The First Systematic Review and Meta-Analysis of Pharmacological and Nonpharmacological Procedural Treatments of Dark Eye Circles (Periorbital Hyperpigmentations): One of the Most Common Cosmetic Concerns
Abstract
Background: A notable trend has been observed toward procedural interventions for periorbital hyperpigmentation (POH), with a variety of pharmacological and nonpharmacological treatment modalities being introduced. This systematic review aims to provide a comprehensive evaluation of these diverse procedural treatments for POH in the medical literature.
Method: A systematic search was performed in major databases up to 2023, and studies were evaluated for clinical improvement, patient satisfaction, and adverse events. The retrieved studies were categorized as lasers and light therapies, chemical peels, PRP, carboxytherapy, fillers and injections, microneedling, and combination therapies.
Results: A total of 33 studies involving 1320 patients were evaluated. The meta-analysis of improvement rates revealed that lasers (fractional CO2 and Q-switched or long-pulsed Nd: YAG) and combination treatments (microneedling + chemical peels or fillers + lasers) demonstrated the highest efficacy, with 82% and 75% of patients experiencing excellent or good (> 50%) improvement, respectively. Chemical peels, carboxytherapy, and PRP were less effective, benefiting 63%, 54%, and 44% of patients in the same category, respectively. Although fillers and autologous fat injections showed marked improvement in 94% and 74% of patients, the comparison of their results was limited due to their representation by a single study in each category. Considering the meta-analysis of satisfaction rates, lasers and combination treatments also led, with 82% and 75% of patients expressing over 50% satisfaction with treatment, respectively. Adverse events were generally mild and transient across treatments. Common side effects of lasers included transient burning and erythema. The fractional CO2 laser was associated with discomfort, pain, and edema, with a shorter duration of swelling and erythema when combined with PRP. Q-switched and picosecond Nd:YAG lasers had higher postinflammatory hyperpigmentation rates compared to carboxytherapy and the picosecond 755-nm laser. The most common adverse effect of chemical peeling was erythema, with glycolic acid showing the maximum incidence.
Conclusion: This systematic review reveals that lasers and combination therapies are the most effective and satisfactory treatments for POH, with generally mild and transient adverse events. However, further studies comprising larger sample sizes, multiple-arm designs, and longer follow-ups are needed to enable more robust comparisons.
Summary
- •
What is known in this topic: Periorbital hyperpigmentation (POH), commonly known as dark eye circles, represents a multifactorial dermatologic concern characterized by epidermal and dermal melanin deposition, skin laxity-induced shadowing, vascular congestion, and specific facial anatomical structures.
- •
This complexity poses challenges in delineating the precise etiological pathways and their relative contributions to POH manifestation.
- •
Amid the growing demand in esthetic dermatology, a broad spectrum of treatments for POH has emerged, spanning from pharmacological agents (e.g., hydroquinone) to procedural interventions (e.g., platelet-rich plasma (PRP) and lasers), and a trend toward procedural treatments has been noticed.
- •
The reported efficacy and patient satisfaction rates of these treatments vary considerably, indicating a notable knowledge gap and the necessity for comprehensive evaluative studies to ascertain optimal treatment modalities.
- •
What this article adds: This systematic review and meta-analysis incorporated 33 studies, with a total of 1320 patients, to evaluate pharmacological and nonpharmacological treatments for POH, and data regarding efficacy, satisfaction, and adverse events were extracted.
- •
The meta-analysis of improvement rates revealed that lasers (fractional CO2 and Nd:YAG) and combination treatments (microneedling + chemical peels or fillers + lasers) demonstrated the highest efficacy, with 82% and 75% of patients experiencing excellent or good (> 50%) improvement, respectively.
- •
Carboxytherapy and PRP were less effective, benefiting 63%, 54%, and 44% of patients in the same category, respectively.
- •
While fillers and autologous fat injections indicated notable improvement in a significant majority of patients (94% and 74%, respectively), the evaluation of their effectiveness is constrained due to the limited representation of these treatments in the studies analyzed, with only one study for each treatment category contributing to these results.
- •
In the meta-analysis of satisfaction rates, lasers and combination treatments led with 82% and 75% of patients, respectively, expressing over 50% satisfaction.
- •
Additionally, chemical peel treatments and PRP treatments followed by 25% and 19% of patients reporting excellent satisfaction.
- •
Carboxytherapies also demonstrated notable satisfaction, with 46% of patients expressing contentment with the outcomes.
- •
Adverse events across different POH treatments were generally mild and transient.
- •
Lasers commonly caused transient burning and erythema, with fractional CO2 laser also showing discomfort, pain, and edema.
- •
Notably, combining CO2 laser with PRP reduced the duration of swelling and erythema.
