Improving Adherence to Appointments in Postradiotherapy Surveillance Practice Through Telephone Reminders Among Breast and Prostate Cancer Patients
Abstract
Objectives: This study aimed to identify factors that influence appointment adherence in postradiotherapy surveillance (PRS) and to evaluate the impact of a telephone reminder system on improving patient adherence among breast and prostate cancer patients.
Methods: A retrospective cross-sectional study was conducted to analyze data from patients scheduled for PRS within a period of 6 months. A total of 468 consecutive patients who were treated with breast or prostate irradiation were divided into two groups: those who attended their appointments and those who did not. Telephone reminders were used as interventions for nonattendees, with a first reminder (I1) followed by a second reminder (I2) in case of nonresponse. Data analysis included univariate and multivariable models to assess factors that affect adherence.
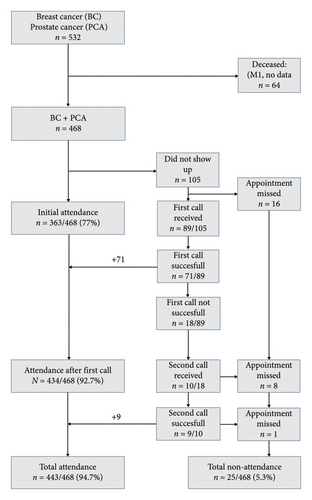
Results: Out of 468 patients, 363 patients (77.6%) initially attended their scheduled appointments. The first telephone reminder increased adherence to 92.7% (434/468 patients). A second reminder further increased the attendance rate to 94.7% (443/468 patients). Marital status was a significant factor, with single individuals having more than three times the odds of nonattendance compared to married individuals. A trend toward significance was found for cigarette smoking as a possible further factor for nonattendance. No significant difference was found between the two groups in any of the other patient-, tumor- or treatment-related characteristics.
Conclusions: Telephone reminders significantly increase appointment adherence in PRS practice, with the first reminder showing the most substantial effect. Single patients have a particularly high risk of nonparticipation, highlighting the need for targeted interventions.
Advances in Knowledge: This study demonstrates the effectiveness of telephone reminders as a cost-effective strategy to improve adherence in PRS surveillance practice, particularly among the high-risk groups, such as single patients.
1. Introduction
Postradiotherapy surveillance (PRS), also known as “postradiotherapy follow-up,” is an integral part of radiotherapeutic treatment for patients with oncological diseases and is legally mandated in Germany [1]. It serves to document long-term side effects and treatment response, making it essential for quality assurance in radiation oncology. The acute side effects of radiotherapy subside within 3 months (3 M) after the completion of radiotherapy. Conversely, late side effects of radiotherapy occur only after a relatively long latency period and usually have a low incidence rate. Severe late effects of radiation are rare but require further diagnostic examinations and, if necessary, therapeutic interventions.
Therefore, PRS examinations are typically conducted at regular intervals over a period of 5 years after the completion of radiotherapy [2]. Assessments of PRS include a medical history discussion and a symptom-focused clinical examination to detect any potential radiotherapy-related side effects, such as skin reactions after breast irradiation or lower urinary tract symptoms (LUTSs) after prostate irradiation, and are carried out by physicians at most institutions in Germany. This process involves relevant personnel and organizational effort.
Recently, Holtgrave et al. reported that appointment adherence in PRS decreased continuously over a 5-year period in breast cancer patients. This not only affects the quality of radiotherapeutic treatment but is also a risk factor for cancer patients to develop unmet needs, such as a lack of information, supportive care, and physical or psychological assistance. Optimal appointment adherence in PRS is also essential for the implementation of risk-adapted radiotherapeutic treatment schedules and possibly reduced surveillance practices in radiation oncology [3].
We conducted a retrospective cross-sectional study to improve PRS practices by enhancing appointment adherence. The aim of this study was to identify factors that influence appointment adherence and to investigate the impact of telephone reminders on improving adherence to PRS practices among breast and prostate cancer patients.
