27 OR S28 | 1,835,384 |
| S28 | TI ((control∗ N5 (Cohort∗ OR group∗))) OR AB ((control∗ N5 (Cohort∗ OR group∗))) | 167,047 |
| S27 | (TI (time∗ N2 interrupted) OR AB (time∗ N2 interrupted)) OR (TI (time∗ N2 interrupted) OR AB (time∗ N2 interrupted)) | 2469 |
| S26 | TI (((“quasi-experimental∗” OR clinical or cluster∗ OR “before and after” OR “before-and-after” OR crossover OR “cross-over” OR “cross over” OR retrospective OR cohort∗ OR “follow-up” OR “follow-up” OR prospective) N5 (trial∗ OR studies OR study))) OR AB (((“quasi-experimental∗” OR clinical or cluster∗ OR “before and after” OR “before-and-after” OR crossover OR “cross-over” OR “cross over” OR retrospective OR cohort∗ OR “follow-up” OR “follow-up” OR prospective) N5 (trial∗ OR studies OR study))) | 588,486 |
| S25 | TI ((random∗ OR placebo OR mask∗ OR blind OR trial OR placebo OR quantitative OR cohort OR “4 arm” OR “four arm” OR baseline OR consecutive∗ OR “case series” OR RCT)) OR AB ((random∗ OR placebo OR mask∗ OR blind OR trial OR placebo OR quantitative OR cohort OR “4 arm” OR “four arm” OR baseline OR consecutive∗ OR “case series” OR RCT)) | 1,119,613 |
| S24 | (MH “Case Control Studies”) OR (MH “Cross Sectional Studies”) OR (MH “Double-Blind Studies”) OR (MH “Prospective Studies”) OR (MH “Concurrent Prospective Studies”) OR (MH “Nonconcurrent Prospective Studies”) OR (MH “Single-Blind Studies”) OR (MH “Triple-Blind Studies”) OR (MH “Matched-Pair Analysis”) | 827,658 |
| S23 | (MH “Case Control Studies+”) OR (MH “Cross Sectional Studies”) OR (MH “Double-Blind Studies”) OR (MM “Prospective Studies”) OR (MH “Single-Blind Studies”) OR (MH “Triple-Blind Studies”) | 386,911 |
| S22 | (MH “Clinical Trials”) OR (MH “Double-Blind Studies”) OR (MH “Randomized Controlled Trials+”) OR (MH “Single-Blind Studies”) OR (MH “Triple-Blind Studies”) OR (MH “Intervention Trials”) | 337,701 |
| S21 | S4 OR S5 OR S6 OR S7 OR S8 OR S9 OR S10 OR S11 OR S12 OR S13 OR S14 OR S15 OR S16 OR S17 OR S18 OR S19 OR S20 | 976,087 |
| S20 | TI ((“smart#watch∗” OR wearable∗)) OR AB ((“smart#watch∗” OR wearable∗)) | 4202 |
| S19 | TI ((social∗ N1 (media∗ OR network∗))) OR AB ((social∗ N1 (media∗ OR network∗))) | 30,083 |
| S18 | TI (((tablet∗ OR “hand-held∗”) N2 (device OR computer))) OR AB (((tablet∗ OR “hand-held∗”) N2 (device OR computer))) | 1609 |
| S17 | TI ((email OR “e-mail” OR electronic mail OR interactive∗ OR telecommunication∗ OR wireless∗ OR bluetooth∗ OR telecommunication∗ OR smartphone∗ OR cellphone∗ OR iphone∗ OR ipod∗ OR podcast∗ OR ipad∗ OR android∗ OR blackberr∗ OR “palm pilot∗” OR pda∗ OR “personal digital assistant∗”)) OR AB ((email OR “e-mail” OR electronic mail OR interactive∗ OR telecommunication∗ OR wireless∗ OR bluetooth∗ OR telecommunication∗ OR smartphone∗ OR cellphone∗ OR iphone∗ OR ipod∗ OR podcast∗ OR ipad∗ OR android∗ OR blackberr∗ OR “palm pilot∗” OR pda∗ OR “personal digital assistant∗”)) | 58,303 |