- •
Q-switched and picosecond Nd:YAG lasers had higher rates of postinflammatory hyperpigmentation (PIH) compared to carboxytherapy and the picosecond 755-nm laser.
- •
Chemical peeling primarily led to erythema, particularly with glycolic acid (GA) peels.
- •
Significant heterogeneity was observed across POH treatment categories, particularly in chemical peels, carboxytherapy, and PRP.
- •
Efforts to reduce this variability through subgroup analysis and stratification by specific treatment settings and geographic location were unsuccessful, indicating the presence of complex, possibly unmeasured variables affecting treatment outcomes.
- •
This suggests that caution is needed when interpreting these results due to the potential masking of true treatment effects.
- •
The study emphasizes the need for personalized treatment strategies in managing POH, taking into account individual patient characteristics and specific causes of POH.
- •
It also highlights the importance of future research with longer follow-up periods and more comprehensive multistudy analyses to better understand the effectiveness and safety of different treatment options, thereby improving their applicability and success in treating POH.
1. Introduction
Dark eye circles, known as POH, represent a common and often challenging dermatological concern that can lead to significant esthetic and psychosocial concerns for affected individuals. The underlying etiologies and contributing factors of POH are multifactorial and may encompass a combination of epidermal melanin deposition, dermal melanin deposition, shadowing due to skin laxity, vascular congestion, and specific facial anatomical structure among other causes [1].
With the rise of esthetic dermatology and the increasing importance of facial aesthetics in various social and professional settings, there has been a surge in the demand for effective treatments of POH [2]. Over the years, a multitude of pharmacological and nonpharmacological treatments have been introduced. The former category mainly includes topical agents like hydroquinone, kojic acid, and arbutin which work by inhibiting melanin synthesis, whereas the latter encompasses procedural treatments such as PRP, chemical peels, laser therapies, carboxytherapy, cell therapies, microneedling, and filler injections. The efficacy and satisfaction rates reported for these treatments, however, vary widely [2], leading to a controversial uncertainty among both clinicians and patients.
Interestingly, there is a growing trend toward the adoption of nonpharmacological procedural treatments, as they often promise quicker and more noticeable results than their pharmacological counterparts. However, despite their popularity, a comprehensive review and meta-analysis of the procedural treatments is still lacking in the current literature [3].
This article presents the first systematic review and meta-analysis of pharmacological and nonpharmacological procedural treatments for POH, providing a comprehensive evaluation based on the most recent and relevant studies published in major databases. Through this meta-analysis, we aim to elucidate the most effective treatment modalities, assess patient satisfaction rates, and examine safety profiles, thereby identifying areas that warrant further investigation.
2. Methods
2.1. Protocol and Registration
This systematic review accompanies the Preferred Reporting Items for Systematic Reviews and Meta-Analyses (PRISMA) guidelines.
2.2. Eligibility Criteria
The population–intervention–comparator–outcomes–study design (PICOS) framework was used to identify eligible studies. Inclusion criteria included original studies that evaluated pharmacological or nonpharmacological procedural therapies for the treatment of POH and evaluated at least one of the efficacy, safety, and satisfaction in both sex and regardless of patients’ age. Treatments were considered procedural in this study which was applied by physicians or health care provided were included in this study consisting of single procedural therapies and combination procedural treatments.
The exclusion criteria consisted of all publications not meeting the above and non-English literature. Unavailable articles, review articles, medical hypothesis articles, in vitro studies, animal studies, periorbital rejuvenation without mentioning pigmentation, nonprocedural therapies (such as medical or patient-applied topical treatments), and pure surgical treatments were also excluded.
2.3. Databases and Search Strategy
Major databases including PubMed (Medline), Scopus, and Web of Science were investigated using comprehensive search syntaxes. The search was designed and conducted on February 15, 2023. The following keywords were implemented to construct the search syntaxes: “infraorbital dark circles” OR “infraorbital hyperpigmentation” OR “periorbital dark circle” OR “periorbital hyperpigmentation” OR “dark eye circles” OR “under-eye dark circle.” The search syntaxes within each database are demonstrated in Table 1.