2. Materials and Methods
2.1. Organization of Follow-Ups
At our clinic, PRS occurs within a period of 5 years after radiation therapy has been completed. To this end, patients are summoned to our clinic at specified time intervals for a follow-up appointment. The first appointment takes place 3 M after the completion of radiation, followed by further appointments at 12 months (12 M), 36 months (36 M) and 60 months (60 M). If a patient appears at the appointment as initially agreed, the anamnesis, clinical examination and documentation of the findings are carried out to record all late effects of radiotherapy and the response to treatment. Then, a new appointment is arranged according to the abovementioned scheme. Further diagnostics and possible treatments will be initiated if higher-grade adverse events occur, as defined by valid scores, as well as in cases of suspected recurrence of the tumor. If necessary, closer monitoring is subsequently carried out.
If patients do not attend the appointment as initially agreed upon, an intervention is made in the form of an initial telephone contact (I1). This intervention takes the form of personal telephone calls by a trained healthcare professional and is carried out as a one-time contact attempt. If the patient is reachable, a replacement appointment is arranged at short intervals of approximately 2 weeks.
If patients do not attend this appointment, a second and final telephone contact (I2) will be made with the aim of arranging a replacement appointment. If personal contact is not feasible, no voicemail will be left. Instead, a letter is sent to the referring oncologist, stating that the patient did not attend the scheduled follow-up appointment and requesting the oncologist to re-refer the patient, particularly if treatment-related side effects occur. The study period for this retrospective cross-sectional analysis covered six consecutive months of our postradiotherapy follow-up consultation. To identify the possible factors that influence appointment adherence, a group comparison was made between patients who initially attended the appointment and patients who did not initially attend the agreed-upon appointment. These two groups were compared for significant differences in patient-, tumor- and treatment-related characteristics.
In addition, we investigated the effect of telephone reminders on the time between the end of radiotherapy and the examination date. To this end, the interval between the end of radiotherapy and the examination date was recorded for each patient. Subgroups were formed according to the respective year in which the follow-up examination occurred. For each subgroup, the increase in appointment adherence after the telephone reminder (I1) was calculated. All patients who had undergone radiotherapy provided consent for an anonymous evaluation of their data for research purposes. The investigation was approved by the Local Ethics Committee of the Hannover Medical School.
2.2. Study Population
First, all consecutive patients who had an appointment for a radiotherapy follow-up at our clinic during the study period were recorded. The analysis was carried out via the patient data management system MOSAIQ by Elekta. All patients who had undergone curative radiotherapy were included regardless of their diagnosis. Breast cancer, including ductal carcinoma in situ (DCIS), and prostate cancer typically affect the majority of patients treated with radiotherapy. In addition, 532/988 (54%) of these two entities comprised the majority of all patients treated with radiotherapy during the study period at our clinic. Since both groups are homogenous in terms of sex due to the oncological entity, only these two groups were examined in more detail for further analysis. Notably, the study population did not include male patients with breast cancer. Other diagnostic groups were poorly represented in terms of numbers and therefore could not be evaluated in a statistically meaningful manner. To avoid inclusion bias, we also excluded patients with metastatic tumors or active tumor disease during treatment, as well as trial participants (due to different follow-up schedules), patients with insufficient language skills, and support-dependent patients. Data on demographic, social, illness, and therapy-related factors were collected from the available patient files to investigate their possible influence on adherence to appointments. The TNM stage was classified based on the 7th edition of the standardized tumor/node/metastasis classification of the Union for International Cancer Control (UICC) [4]. If available, the pathological TNM stage was used; otherwise, the clinical TNM stage was documented.
2.3. Radiation Data
Breast cancer is predominantly treated with conventional techniques (three-dimensional conformal technique [3D-CRT]). Among the 259 patients, 165 (63.5%) received conventional fractionated irradiation with single doses ranging from 1.8 Gray (Gy) to 2.0 Gy. Mild hypofractionated irradiation with a single dose of 2.1 Gy was administered to 22 patients (8.5%). 58 patients (22.5%) received moderately hypofractionated radiation with a single dose of 2.67 Gy. Intraoperative radiation with a single dose of 20 Gy was administered to 14 patients (5.5%). The cumulative median dose was 50 Gy (20–60 Gy) for this cohort. Prostate cancer was predominantly treated with modern intensity modulation technology with image guidance. In the prostate cancer group, conventional fractionation with single doses ranging from 1.8 to 2.0 Gy was used almost exclusively in 208 of the 209 (99.5%) patients. One patient received hypofractionated radiation with a single dose of 3.0 Gy. The collective cumulative median dose was 66.6 Gy (45–78 Gy).