| S16 | TI ((internet∗ OR computer∗ OR web∗ OR online∗ OR telephone OR phone∗ OR sms OR mms OR texting OR “text messag∗” OR video∗ OR skype∗ OR zoom)) OR AB ((internet∗ OR computer∗ OR web∗ OR online∗ OR telephone OR phone∗ OR sms OR mms OR texting OR “text messag∗” OR video∗ OR skype∗ OR zoom)) | 346,853 |
| S15 | (MH “decision Making, Computer Assisted+”) | 48,733 |
| S14 | (MH “Computer Assisted instruction”) | 8214 |
| S13 | (MH “Computers, Hand-Held+”) | 8240 |
| S12 | (MH “Software+”) | 433,437 |
| S11 | (MH “Telecommunications+”) | 157,248 |
| S10 | (MH “Technology+”) | 83,652 |
| S9 | TI ((ehealth OR “e-health” OR mhealth OR “m-health”)) OR AB ((ehealth OR “e-health” OR mhealth OR “m-health”)) | 6650 |
| S8 | TI (((mobile∗ OR digital∗) N1 health∗)) OR AB (((mobile∗ OR digital∗) N1 health∗)) | 5395 |
| S7 | TI (((remote∗ OR distant OR distance) N1 (consult∗ OR monitor∗ OR care OR treat∗ OR therap∗))) OR AB (((remote∗ OR distant OR distance) N1 (consult∗ OR monitor∗ OR care OR treat∗ OR therap∗))) | 3617 |
| S6 | TI (((remote∗ OR distant OR distance) N1 (consult∗ OR monitor∗ OR care OR treat∗ OR therap∗))) OR AB (((remote∗ OR distant OR distance) N1 (consult∗ OR monitor∗ OR care OR treat∗ OR therap∗))) | 3617 |
| S5 | TI ((telehealth∗ OR “tele-health∗” OR telemedicine∗ OR “tele-medicine∗” OR telecare∗ OR “tele-care∗” OR telematic∗ OR telepharmacy OR “tele-pharmacy” OR telenurs∗ OR “tele-nurs∗” OR “tele-homecare” OR telehomecare OR teleconsultation OR “tele-consultation∗”)) OR AB ((telehealth∗ OR “tele-health∗” OR telemedicine∗ OR “tele-medicine∗” OR telecare∗ OR “tele-care∗” OR telematic∗ OR telepharmacy OR “tele-pharmacy” OR telenurs∗ OR “tele-nurs∗” OR “tele-homecare” OR telehomecare OR teleconsultation OR “tele-consultation∗”)) | 15,029 |
| S4 | (MH “Telehealth+”) | 32,233 |
| S3 | S1 OR S2 | 3334 |
| S2 | TI ((Homebound OR “home-bound” OR housebound OR “house-bound” OR Bedbound OR “bed-bound” OR Bedfast OR Bedridden OR “bed-ridden” OR “shut in∗” OR “shut-in∗” OR Hikikomori OR agoraphobi∗)) OR AB ((Homebound OR “home-bound” OR housebound OR “house-bound” OR Bedbound OR “bed-bound” OR Bedfast OR Bedridden OR “bed-ridden” OR “shut in∗” OR “shut-in∗” OR Hikikomori OR agoraphobi∗)) | Display |
| S1 | (MH “Homebound Persons”) OR (MH “Bedridden Persons”) OR (MH “agoraphobia”) | 1289 |
Appendix A5.1: CINAHL Guide
-
/ = Subject Heading
-
∗ = Truncation symbol, will find all variations of the words’ ending—eg therap∗ will find therapist, therapists, therapy, therapies
-
““= Add double quotes around phrases (two words or more)
-
TI = = searching for these words only in the title
-
AB = = searching for these words only in the abstract
-
N3 = Adjacency—words need to be within 3 (can be a different number) words of each other
-
OR = Boolean search of OR—used to combine all variations of words within one concept, will make the results bigger
-
AND = Boolean search of AND—will tie the concepts together and make the results smaller
Appendix A6: Notable Search Strategy—Scopus
-
Go to Flinders Library
-
Click on Databases
-
Search for Scopus—click on Available Online—click Scopus
-
Click on Advanced Search
-
Enter in the below search string