| Database | Search strategy | Count |
|---|---|---|
| PubMed | “Infraorbital dark circles” OR “infraorbital dark circle” OR “infraorbital hyperpigmentation” OR “periorbital dark circle” OR “periorbital dark circles” OR “periorbital hyperpigmentation” OR “dark eye circles” OR “eye dark circles” OR “dark eye circle” OR “eye dark circle” OR “under-eye dark circle” OR (“idiopathic hyperchromia” AND “orbital”) OR “under eye circles” OR “idiopathic cutaneous hyperchromia of the orbital region” OR “dark circle” OR “orbital hyperpigmentation” OR “tear trough rejuvenation” OR “infra orbital rejuvenation” OR “periorbital rejuvenation” Filters: Clinical trial, randomized controlled trial, from 2010/1/1-3000/12/12 | 33 |
| Scopus | (TITLE-ABS-KEY (“infraorbital dark circles” OR “infraorbital dark circle” OR “infraorbital hyperpigmentation” OR “periorbital dark circle” OR “periorbital dark circles” OR “periorbital hyperpigmentation” OR “dark eye circles” OR “eye dark circles” OR “dark eye circle” OR “eye dark circle” OR “under-eye dark circle” OR (“idiopathic hyperchromia” AND “orbital”) OR “under eye circles” OR “idiopathic cutaneous hyperchromia of the orbital region” OR “dark circle” OR “orbital hyperpigmentation” OR “tear trough rejuvenation” OR “infra orbital rejuvenation” OR “periorbital rejuvenation”) AND PUBYEAR > 2009 AND PUBYEAR < 2024) AND (TITLE-ABS-KEY (random ∗ OR sham OR placebo ∗) OR TITLE-ABS-KEY ((singl ∗ OR doubl ∗) W/1 (blind ∗ OR dumm ∗ OR mask ∗)) OR TITLE-ABS-KEY ((tripl ∗ OR trebl ∗) W/1 (blind ∗ OR dumm ∗ OR mask ∗)) OR TITLE-ABS-KEY (control ∗ W/3 (study OR studies OR trial ∗ OR group ∗)) OR TITLE-ABS-KEY (clinical W/3 (study OR studies OR trial ∗)) OR TITLE-ABS-KEY (nonrandom ∗ OR “non random ∗” OR non-random ∗ OR quasi-random ∗ OR quasirandom ∗) OR TITLE-ABS-KEY (phase W/3 (study OR studies OR trial ∗)) OR TITLE-ABS-KEY ((crossover OR cross-over) W/3 (study OR studies OR trial ∗)) OR TITLE-ABS-KEY ((multicent ∗ OR multi-cent ∗) W/3 (study OR studies OR trial ∗)) OR TITLE-ABS (allocated) OR TITLE-ABS-KEY ((“open label” OR open-label) W/5 (study OR studies OR trial ∗)) OR TITLE-ABS-KEY ((equivalence OR superiority OR non-inferiority OR noninferiority) W/3 (study OR studies OR trial ∗)) OR TITLE-ABS-KEY (“pragmatic study” OR “pragmatic studies”) OR TITLE-ABS-KEY ((pragmatic OR practical) W/3 trial ∗) OR TITLE-ABS-KEY ((quasiexperimental OR quasi-experimental) W/3 (study OR studies OR trial ∗)) OR TITLE (trial) OR KEY (trial)) AND (LIMIT-TO (DOCTYPE, “ar”)) AND (LIMIT-TO (EXACTKEYWORD, “human”)) | 104 |
| Embase | (‘Infraorbital dark circles’ OR ‘infraorbital dark circle’/exp OR ‘infraorbital dark circle’ OR ‘infraorbital hyperpigmentation’ OR ‘periorbital dark circle’ OR ‘periorbital dark circles’ OR ‘periorbital hyperpigmentation’/exp OR ‘periorbital hyperpigmentation’ OR ‘dark eye circles’ OR ‘eye dark circles’ OR ‘dark eye circle’ OR ‘eye dark circle’ OR ‘under-eye dark circle’ OR (‘idiopathic hyperchromia’ AND (‘orbital’/exp OR ‘orbital’)) OR ‘under eye circles’ OR ‘idiopathic cutaneous hyperchromia of the orbital region’ OR ‘dark circle’ OR ‘orbital hyperpigmentation’ OR ‘tear trough rejuvenation’ OR ‘infra orbital rejuvenation’ OR ‘periorbital rejuvenation’) AND (‘case control study’/de OR ‘clinical study’/de OR ‘clinical trial’/de OR ‘clinical trial topic’/de OR ‘controlled clinical trial’/de OR ‘controlled study’/de OR ‘randomized controlled trial’/de) | 106 |
| Web of science | TI = (“infraorbital dark circles” OR “infraorbital dark circle” OR “infraorbital hyperpigmentation” OR “periorbital dark circle” OR “periorbital dark circles” OR “periorbital hyperpigmentation” OR “dark eye circles” OR “eye dark circles” OR “dark eye circle” OR “eye dark circle” OR “under-eye dark circle” OR (“idiopathic hyperchromia” AND “orbital”) OR “under eye circles” OR “idiopathic cutaneous hyperchromia of the orbital region” OR “dark circle” OR “orbital hyperpigmentation” OR “tear trough rejuvenation” OR “infra orbital rejuvenation” OR “periorbital rejuvenation”) AND (TS = clinical trial ∗ OR TS = research design OR TS = comparative stud ∗ OR TS = evaluation stud ∗ OR TS = controlled trial ∗ OR TS = follow-up stud ∗ OR TS = prospective stud ∗ OR TS = random ∗ OR TS = placebo ∗ OR TS = (single blind ∗) OR TS = (double blind ∗)) AND 2010 o 2023 (publication years) | 35 |
2.4. Study Selection
Endnote X9 (Clarivate Analytics, Philadelphia, USA) was used for study screening and data extraction. The title and abstract screening followed by full-text screening was conducted considering the inclusion and exclusion criteria. Disagreement situations regarding the inclusion process were resolved through negotiation, and the final decision was made by the principal investigator.