2.4. Assessments
Exclusively physicians carried out the assessment and investigation during the postradiotherapy follow-up. Information on patient, tumor, and treatment characteristics was collected from medical records and reports. Postradiotherapy follow-up data included follow-up events (recurrence, metastases, second tumor, death, and late radiation effects) as well as attendance at appointments and were collected from medical records and, in part, from appointment books. Higher-grade acute and chronic side effects (Grades 3–5) were recorded in this analysis. To document early/acute radiotherapy–related side effects, version four of the classification of the National Cancer Center’s Common Terminology Criteria of Adverse Events (CTCAE) was used [5]. Chronic radiogenic adverse events (or late radiation effects) are defined as reactions that occur at the earliest 3 M after the end of radiotherapy. Grading was carried out in accordance with the LENT–SOMA criteria [6].
The presence of relevant secondary diagnoses/comorbidities and their possible influence on the follow-up behavior of the patients were also examined. Relevant secondary diagnoses were defined as comorbidities that are usually associated with long-term therapy or regular medical visits or that require long-term therapeutic support. These patients were divided into appropriate groups (neurological, cardiovascular, rheumatological, psychiatric, nephrological, pulmonary, and previous oncological diseases). Common mild comorbidities, such as arterial hypertension, hypothyroidism, and osteoarthritis, were considered irrelevant. If several comorbidities from different groups were present, they were documented as “multiple” in a separate group (Table 1).
| Category | n (%) |
|---|---|
| Cardiovascular diseases (coronary heart disease, heart failure, pacemaker, postmyocardial infarction, and bypass) | 64 (13.7) |
| Neoplasms/secondary malignancies | 27 (5.8) |
| Metabolic diseases (insulin-dependent diabetes mellitus) | 8 (1.7) |
| Nephrological diseases (chronic renal insufficiency and kidney transplantation) | 2 (0.4) |
| Neurological diseases (dementia and postapoplexy) | 7 (1.5) |
| Psychiatric diseases (depression and schizophrenia) | 10 (2.1) |
| Respiratory diseases (COPD and bronchial asthma) | 2 (0.4) |
| Other diseases (chromosomal aberrations) | 3 (0.6) |
| Multiple diseases | 47 (10) |
- Note: n = number of patients.
- Abbreviation: COPD = chronic obstructive pulmonary disease.
2.5. Statistics
Demographic, social, disease, and treatment-related data were summarized via descriptive statistics. Table 2 shows patient characteristics of the study population. The overall population examined was divided into two groups: Group 1 included all patients who initially attended the PRS appointment, and Group 2 included patients who initially did not attend the first PRS appointment. The groups were compared with respect to the parameters collected. To this end, we performed univariate analysis using the t-test for age as a continuous variable. We performed the chi-square test to analyze categorical variables. Fisher’s exact test was applied only to categorical variables where the expected values were less than 5 in over 20% of the cells. These variables are marked with a raised cross (“#”). Table 3 provides an overview of all tested variables.