-
TITLE-ABS-KEY ((homebound OR “home-bound” OR housebound OR “house-bound” OR bedbound OR “bed-bound” OR bedfast OR bedridden OR “bed-ridden” OR “shut in∗” OR “shut-in∗” OR hikikomori OR agoraphobi∗) AND (telehealth∗ OR “tele-health∗” OR telemedicine∗ OR “tele-medicine∗” OR telecare∗ OR “tele-care∗” OR telematic∗ OR telepharmacy OR “tele-pharmacy” OR telenurs∗ OR “tele-nurs∗” OR “tele-homecare” OR telehomecare OR teleconsultation OR “tele-consultation∗” OR ((remote∗ OR distant OR distance) W/2 (consult∗ OR monitor∗ OR care OR treat∗ OR therap∗)) OR ((remote∗ OR distant OR distance) W/2 (consult∗ OR monitor∗ OR care OR treat∗ OR therap∗)) OR ((mobile∗ OR digital∗) W/2 health∗) OR ehealth OR “e-health” OR mhealth OR “m-health” OR internet∗ OR computer∗ OR web∗ OR online∗ OR telephone OR phone∗ OR sms OR mms OR texting OR “text messag∗” OR video∗ OR skype∗ OR zoom OR email OR “e-mail” OR “electronic mail” OR interactive∗ OR telecommunication∗ OR wireless∗ OR bluetooth∗ OR telecommunication∗ OR smartphone∗ OR cellphone∗ OR iphone∗ OR ipod∗ OR podcast∗ OR ipad∗ OR android∗ OR blackberr∗ OR “palm pilot∗” OR pda∗ OR “personal digital assistant∗” OR ((tablet∗ OR “hand-held∗”) W/3 (device OR computer)) OR (social∗ W/2 (media∗ OR network∗)) OR smartwatch∗ OR “smart watch∗” OR “smart-watch∗” OR wearable∗) AND ((control∗ W/5 (cohort∗ OR group∗)) OR (time∗ W/2 interrupted) OR ((“quasi-experimental∗” OR clinical OR cluster∗ OR “before and after” OR “before-and-after” OR crossover OR “cross-over” OR “cross over” OR retrospective OR cohort∗ OR “follow-up” OR “follow-up” OR prospective) W/5 (trial∗ OR studies OR study)) OR random∗ OR placebo OR mask∗ OR blind OR trial OR placebo OR quantitative OR cohort OR “4 arm” OR “four arm” OR baseline OR consecutive∗ OR “case series” OR rct)) AND (LIMIT-TO (DOCTYPE, “ar”))
-
(homebound OR “home-bound” OR housebound OR “house-bound” OR bedbound OR “bed-bound” OR bedfast OR bedridden OR “bed-ridden” OR “shut in∗” OR “shut-in∗” OR hikikomori OR agoraphobi∗)
-
AND
-
(telehealth∗ OR “tele-health∗” OR telemedicine∗ OR “tele-medicine∗” OR telecare∗ OR “tele-care∗” OR telematic∗ OR telepharmacy OR “tele-pharmacy” OR telenurs∗ OR “tele-nurs∗” OR “tele-homecare” OR telehomecare OR teleconsultation OR “tele-consultation∗” OR ((remote∗ OR distant OR distance) W/2 (consult∗ OR monitor∗ OR care OR treat∗ OR therap∗)) OR ((remote∗ OR distant OR distance) W/2 (consult∗ OR monitor∗ OR care OR treat∗ OR therap∗)) OR ((mobile∗ OR digital∗) W/2 health∗) OR ehealth OR “e-health” OR mhealth OR “m-health” OR internet∗ OR computer∗ OR web∗ OR online∗ OR telephone OR phone∗ OR sms OR mms OR texting OR “text messag∗” OR video∗ OR skype∗ OR zoom OR email OR “e-mail” OR “electronic mail” OR interactive∗ OR telecommunication∗ OR wireless∗ OR bluetooth∗ OR telecommunication∗ OR smartphone∗ OR cellphone∗ OR iphone∗ OR ipod∗ OR podcast∗ OR ipad∗ OR android∗ OR blackberr∗ OR “palm pilot∗” OR pda∗ OR “personal digital assistant∗” OR ((tablet∗ OR “hand-held∗”) W/3 (device OR computer)) OR (social∗ W/2 (media∗ OR network∗)) OR smartwatch∗ OR “smart watch∗” OR “smart-watch∗” OR wearable∗)