2.5. Extracted Items
Our data extraction sheet included the study’s first author, country of study, study type, number of arms, and patient demographics including number of recruited patients, mean age, gender distribution, and Fitzpatrick skin type. Also, details on the type of POH, number of patients in each arm, type of procedure, procedure parameters, pigment scoring methodology, pre- and post-treatment pigment scores, overall clinical improvement rate, and proportion of patients in each of the quartile improvement and satisfaction rates were retrieved. Furthermore, any reported adverse events were summarized.
2.6. Statistical Analysis
All statistical analyses were executed using STATA software (version 14.1, StataCorp LLC, College Station, TX, USA). For our meta-analysis, we employed the metaprop function. Given the anticipated variability between studies, a random-effects model was utilized to provide a conservative estimate of the pooled proportions. Our primary metrics for this were the proportions of patients within each quartile improvement category. The same was considered for satisfaction rates. Subsequently, a subgroup analysis was performed to evaluate the studies within each treatment type individually. Heterogeneity among studies was assessed using the I2 index.
3. Results
3.1. Study Selection
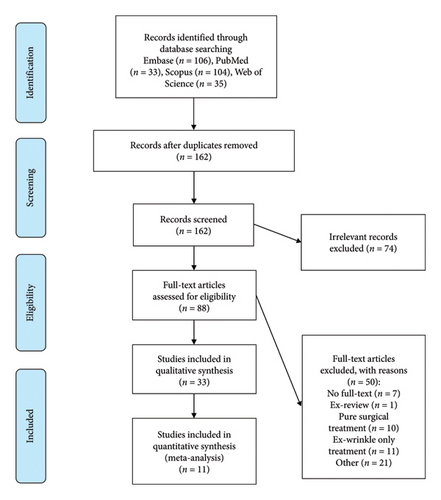
A total of 278 records were obtained from databases, and finally, 33 studies were considered eligible following full-text screening. The detailed screening process is visualized in the PRISMA chart in Figure 1. The selected studies comprised 12 one-arm studies, 17 two-arm studies, and 4 three-arm studies, recruiting a total of 1320 patients. The characteristics of these studies are detailed in Table 2. Meta-analysis was procurable only on quartile improvement rates and quartile satisfaction rates. To accurately determine the effect size for each treatment category, each arm of the comparative studies with two or more arms was analyzed independently. Consequently, 11 studies were included in the meta-analysis for both the improvement rates and the satisfaction rates.
| First author, year, country of study | No. of all patients (mean age/Mean age in each group) | Fitzpatrick skin type | Type of procedure (s) | Modality settings | Summary of improvement | Summary of adverse events |
|---|---|---|---|---|---|---|
| Nilforoushzadeh, 2021, Iran [4] | 32 (41.5) | NM | Fractional long-pulse Er: YAG laser PRP | — |
|
|
| Er: YAG laser | Long-pulse energy of 500–700 mill Joule | |||||
| Mehryan, 2014, Iran [5] | 10 (41.2) | III, IV | PRP | 10 mL of venous blood was centrifuged at settings of 1600–1800 G/6 min, followed by 2000G for 5 min. The resulting PRP, with platelets estimated to be 3–4 times more concentrated than whole blood, was activated with calcium chloride and then injected into specific facial areas using a 1-mL insulin syringe and a 30-g needle. |
|
Mild burning sensation experienced by all participants. Mild and transient bruising/echymoses reported in the first week or two after injection by 60% of participants. No participants reported any persistent or significant adverse events during the study period. |
| Bernardini, 2014, Italy [6] | 63 (42) | NM | Calcium hydroxyl-apatite (CaHa) | Injections were administered by a standardized technique with patients seated upright after applying an anesthetic cream. Using a 25-gauge blunt cannula, Radiesse mixed with 2% lidocaine was injected subcutaneously into the tear trough in a retrograde linear threading manner, with multiple passages delivering moderate product amounts. |
|
|
| Eyraud, 2021, France [7] | 35 (28.3) | I-V | Carboxytherapy | 3-Session injection protocol, |
|
|
| Dayal, 2016, India [8] | 90 (25.20–26.00) | NM |
|
|
|
|
| Yu, 2020, China [9] | 20 (NM) | NM | 1% phenylethyl resorcinol (PR) + nano-microneedle | Participants received topical PR gel under the left orbit once a day and topical PR plus nano-microneedle-assisted PR gel under the right orbit twice a week |
|
|
| Placebo gel with nano-microneedle on the right side. | Group C: Participants were assigned to treat with gel without PR (once a day) and similarly imported with nano-microneedle on the right side. Nano-microneedle treatment was applied twice a week, with the intervals of 3–4 days between sessions. | |||||