| Variable | ||
|---|---|---|
| Age in years | Mean (range) | 64.7 (34–88) |
| n (%) | ||
| Sex | Male | 209 (44.7) |
| Female | 259 (55.3) | |
| Insurance status | Privately insured | 385 (82.3) |
| Statutory health insurance | 83 (17.7) | |
| Distance to clinic | Urban area < 30 km outside the urban area > 30 km | 438 (93.6) |
| 30 (6.4) | ||
| Marital status | Married | 318 (67.9) |
| Single/widowed | 84 (17.9) | |
| Unknown | 66 (14.2) | |
| Children | Children | 274 (58.5) |
| No children | 58 (12.4) | |
| Unknown | 136 (29.1) | |
| Profession | Employed | 161 (34.4) |
| Not employed | 18 (3.8) | |
| Retired | 219 (46.8) | |
| Unknown | 70 (15) | |
| Alcohol consumption (regular) | Yes | 33 (7.1) |
| No | 282 (60.3) | |
| Unknown | 153 (32.7) | |
| Cigarette smoking (regular) | Yes | 48 (10.3) |
| No | 270 (57.7) | |
| Unknown | 150 (32.1) | |
| Diagnosis | Breast cancer | 259 (55.3) |
| Prostate cancer | 209 (44.7) | |
| T-Stage | Tis | 48 (10.3) |
| T1 | 190 (40.6) | |
| T2 | 141 (30.1) | |
| T3 | 80 (17.1) | |
| T4 | 9 (1.9) | |
| N-Stage | N0 | 392 (83.8) |
| N1 | 57 (12.2) | |
| N2 | 14 (3) | |
| N3 | 5 (1.1) | |
| M-Stage | M0 | 468 (100) |
| Relevant secondary diagnoses | Yes | 170 (36.3) |
| No | 298 (63.7) | |
| Preirradiated | Yes | 39 (8.3) |
| No | 429 (91.6) | |
| Surgery | Yes | 371 (79.3) |
| No | 97 (20.7) | |
| Chemotherapy | Yes | 87 (18.6) |
| No | 381 (81.4) | |
| Hormone therapy | Yes | 286 (61.1) |
| No | 179 (38.2) | |
| Unknown | 3 (0.6) | |
| Immunotherapy | Yes | 1 (0.2) |
| No | 467 (99.8) | |
| Acute toxicity (> Grade II° CTCAE) | Yes | 4 (0.9) |
| No | 464 (99.1) | |
| Late toxicity (> Grade II° according to LENT–SOMA) | Yes | 1 (0.2) |
| No | 461 (98.5) | |
| Unknown | 6 (1.3) | |
- Note: n = number of patients.
- Abbreviations: CTCAE = Common Terminology Criteria for Adverse Events; LENT–SOMA = Late Effects of Normal Tissue, Subjective Objective Management Analytics.
| Variable | PRS initially perceived N = 393 |
PRS initially not perceived N = 105 |
p value |
|---|---|---|---|
| n (%) | n (%) | ||
| Sex | 0.843 | ||
| Male | 163 (44.9%) | 46 (43.8%) | |
| Female | 200 (55.1%) | 59 (56.2%) | |
| Insurance status | 0.550 | ||
| Statutory health insurance | 292 (80.4%) | 93 (88.6%) | |
| Privately insured | 71 (19.6%) | 12 (11.4%) | |
| Distance to clinic | 0.741 | ||
| Inside urban area < 30 km | 339 (93.4%) | 99 (94.3%) | |
| Outside urban area > 30 km | 24 (6.6%) | 6 (5.7%) | |
| Marital status | < 0.001 | ||
| Living with a partner | 262 (72.2%) | 56 (53.3%) | |
| Living alone | 51 (14%) | 33 (31.4%) | |
| No data | 50 (13.8%) | 16 (15.2%) | |
| Children | 0.558 | ||
| Yes | 212 (58.4%) | 62 (59%) | |
| No | 48 (13.2%) | 10 (9.5%) | |
| No data | 103 (28.4%) | 33 (31.4%) | |
| Employment | 0.117 | ||
| Yes | 117 (32.2%) | 44 (41.9%) | |
| No | 17 (4.7%) | 1 (1%) | |
| Retired | 172 (47.4%) | 47 (44.8%) | |
| No data | 57 (15.7%) | 13 (12.4%) | |
| Alcohol consumption | 0.351 | ||
| Yes, regularly | 28 (7.7%) | 5 (4.8%) | |
| No | 213 (58.7%) | 69 (65.7%) | |
| No data | 122 (33.6%) | 31 (29.5%) | |
| Cigarette smoking | 0.030 | ||
| Yes | 30 (8.3%) | 18 (17.1%) | |
| No | 213 (58.7%) | 57 (54.3%) | |
| No data | 120 (33.1%) | 30 (28.6%) | |
| Diagnosis | |||
| Breast cancer | 200 (55.1%) | 59 (56.2%) | |
| Prostate cancer | 163 (44.9%) | 46 (43.8%) | |