-
((control∗ W/5 (Cohort∗ OR group∗)) OR (time∗ W/2 interrupted) OR ((“quasi-experimental∗” OR clinical or cluster∗ OR “before and after” OR “before-and-after” OR crossover OR “cross-over” OR “cross over” OR retrospective OR cohort∗ OR “follow-up” OR “follow-up” OR prospective) W/5 (trial∗ OR studies OR study)) OR random∗ OR placebo OR mask∗ OR blind OR trial OR placebo OR quantitative OR cohort OR “4 arm” OR “four arm” OR baseline OR consecutive∗ OR “case series” OR RCT)
-
TITLE-ABS-KEY (((homebound OR “home-bound” OR housebound OR “house-bound” OR bedbound OR “bed-bound” OR bedfast OR bedridden OR “bed-ridden” OR “shut in∗” OR “shut-in∗” OR hikikomori OR agoraphobi∗) AND ((telehealth∗ OR “tele-health∗” OR telemedicine∗ OR “tele-medicine∗” OR telecare∗ OR “tele-care∗” OR telematic∗ OR telepharmacy OR “tele-pharmacy” OR telenurs∗ OR “tele-nurs∗” OR “tele-homecare” OR telehomecare OR teleconsultation OR “tele-consultation∗”) OR ((remote∗ OR distant OR distance) W/2 (consult∗ OR monitor∗ OR care OR treat∗ OR therap∗)) OR ((remote∗ OR distant OR distance) W/2 (consult∗ OR monitor∗ OR care OR treat∗ OR therap∗)) OR ((mobile∗ OR digital∗) W/2 health∗) OR (ehealth OR “e-health” OR mhealth OR “m-health”) OR (internet∗ OR computer∗ OR web∗ OR online∗ OR telephone OR phone∗ OR sms OR mms OR texting OR “text messag∗” OR video∗ OR skype∗ OR zoom) OR (email OR “e-mail” OR “electronic mail” OR interactive∗ OR telecommunication∗ OR wireless∗ OR bluetooth∗ OR telecommunication∗ OR smartphone∗ OR cellphone∗ OR iphone∗ OR ipod∗ OR podcast∗ OR ipad∗ OR android∗ OR blackberr∗ OR “palm pilot∗” OR pda∗ OR “personal digital assistant∗”) OR ((tablet∗ OR “hand-held∗”) W/3 (device OR computer)) OR (social∗ W/2 (media∗ OR network∗)) OR (smartwatch∗ OR “smart watch∗” OR “smart-watch∗” OR wearable∗)))
-
AND
Appendix A7: Notable Search Strategy—Web of Science
-
Go to Flinders Library
-
Click on Databases
-
Search for Web of Science—click on Available Online—click Web of Science
-
Click on Advanced Search
-
Enter in the below search string
-
TS=(((homebound OR “home-bound” OR housebound OR “house-bound” OR bedbound OR “bed-bound” OR bedfast OR bedridden OR “bed-ridden” OR “shut in∗” OR “shut-in∗” OR hikikomori OR agoraphobi∗) AND (telehealth∗ OR “tele-health∗” OR telemedicine∗ OR “tele-medicine∗” OR telecare∗ OR “tele-care∗” OR telematic∗ OR telepharmacy OR “tele-pharmacy” OR telenurs∗ OR “tele-nurs∗” OR “tele-homecare” OR telehomecare OR teleconsultation OR “tele-consultation∗” OR ((remote∗ OR distant OR distance) NEAR/2 (consult∗ OR monitor∗ OR care OR treat∗ OR therap∗)) OR ((remote∗ OR distant OR distance) NEAR/2 (consult∗ OR monitor∗ OR care OR treat∗ OR therap∗)) OR ((mobile∗ OR digital∗) NEAR/2 health∗) OR ehealth OR “e-health” OR mhealth OR “m-health” OR internet∗ OR computer∗ OR web∗ OR online∗ OR telephone OR phone∗ OR sms OR mms OR texting OR “text messag∗” OR video∗ OR skype∗ OR zoom OR email OR “e-mail” OR “electronic