| Kontochristopoulos, 2016, Greece [10] | 13 (41.61) | II-IV | Microneedling and 10% trichloroacetic acid peel | The patients were treated with automatic microneedle therapy system—handhold and topical application of 10% trichloroacetic acid solution. A 0.5- to 1-mm derma roller was used and rolling was performed in both vertical and horizontal direction. Subsequently, the peeling agent was applied to each infraorbital area for 5 min. |
|
|
| Budania, 2021, India [11] | 21 (31.8) | NM | Novel PRP | The novel PRP was prepared using a single spin method from 16 mL of venous blood, with centrifugation at 100 g for 10 min, and low-temperature activation at 4°C for 15–30 min. The upper one-third of the plasma was discarded postcentrifugation, utilizing the lower two-thirds for PRP preparation. Additionally, 1 mL of PRP was cryopreserved for future assessment of growth factors, necessitating an extra 8 mL of blood collected during the initial procedure. |
|
|
| Conventional PRP | 16 mL of blood is spin at 160 g for 10 min, followed by a second spin of the collected supernatants and buffy coat at 400 g for 10 min. The resulting platelet pellet is resuspended in plasma and, in one instance, 1 mL of PRP was cryopreserved for assessing growth factors, with an additional 8 mL of blood collected. Before injection, PRP is activated with a 10% v/v calcium gluconate solution in a 1:9 ratio with PRP | |||||
| Zamanian, 2019, Iran [12] | 51 (41.85–42.71) | II-IV | Microneedling combined with using TCA 10% cream topically (MT group) | NM | The mean difference in skin darkening intensity was consistently higher in the laser group across all treatment sessions. Patients in the laser group reported greater satisfaction during the fifth visit. Overall, the combination therapy of fractional CO2 laser, microneedling, and TCA was found to be more effective in treating infraorbital dark circles. |
|
| Fractional CO2 laser (CL group) | The laser was transmitted with power: 15; stack: 1; pulse duration: 1000; and spacing: 1000. | |||||
| Nilforoushzadeh, 2021, Iran [4] | 28 (41.5) | II-IV | Carboxytherapy | A 30-G needle with an infusion velocity of 1 mL/s was used. In total, 2 mL of gas was administered on each side, and the average time of each session was 5–7 min. |
|
Carboxytherapy results in fewer side effects, including less erythema and postinflammatory hyperpigmentation, compared to Nd:YAG laser. |
| Fractional 10.64 nm Q-switched Nd:YAG laser | Fluency of 1.3 J/cm2, pulse rate of 5 hz, spot size of 7 × 7 mm, energy 500 spot size, and a pulse duration of 5 ns. | |||||
| Zaheri, 2023, Iran [13] | 30 (38.22) | Carboxytherapy |
|
Both treatment groups exhibited mild side effects, including: erythema, pain, and discomfort, without any significant differences between them. | ||
| Fractional CO2 laser therapy | ||||||
| Kounidas, 2022, United Kingdom [14] | 34 (NM) | I-V | Fillers | Juvederm 2 with canula was used in the tear trough area and Juvederm 3 lateral was used in the lower eyelids and around the rim with canula. One vial of Juvederm 3 was used in first session and one vial of Juvederm 2 at second session. | All three treatment modalities (fillers, CO2 laser, and nonsurgical options) were effective in reducing periorbital dark circles, depending on the underlying cause. Nonsurgical treatments proved capable of correcting and improving dark circles with minimal complications and downtime. |
|
| Q-switched Nd:YAG + long-pulsed Nd:YAG + fractional CO2 laser |
|
|||||
| Kounidas, 2022 [14] | Fillers and lasers combined | Lasers were done first and then fillers. | All three treatment modalities were effective in reducing periorbital dark circles, with effectiveness depending on the underlying cause. | |||
| Assaf, 2022, Egypt [15] | 31 (25.2) | II-IV | Carboxytherapy | 4–6 puffs/session (about 5 cc gas in each puff) |
|
Both treatments had a similar safety profile, with no significant difference between the two (p = 0.23). |
| Microneedling plus topical glutathione | 6500–10000 r/mand vibration speed level 5 | |||||