| T-Stage | 0.879 | ||
| Tis | 37 (10.2%) | 11 (10.5%) | |
| T1 | 152 (41.9%) | 38 (36.2%) | |
| T2 | 106 (29.2%) | 35 (33.3%) | |
| T3 | 61 (16.8%) | 19 (18.1%) | |
| T4 | 7 (1.9%) | 2 (1.9%) | |
| N-Stage | 0.570# | ||
| N0 | 307 (84.6%) | 85 (81%) | |
| N1 | 42 (11.6%) | 15 (14.3%) | |
| N2 | 11 (3%) | 3 (2.9%) | |
| N3 | 3 (0.8%) | 2 (1.9%) | |
| Relevant secondary diagnoses/comorbidities | 0.230 | ||
| Yes | 122 (33.6%) | 48 (45.7%) | |
| No | 241 (66.4%) | 57 (54.3%) | |
| Preirradiated | 0.367 | ||
| Yes | 28 (7.7%) | 11 (10.5%) | |
| No | 335 (92.3%) | 94 (89.5%) | |
| Surgery | 0.164 | ||
| Yes | 289 (79.6%) | 81 (77.1%) | |
| No | 74 (20.4%) | 24 (22.9%) | |
| Chemotherapy | 0.480 | ||
| Yes | 65 (17.6%) | 22 (210%) | |
| No | 298 (82.1%) | 83 (79%) | |
| Hormone therapy | 0.133 | ||
| Yes | 216 (59.5%) | 71 (67.6%) | |
| No | 147 (40.5%) | 34 (32.4%) | |
| Immunotherapy | 1.000# | ||
| Yes | 1 (0.3%) | 0 | |
| No | 362 (99.7%) | 105 (100%) | |
| Acute toxicity (> Grade II° according to CTCAE) | 0.579# | ||
| Yes | 4 (1.1%) | 0 | |
| No | 359 (98.9%) | 105 (100%) | |
| Late toxicity (> Grade II° according to LENT–SOMA) | (< 0.001)#∗ | ||
| Yes | 1 (0.3%) | 0 | |
| No | 362 (99.7%) | 99 (94.3%) | |
| No data | 0 | 6 (5.7%) | |
| PRS time (year) | 0.113 | ||
| 1 | 120 (33.1%) | 28 (26.7%) | |
| 2 | 80 (22%) | 33 (31.4%) | |
| 3 | 74 (20.4%) | 22 (20.9%) | |
| ≥ 4 | 89 (24.5%) | 22 (20.9%) | |
| Age in years | 64.8 ± 10.7 | 64.35 ± 11.7 | 0.712 |
- Note: n = number of patients; bold p values represent statistically significant values.
- Abbreviations: CTCAE = Common Terminology Criteria for Adverse Events; LENT–SOMA = Late Effects of Normal Tissue, Subjective Objective Management Analytics; PRS = postradiotherapy surveillance.
- ∗see comment in text.
- #Calculated with Fisher’s exact test.
Based on the univariate analyses, a multivariable model was developed that considered all relevant factors that could influence nonparticipation in the initial PRS. A logistic regression model was used. This analysis included the variables that were significant in the univariate analysis. It was expanded to include potentially relevant factors found in the literature, such as sex, place of residence, and insurance status [7]. Multicollinearity was tested. The correlation between the predictors was low (r < 0.5), which suggests a lack of confounding due to multicollinearity [8–10]. The regression model was statistically significant, x2 (7) = 25.892, p < 0.001.
The same procedure was used to identify factors that improved the response to the telephone reminder. The two groups, “PRS initially not perceived but after reminder” and “PRS initially not perceived and also not after reminder,” were compared with respect to statistically significant differences in group composition.
To show the effect of the telephone reminder on the increase in the participation rate for the PRS, the proportions of appointments, who attended after the first telephone reminder and the second telephone reminder, were compared with the initial rate (PRS initially perceived), and the effect was tested for significance via a binomial test.
The statistical analysis was carried out via SPSS software (IBM SPSS Statistics 29, Chicago, IL, USA). Unless otherwise stated, testing was carried out at a significance level corresponding to α = 0.05.