mail” OR interactive∗ OR telecommunication∗ OR wireless∗ OR bluetooth∗ OR telecommunication∗ OR smartphone∗ OR cellphone∗ OR iphone∗ OR ipod∗ OR podcast∗ OR ipad∗ OR android∗ OR blackberr∗ OR “palm pilot∗” OR pda∗ OR “personal digital assistant∗” OR ((tablet∗ OR “hand-held∗”) NEAR/3 (device OR computer)) OR (social∗ NEAR/2 (media∗ OR network∗)) OR smartwatch∗ OR “smart watch∗” OR “smart-watch∗” OR wearable∗) AND ((control∗ NEAR/5 (cohort∗ OR group∗)) OR (time∗ NEAR/2 interrupted) OR ((“quasi-experimental∗” OR clinical OR cluster∗ OR “before and after” OR “before-and-after” OR crossover OR “cross-over” OR “cross over” OR retrospective OR cohort∗ OR “follow-up” OR “follow-up” OR prospective) NEAR/5 (trial∗ OR studies OR study)) OR random∗ OR placebo OR mask∗ OR blind OR trial OR placebo OR quantitative OR “4 arm” OR “four arm” OR baseline OR cohort OR consecutive∗ OR “case series” OR rct)))
Appendix A8: Notable Search Strategy—Cochrane Central
-
Go to Cochrane https://www.cochranelibrary.com/
-
Go to advanced search
-
Go to Search manager and enter each of the lines below separately (see screen shot below)
-
#1 ((homebound OR “home-bound” OR housebound OR “house-bound” OR bedbound OR “bed-bound” OR bedfast OR bedridden OR “bed-ridden” OR “shut in∗” OR “shut-in∗” OR hikikomori OR agoraphobi∗)):ti,ab,kw
-
#2 (((telehealth∗ OR “tele-health∗” OR telemedicine∗ OR “tele-medicine∗” OR telecare∗ OR “tele-care∗” OR telematic∗ OR telepharmacy OR “tele-pharmacy” OR telenurs∗ OR “tele-nurs∗” OR “tele-homecare” OR telehomecare OR teleconsultation OR “tele-consultation∗”) OR ((remote∗ OR distant OR distance) NEAR/2 (consult∗ OR monitor∗ OR care OR treat∗ OR therap∗)) OR ((remote∗ OR distant OR distance) NEAR/2 (consult∗ OR monitor∗ OR care OR treat∗ OR therap∗)) OR ((mobile∗ OR digital∗) NEAR/2 health∗) OR (ehealth OR “e-health” OR mhealth OR “m-health”) OR (internet∗ OR computer∗ OR web∗ OR online∗ OR telephone OR phone∗ OR sms OR mms OR texting OR “text messag∗” OR video∗ OR skype∗ OR zoom) OR (email OR “e-mail” OR “electronic mail” OR interactive∗ OR telecommunication∗ OR wireless∗ OR bluetooth∗ OR telecommunication∗ OR smartphone∗ OR cellphone∗ OR iphone∗ OR ipod∗ OR podcast∗ OR ipad∗ OR android∗ OR blackberr∗ OR “palm pilot∗” OR pda∗ OR “personal digital assistant∗”) OR ((tablet∗ OR “hand-held∗”) NEAR/3 (device OR computer)) OR (social∗ NEAR/2 (media∗ OR network∗)) OR (smartwatch∗ OR “smart watch∗” OR “smart-watch∗” OR wearable∗))):ti,ab,kw
-
((control∗ NEAR/5 (cohort∗ OR group∗)) OR (time∗ NEAR/2 interrupted) OR ((“quasi-experimental∗” OR clinical OR cluster∗ OR “before and after” OR “before-and-after” OR crossover OR “cross-over” OR “cross over” OR retrospective OR cohort∗ OR “follow-up” OR “follow-up” OR prospective) NEAR/5 (trial∗ OR studies OR study)) OR random∗ OR placebo OR mask∗ OR blind OR trial OR placebo OR quantitative OR cohort OR “4 arm” OR “four arm” OR baseline OR consecutive∗ OR “case series” OR rct):ti,ab,kw
-
#1 AND #2 AND #3
-
Total 303
Appendix A9: Notable Search Strategy—LILACS
- 1.