| Ghandehari, 2022, Iran [16] | 30 (44.9) | II-IV | Fractional CO2 laser | 10,600 nm fluences of 10–15 mJ/cm2, 0.8 mm distance, overlap 1 step, and repeat 1 s with scatter mode; two passes were, 2 cc of tranexamic acid (500 mg/5 mL) vial applied to the treatment area with a cotton swab, waiting until the drug completely absorbed. |
|
|
| Microneedling | Microneedling containing 12 sterile needles, 0.5–1 mm. Frequency from 100 to 150 Hz. Immediately after laser or microneedling procedure, 2 cc of tranexamic acid (500 mg/5 mL) vial applied to the treatment area with a cotton swab, waiting until the drug was completely absorbed. | |||||
| Behrangi, 2022, Iran [17] | 100 (NM) | Fractional CO2 laser | SmartXide DOT/DEKA fractional CO2 laser apparatus with a power of 10, stack of 2, and a density of 1. | The combination of platelet-rich plasma (PRP) with CO2 laser treatment led to a 25% reduction in periorbital hyperpigmentation (POH). This combined approach also increased satisfaction levels for both physicians and patients. Both the CO2 laser-only group and the CP group (CO2 laser and PRP) demonstrated significant reductions in assessed parameters during the follow-up period. Notably, the reduction in hyperpigmentation was higher in the CP group. |
|
|
| Fractional CO2 laser + PRP | Same laser parameters. For PRP. 5 mL of venous blood sample was extracted and diluted with 1.5 mL of adenine dextrose citric acid (ADCA) solution. Then, the solution was centrifuged (4000 rpm), and 2 mL of PRP was extracted. Finally, 1 mL of PRP solution was injected in each side of the POH area | |||||
| Ellabban, 2019, Egypt [18] | 42 (28.14) | Chemical peeling (TCA 3.75 + LA 15%) | The chemical peeling agent contains a combination of TCA 3.75% and lactic acid (LA) 15% in a gel form. It is applied in four layers to the infraorbital area, with a total session time ranging from 8 to 11 min, followed by rinsing with pure water. |
|
|
|
| PRP | The PRP procedure involves a two-step centrifugation of 10 mL of blood to isolate platelets, resulting in a 3-4 times concentrated PRP solution, which is activated with calcium chloride and microinjected using an insulin syringe. | |||||
| Kadry, 2023, Egypt [19] | 30 (31.6–32.3) | III-IV | Platelet-rich plasma | Tubex tubes and Selex centrifuge were used for all PRP patients. Blood samples (10 mL) were drawn from the participants’ medial initial centrifugation at 1500 rpm for 10 min. The plasma supernatant subjected to a second centrifugation step at 4000 rpm for 10 min. The upper section consisted of PPP, whereas the PRP collected at the bottom of the tube. PRP was activated by adding calcium chloride at a ratio of 10:1 |
|
|
| Microfat injection | The microfat was used first to fill the nasojugal and palpebromalar grooves by injecting the fat in the supraperiosteal plane using a 0.7-mm blunt cannula. A small bolus was injected in the nasojugal groove at the midpupillary line, followed by smooth distribution of the microfat over the rest of the treated area. Nanofat was then injected superficially all over the under-eye area using a 27-G needle | |||||
| Nofal, 2018, Egypt [20] | 30 (28.93) | II–IV | PRP | The PRP was prepared using a double-spin method from 10 mL of participants’ blood, concentrated through two centrifugation steps, and activated with calcium chloride. It was then microinjected into the periorbital areas using an insulin syringe via the mesotherapy technique. |
|
|
| Carboxytherapy | The used device was locally manufactured by a national company for esthetic and dermatological devices. Carbon dioxide gas was intradermally injected at the lateral one-third of each eye lid (5 cc gas in each puff according to standardized flowmetry) using 30 G needle; with infusion velocity 50 mL/min. | |||||
| Dayal, 2020, India [21] | 90 (24.7–26.43) | 20% glycolic acid peeling |
|
|
||
| 15% lactic acid peeling | ||||||
| 12% ferulic acid | ||||||
| West, 1998, USA [22] | 12 (44) | I–III | CO2 fractional laser |
|
Four patients experienced transient (for 8 weeks) infraorbital hyperpigmentation postoperatively. | |
| Bhat, 2022, India [23] | 20 (41.5) | MSC-CM along with antioxidants, in vitro using human melanocytes cultures |
|
No adverse events observed in any of the subjects | ||