3. Results
3.1. Analysis of Appointment Keeping Depending on Telephone Reminders
A total of 468 patients were included in the study. In total, 363/468 (77.6%) patients attended their initial PRS appointment. The attendance rate did not significantly differ between women (200/259; 77.2%) and men (163/209; 77.9%) (Table 2). Conversely, 105/468 (22.4%) did not attend their initial appointment. A total of 89/105 (84.7%) patients could be reached by telephone (=first telephone reminder, I1) and received an alternative appointment, which was attended by 71/89 (79.7%) patients. However, 18/89 (20.2%) patients did not attend the alternative appointment, and 10/18 (55.5%) patients were reached a second time by telephone (second telephone reminder, I2) and received a second alternative appointment. I2 was successful in 9/10 (90%) patients. The overall participation rate for PRS increased from the original 77.6%–92.7% (after I1, p < 0.001) to 94.7% (after I1 + I2, p = 0.06). The course of recruitment and appointments is shown in Figure 1.
I1 also had a positive effect on the participation rate with increasing time between the end of radiotherapy and PRS. In the first 3 years after radiotherapy, the average effect of I1 was 17.46% (13.5%–21.2%). The participation rate increased less strongly by 9% if radiotherapy had been completed 3 or more years before (Table 4).
| Year | Months since therapy end | Participated regularly n (%) | Participated after reminder n (%) | Increase (%) |
|---|---|---|---|---|
| 1 | 0–11 | 120/148 (81.1) | 140/148 (94.6) | 13.5 |
| 2 | 12–23 | 80/113 (70.8) | 104/113 (92) | 21.2 |
| 3 | 24–35 | 74/96 (77.1) | 91/96 (94.8) | 17.7 |
| > 4 | 36–72 | 89/111 (80.2) | 99/111 (89.2) | 9 |
3.2. Analysis of Factors That Influence Appointment Keeping
The variables marital status, cigarette smoking, and higher-grade long-term adverse events were significantly different between the “PRS initially perceived” and “PRS initially not perceived” groups. No significant difference was found between the two groups in any of the other variables.
Higher-grade long-term side effects occurred in only a single patient. For 6 patients, no data were available on higher-grade side effects. Due to this imbalance, no conclusions can be drawn about the possible influence of higher-grade long-term side effects on aftercare behavior.
Including the variables marital status, cigarette smoking status, sex, place of residence, and insurance status, multivariable analysis revealed that only marital status significantly affected adherence to the appointment (p < 0.001). Therefore, single persons are by the factor of 3.106 (95% CI: 1.767–5.458) more likely to not participate in PRS. None of the other variables significantly influenced the probability of nonparticipation in PRS. Smoking status was not significant in this multivariable model (Table 5). However, the univariate analysis revealed a trend toward significance for the “smoking” variable (p = 0.052 < 0.100).
| Binary logistic analysis (multivariable) | Category (baseline/comparison) | p value | Odds ratio 95% CI |
|---|---|---|---|
| Marital status | Living with a partner/living alone | < 0.001 | 3.106; 1.767–5.458 |
| Smoking | Nonsmoking/smoking | 0.052 | 1.961; 0.994–3.869 |
| Sex | Male/female | 0.247 | 0.754; 0.468–1.216 |
| Distance to clinic | Inside urban area < 30 km/outside urban area > 30 km | 0.862 | 1.088; 0.421–2.812 |
| Insurance status | Statutory health insurance/private insured | 0.087 | 0.552; 0.279–1.091 |
- Note: bold p values represent statistically significant values.
- Abbreviation: PRS, postradiotherapy surveillance.
3.3. Analysis of Factors That Influence the Response to Telephone Reminders
The “PRS initially not perceived but after reminder” and “PRS initially not perceived and not even after reminder,” groups were compared but did not significantly differ. Therefore, no in-depth analysis was carried out.
4. Discussion
The aim of this study was to investigate the influence of telephone reminders on the adherence of breast and prostate cancer patients to postradiotherapy follow-up and to identify factors that influence appointment adherence.