Go to Lilacs https://lilacs.bvsalud.org/en/
- 2.
Go in the search bar enter
-
(((homebound OR “home-bound” OR housebound OR “house-bound” OR bedbound OR “bed-bound” OR bedfast OR bedridden OR “bed-ridden” OR “shut in∗” OR “shut-in∗” OR hikikomori OR agoraphobi∗)) AND (((telehealth∗ OR “tele-health∗” OR telemedicine∗ OR “tele-medicine∗” OR telecare∗ OR “tele-care∗” OR telematic∗ OR telepharmacy OR “tele-pharmacy” OR telenurs∗ OR “tele-nurs∗” OR “tele-homecare” OR telehomecare OR teleconsultation OR “tele-consultation∗”) OR ((remote∗ OR distant OR distance) AND(consult∗ OR monitor∗ OR care OR treat∗ OR therap∗)) OR ((remote∗ OR distant OR distance) AND (consult∗ OR monitor∗ OR care OR treat∗ OR therap∗)) OR ((mobile∗ OR digital∗) AND health∗) OR (ehealth OR “e-health” OR mhealth OR “m-health”) OR (internet∗ OR computer∗ OR web∗ OR online∗ OR telephone OR phone∗ OR sms OR mms OR texting OR “text messag∗” OR video∗ OR skype∗ OR zoom) OR (email OR “e-mail” OR “electronic mail” OR interactive∗ OR telecommunication∗ OR wireless∗ OR bluetooth∗ OR telecommunication∗ OR smartphone∗ OR cellphone∗ OR iphone∗ OR ipod∗ OR podcast∗ OR ipad∗ OR android∗ OR blackberr∗ OR “palm pilot∗” OR pda∗ OR “personal digital assistant∗”) OR ((tablet∗ OR “hand-held∗”) AND (device OR computer)) OR (social∗ AND (media∗ OR network∗)) OR (smartwatch∗ OR “smart watch∗” OR “smart-watch∗” OR wearable∗))) AND ((control∗ AND (cohort∗ OR group∗)) OR (time∗ AND interrupted) OR ((“quasi-experimental∗” OR clinical OR cluster∗ OR “before and after” OR “before-and-after” OR crossover OR “cross-over” OR “cross over” OR retrospective OR cohort∗ OR “follow-up” OR “follow-up” OR prospective) AND (trial∗ OR studies OR study)) OR random∗ OR placebo OR mask∗ OR blind OR trial OR placebo OR quantitative OR cohort OR “4 arm” OR “four arm” OR baseline OR consecutive∗ OR “case series” OR rct))
Appendix B: Critical Appraisal Results
The critical appraisal results for RCTs are shown in Appendix B1, Table A6, and for quasi-experimental studies in Appendix B2, Table A7.
| Citation | Q1 | Q2 | Q3 | Q4 | Q5 | Q6 | Q7 | Q8 | Q9 | Q10 | Q11 | Q12 | Q13 | % |
|---|---|---|---|---|---|---|---|---|---|---|---|---|---|---|
| Choi et al. [59] | Y | Y | Y | Y | Y | Y | Y | Y | Y | Y | Y | Y | Y | 100.0 |
| Kahlon et al. [60] | Y | Y | Y | U | U | Y | U | Y | Y | Y | Y | Y | Y | 76.9 |
| Gellis et al. [56] | Y | Y | Y | Y | Y | Y | U | Y | Y | Y | Y | Y | Y | 92.3 |
| Choi et al. [57] | U | U | Y | N | N | N | U | Y | Y | Y | Y | Y | U | 61.53 |
| Gellis et al. [47] | Y | Y | Y | N | Y | Y | Y | Y | Y | N | Y | Y | N | 76.9 |
| Choi et al. [58](a) | Y | N | Y | N | N | Y | N | Y | N | Y | Y | N | N | 53.8 |
- Note: Y = Yes, N = no, U = Unclear.
| Citation | Q1 | Q2 | Q3 | Q4 | Q5 | Q6 | Q7 | Q8 | Q9 | % |
|---|---|---|---|---|---|---|---|---|---|---|
| Kobulnik et al. [62] | Y | Y | Y | U | N | Y | Y | Y | Y | 77.7 |
| Milosevic et al. [61] | Y | Y | N | Y | Y | Y | Y | Y | Y | 88.8 |
| Zahoransky et al. [64] | Y | Y | Y | N | Y | Y | Y | Y | Y | 88.8 |
| Rees and Bashshur [63] | Y | Y | Y | Y | Y | U | U | Y | Y | 77.7 |
- Note: Y = Yes, N = no, U = Unclear.