| Shah-Desai, 2021, UK [24] | 165 [9] | Hyaluronic acid product | Depth of injection for each patient was subdermal using a serial puncture injection technique. The treatment was performed to a visual endpoint of small subdermal “bubbles” placed at regular intervals of 3–5 mm within the upper 1/3rd of the superomedial tear trough and the preseptal hollow. Three micro boluses were injected before the “click” was activated, estimating that 10 μL was delivered per micro bolus. No patients required greater than 0.2 cc of hyaluronic acid per subdermal placement per trough. |
|
|
|
| Asilian, 2021, Iran [25] | 21 (37.76) | III-IV | Carboxytherapy | Carboxytherapy was performed by injection of carbon dioxide gas once weekly for 6 weeks. The amount of 5 cc of CO2 was intradermally injected at the one-third lateral part of each eyelid using a 30-gauge needle with a velocity of 50 cc per minute. |
|
|
| PRP | 10 mL venous blood was taken from each of the patients centrifuged twice. 1st 150–200 g for 10 m at room temperature. 2nd 1500–2000 g for 15 m to separate the platelet-rich plasma from the platelet poor plasma. One cc of PRP injected in periorbital space. | |||||
| El-Tahlawi, 2022, Egypt [26] | 23 (NM) | III-IV | Carboxytherapy | A 32-G needle with 30°–45° injection angle was used. For injections in the lateral left periorbital area. A total amount of gas administered was 1-2 mL with flow rate of 1 cc/s. The average time for each session was between 5 and 7 min. |
|
|
| PRP | 6 mL of venous blood was withdrawn. Centrifugation twice. 1st at 377 g for 10 min. 2nd at 2504 g, separating PPP from PRP. PRP into the right periorbital area using a 32-G needle into the papillary dermis (1.5–2.0 mm deep) with injection angle at < 15° directing bevel border up using papule method which is one of mesotherapy techniques with (1.5–2.0 mm deep) into the papillary dermis with injection. As for the injection, upper lid needed two injections with 0.1 mL; lower lid needed five injections. | |||||
| Vanaman Wilson, 2018, USA [27] | 29 (49.43) | II-IV | PicoWay (1064 nm Nd:YAG + 532 nm KTP) laser | Treatment with a single session using dual-wavelength picosecond Nd: YAG laser in consecutive passes using the fractionated lens as follows: a single pass of 1064 nm at 1.3 J/cm2 and 5 hz, immediately followed by a single pass of 532 nm at 0.16 J/cm2 at 5 Hz for a total of 250 pulses between both eyes |
|
|
| Picosecond 755 nm alexandrite laser | 755 nm alexandrite laser via a fractionated lens with a 6 mm spot size and 0.71 J/cm2 fluence at 1–5 Hz in a single pass for a minimum of 50 pulse per eye to no more than 150 pulses combined between both eyes | |||||
| Wu, 2022, China [28] | 22 [28] | NM | Microneedling | Penetration depth 0.5 mm, fluency level 2, power 12.5 W, and duration 50 ms. |
|
|
| Roshdy, 2022, Egypt [29] | 80 (29.37–30.83) | III-IV | Carboxytherapy 30 mL/min | Same flow rate for both eyes. The duration of injection was fixed for both groups. |
|
|
| Carboxytherapy 60 mL/min | ||||||
| Manuskiatti, 2000, USA [30] | 11 (NM) | I–IV | Pulsed CO2 laser + Q-switched 755 nm | QS alexandrite laser immediately following the use of the pulsed CO2 laser. 3-mm spot size at a fluence of 8.0 J/cm2. | Combined treatment using appropriate lasers can offer an excellent therapeutic outcome for patients with multiple cosmetic complaints. | There were no complications that could be attributed to the simultaneous use of multiple lasers. |
| Cymbalista, 2006, Brazil [31] | 12 (NM) | II–IV | Intense pulsed light | Wavelengths of 515 to 1200 nm, in single, double, or triple pulses of 1–25 ms with intervals of 10–300 ms and fluences of 3–90 J/cm2. Probe tip dimensions of 8 35 mm and 10 45 mm were available. The HEPL application was performed using a cold gel layer between the probe tip and the skin. Filters of 515, 550, or 570 nm; fluences of 36–37 J/cm2; and double pulses of 2.6 and 4.0 ms with intervals between pulses of 20 ms were utilized. |
|
|
| Xu, 2011, China [32] | 30 (35.5) | — | Low-fluence 1064 nm Q-switched neodymium-doped yttrium aluminum garnet (QSNY) laser | Participants were treated using the low-fluence 1064 nm QSNY laser at 3- to 4-day intervals. A spot size of 3.5 mm was used, with a fluence of 4.2 J/cm2 and a repetition of rate of 5 hz. |