Our study revealed that initial appointment adherence for PRS was 77.6% among breast and prostate cancer patients, corresponding to a missed appointment rate of 22.4%, with no significant difference between these two diagnostic groups in terms of surrogate parameters for the follow-up behavior of women and men (77.2% and 77.9%, respectively). A first telephone reminder (I1) significantly increased the adherence to 92.7%, and a second reminder (I2) further increased the value to 94.7%. These results highlight the effectiveness of telephone reminders as a straightforward and cost-efficient way to improve appointment adherence.
Missing appointments are a well-known problem in the public health care system. They lead to the ineffective use of structural and personnel resources and are associated with avoidable costs. For example, the costs for missed general practitioner appointments in England amounted to 216 million pounds or 256 million euros in 2019 [11]. In Germany, comprehensive national data on the exact costs incurred due to missed medical appointments are not available. Although the health care systems of these countries differ, Germany can be estimated to incur costs of several hundred million euros annually because of missed doctor appointments. The rate of missed appointments in the healthcare sector fluctuates, varies greatly, and depends on a wide range of circumstances. The literature shows that between 15% and 30% of appointments are missed. These numbers vary considerably depending on the medical context and country [12–14]. Bauerle et al. reported rates of approximately 30% for patients who underwent aftercare following traumatic injuries [15]. Similar data are evident in other specialized fields, such as endocrinology and cardiology [7]. In contrast, medical fields such as pediatrics or dentistry have significantly lower rates of unattended appointments, approximately 15%. In addition, no-show rates vary across global regions [7]. The proportion of missed appointments in PRS has rarely been investigated and is estimated to be 20%–25% among breast cancer patients in Germany [16]. Holtgrave et al. reported that appointment adherence in PRS continuously decreases over the 5-year period among breast cancer patients; in particular, they reported a nonattendance rate of 11.9% at the beginning of the PRS phase that increased to over 60% after 5 years [3]. In our study, the nonparticipation rate among patients diagnosed with breast cancer and prostate cancer was 23%, but the rate of missed appointments fluctuated between 18.9% and 29.2% during the PRS period of 5 years, with no significant decrease in the late follow-up years (Table 4).
Several studies have investigated the factors that influence nonattendance in healthcare, such as marital status, employment status, or sex [17]. Our study revealed that single patients constitute a high-risk group compared to nonsingle people in terms of their participation in follow-up examinations after radiotherapy. Single patients were more than three times more likely to not attend PRS appointments. Single people have also been shown to be at greater risk of not attending their appointments in other medical contexts [17, 18]. Similar to our study, Hoyle et al. reported that single patients were less likely to attend follow-up visits after radiotherapy for head and neck tumors [19].
This high attendance rate of married patients at health and treatment follow-ups was attributed to the support and help of their family and community. Therefore, health care professionals should focus on single persons during follow-up care because they are at greater risk of missing appointments.
Cigarette smoking did not significantly influence appointment adherence in the multivariable analysis. However, it did significantly affect appointment adherence in the univariate analysis, with a trend towards significance in the multivariable analysis. Several studies have also reported a relationship between cigarette smoking and the risk of missed appointments [17, 20, 21]. This relationship could be related to interactions between different social and economic factors. Ramsey et al. reported that the prevalence of cigarette smoking is greater among people living alone than among people living in a relationship. Other circumstances associated with an increased prevalence of cigarette smoking are lower income and lower levels of education [22]. Individual risk factors, such as cigarette smoking, should therefore always be considered in the wider context of other factors. Future studies could help to understand this complex interaction between various demographic and social factors.
Sex was found to affect nonattendance in several studies. In the majority of studies, male sex was associated with nonattendance. However, other studies have shown an increased risk of nonattendance for females [18]. In our study, sex did not significantly affect appointment adherence: PRS attendance was high for both women and men (77.2% and 77.9%, respectively). One explanation for this could be the fact that cancer is perceived by society as a severe illness, leading to a strong need for safety, irrespective of sex.