Appendix B1: Critical Appraisal Results (RCTs)
-
Q1. Was true randomization used for assignment of participants to treatment groups?
-
Q2. Was allocation to treatment groups concealed?
-
Q3. Were treatment groups similar at the baseline?
-
Q4. Were participants blind to treatment assignment?
-
Q5. Were those delivering treatment blind to treatment assignment?
-
Q6. Were outcomes assessors blind to treatment assignment?
-
Q7. Were treatments groups treated identically other than the intervention of interest?
-
Q8. Was follow-up complete and if not, were differences between groups in terms of their follow-up adequately described and analyzed?
-
Q9. Were participants analyzed in the groups to which they were randomized?
-
Q10. Were outcomes measured in the same way for treatment groups?
-
Q11. Were outcomes measured in a reliable way?
-
Q12. Was appropriate statistical analysis used?
-
Q13. Was the trial design appropriate, and any deviations from the standard RCT design (individual randomization, parallel groups) accounted for in the conduct and analysis of the trial
Appendix B2: Critical Appraisal Results (Quasiexperimental Studies)
-
Q1. Is it clear in the study what is the “cause” and what is the “effect” (i.e., is there no confusion about which variable comes first)?
-
Q2. Were the participants included in any comparisons similar?
-
Q3. Were the participants included in any comparisons receiving similar treatment/care, other than the exposure or intervention of interest?
-
Q4. Was there a control group?
-
Q5. Were there multiple measurements of the outcome both pre and post the intervention/exposure?
-
Q6. Was follow-up complete and if not, were differences between groups in terms of their follow-up adequately described and analyzed?
-
Q7. Were the outcomes of participants included in any comparisons measured in the same way?
-
Q8. Were outcomes measured in a reliable way?
-
Q9. Was appropriate statistical analysis used?
Appendix C: Certainty of the Evidence (GRADE)
-
Question: Telehealth compared to usual care for homebound populations
-
Population: Homebound people
-
Intervention: Telehealth
-
Setting: Community
-
Comparison: Standard Care
-
Outcomes: Healthcare Utilization, Health-related Quality of Life, and Well-being
| Certainty assessment | No of patients | Effect | Certainty | Importance | ||||||||
|---|---|---|---|---|---|---|---|---|---|---|---|---|
| No. of studies | Study design | Risk of bias | Inconsistency | Indirectness | Imprecision | Other considerations | Telehealth | Usual care | Relative (95% CI) | Absolute (95% CI) | ||
| Healthcare utilization | ||||||||||||
| 3 | Randomized trials | Not serious | Not serious | Serious | Not serious | Publication bias strongly suspected | 346 | 346 | — | SMD: −0.49 (lower score); 95% CI: −0.76 to −0.22 |
|
|
| Health-related quality of life | ||||||||||||
| 4 | Randomized trials | Not serious | Not serious | Not serious | Not serious | Publication bias suspected | 218 | 218 | — | SMD: 0.18 (higher score); 95% CI: 0.01 to 0.35 |
|
|
| Wellbeing | ||||||||||||
| 7 | Randomized trials | Not serious | Serious | Not serious | Not serious | Undetected | 540 | 577 | — | SMD -0.31 (lower score) 95% CI: (−0.47, −0.15) |
|
|
- Abbreviations: CI = confidence interval, SMD = standardized mean difference.
- aDowngraded 1 level due to publication bias.
- bDowngraded 2 level due to publication bias and indirectness.
- cDowngraded 1 level due inconsistency.
Open Research
Data Availability Statement
The data that support the findings of this study are available within the article. Further data may be available from the corresponding author upon reasonable request.