The positive effects of follow-up reminders in various medical contexts are also emphasized in the literature [23, 24]. Liew et al. reported a positive effect of telephone reminders on reducing nonattendance in long-term follow-up care for patients with chronic diseases [23]. In the study by Bruns et al., nonattendance at postradiotherapy follow-up among breast cancer patients decreased from 18.1% to 13.1% when written reminders were used and to 6.3% when combined with two telephone reminders [16]. This finding suggests that methods such as telephone reminders, which are frequently used by patients and are part of their daily digital interactions, can positively influence adherence to treatment and care appointments.
Our results largely align with the rates reported in the literature, demonstrating that telephone reminders are an effective measure to improve adherence. Our results, in turn, confirm findings from other studies that have also reported improved adherence in various medical contexts through telephone interventions [25].
In a recent systematic review and meta-analysis, Werner et al. reported mixed results regarding the most effective reminder method. When comparing written reminder letters with telephone calls and SMSs, any reminder system decreased the no-show rate. Telephone reminders are more likely than written letters to motivate patients to keep their appointments. Similar results were found when phone calls were compared with SMS reminders. A combination of different reminder methods may be more effective than a single method [26].
Other forms of reminders, such as app-based reminders, can also be considered to improve attendance rates. In times of increasing staff shortages in the healthcare sector, these forms could represent a cost-effective alternative. However, they often lack the personal connection that a direct phone call offers. Studies have shown that direct contact over the phone is difficult to ignore and often results in higher adherence than more impersonal forms of reminders [27, 28].
In addition, app-based reminders require patients to have certain skills and smartphone technical capabilities. Both of these factors are often inadequate among (very) elderly patients. Another critical point is the issue of data protection, especially if the therapy was completed years ago. Different methods are naturally associated with different personnel and financial costs, which should be considered when choosing the optimal reminder method.
In this study, we focused on patients with breast and prostate cancer because these two entities accounted for the majority of all patients observed after radiotherapy during the study period.
The strength of this study lies in the homogeneous patient population that was followed up under the same conditions after radiotherapy. However, the follow-up examinations in this retrospective study were performed by different investigators at different times. However, the quality of the data collection can be considered acceptably consistent because the examination parameters are defined by the department itself. Other limitations of the study were its retrospective design and possible unrecorded factors leading to patient nonparticipation, which could cause the so-called “confounding bias.” In some cases, data on “cigarette smoking” status were unavailable, which led to uncertainty in the evaluation. The restriction to patients with breast and prostate cancer limits the generalizability of the results to other diagnoses. Furthermore, certain potentially relevant variables, such as psychological factors, were not recorded.
5. Conclusion
Our results suggest that the implementation of telephone reminders in routine PRS practice is an effective strategy to improve appointment adherence. This practice could ultimately improve the monitoring and treatment of late radiotherapy effects and consequently improve the quality of patient care in the long term. Other forms of reminders, such as SMS or app-based reminders, can also be considered to improve attendance rates, but the limitations mentioned above should be considered, and further investigation is needed. Furthermore, the factors that hinder compliance, such as having a single patient and smoking, should also be considered when setting the appointment. Strategies to better support difficult-to-reach patient groups are desirable.
Ethics Statement
This investigation was performed with the approval of the regional Hannover Medical School Ethics Committee. This article does not contain any studies with human subjects. The research described in the present manuscript was in accordance with both national law and the Helsinki Declaration of 1975 (including its most recently amended version).
Consent
Informed consent was obtained from all individual participants included in the study.
Conflicts of Interest
The authors declare no conflicts of interest.
Author Contributions
Idea: F.B,; reviewed the literature: T.L., B.B.S., and F.B.; conception and design: T.L., A.C.K., D.S., and F.B.; acquisition of data: T.L. and G.-H.H.; analysis and interpretation of data: T.L. and F.B.; manuscript draft (including preparation of figures and tables): T.L., B.B.S., D.S., and F.B.; manuscript revision: T.L., G.-H.H., B.B.S., A.C.K., D.S., and F.B. All the authors read and approved the final manuscript.
Funding
No funding was received for this manuscript.
Acknowledgments
The authors thank the AJE Support Team (https://www.aje.com) for the language editing pass as part of the preparation of the manuscript. Open access funding was enabled and organized by Project DEAL.
Open Research
Data Availability Statement
The datasets used and/or analyzed during the current study are available from the corresponding author upon reasonable request.