|
|
| Ahmed, 2019, Egypt [33] | 45 [6] | II–V | Carboxy therapy | A 32-G needle with an infusion velocity of 50 mL/min. In total, 3 mL of gas was administered on each side, with an average time for each session of 5–8 min. | No statistically significant differences were detected in improvements in pigmentation or the degree of patient satisfaction between any of the groups. However, the mesotherapy group reported more of a burning sensation following treatment than the other 2 groups but also showed a higher significant improvement in pigmentation and patient satisfaction compared with the carboxy group. Mesotherapy showed a significant improvement in pigmentation and a higher level of patient satisfaction compared with the other types of treatment. |
|
| Chemical peel agents (3.75% TCA, 15% lactic acid) | The duration of the first, second, and third layers of peel was 1-2 min, and the fourth layer was applied for about 5 min. The total time for a session ranged from 9 to 12 min. Then, the peel was neutralized with a wipe moistened with a 12% solution of arginine. | |||||
| Vitamin C mesotherapy (epidermal injection) | 10 mL was injected intradermally into both lower eyelids (5 mL for each eye)/Treatment was repeated 5 times at 1-week intervals. | |||||
| Diab, 2022, Egypt [34] | 40 (32.48) | PRP | 10 mL of venous blood were withdrawn and centrifuged at 320 g, for 15 min at 4°C. then centrifuged again for another 5 min at 1000 g to collect plasma sample: The upper part consisting of PPP and the lower part composed of PRP for injection. PRP was injected intradermally using 26-G needles in the Rt-sided periorbital area. The activated PPP (+calcium gluconate) was distributed into five 1.0-mL syringes and heated in a hot water bath at a temperature between 60°C and 100°C for 1 min and then in a cold bath at a temperature between 8°C and 0°C for 1 min. Finally, PPP was transformed into a viscous plasma gel and injected. |
|
No patients experienced severe complications (severe pain and/or erythema + ecchymosis and/or edema covering more than 2/3 of the eyelid area) following PRP injection compared to 10% of patients after plasma gel injection, and only 2.5% of the patients showed moderate complications (moderate pain and/or erythema + ecchymosis and/or edema covering two-thirds of the eyelid surface area) following PRP injection, while 17.5% of patients showed moderate complications following plasma gel injection, 45% of patients showed mild complications (mild pain and/or erythema + ecchymosis and/or edema over up to one-third of the eyelid surface area) after PRP and 40% of patients after plasma gel. | |
| Platelet poor plasma (PPP) | ||||||
| Banihashemi, 2021, Iran [35] | 30 (45.1) | Concentrated PRP (cPRP) | 2 sessions with a 3-month interval. PRP was prepared by first centrifugation at 2000 g for 2 min and then was prepared by second centrifugation at 4000 g for 8 min and the supernatant plasma was removed and precipitated platelets were resuspended in 5-mL plasma. 0.5 mL of 10% calcium gluconate was added for activation. |
|
|
|
The studies in this analysis were predominantly from Iran (30.6%), Egypt (25%), and India (13.9%), with notable contributions from the USA (8.3%) and China (5.6%). The inclusion of studies from the UK, Italy, France, Greece, and Brazil, each constituting 2.8%.
3.2. Meta-Analysis of Clinical Improvement Rates
Considering the results of the meta-analysis, the proportion of excellent improvement (75%–100%) was highest in the filler treatments, at 76%. It is important to note, however, that this result is derived from a single study, which may limit the generalizability of the findings. Laser and combination treatments both showed a significant proportion of 56% in the excellent improvement category. Autologous fat transfer was observed to have a 47% rate, and chemical peels registered a 25% rate. Notably, PRP treatments did not demonstrate any excellent improvement in the pooled effect size (Figure 2(a)).
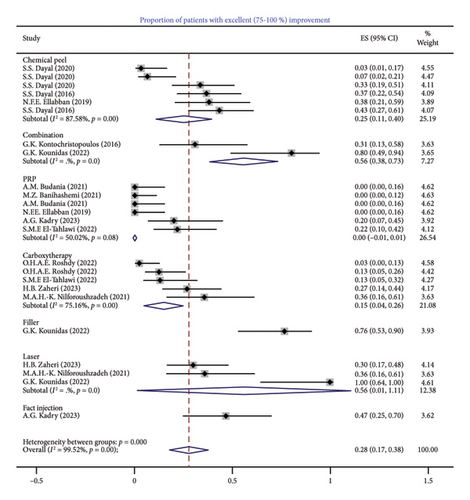
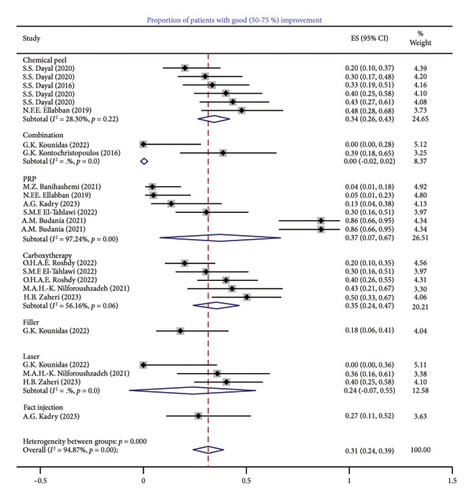
The good improvement rate (50%–75%) was predominantly observed in PRP treatments with a rate of 37%. This was closely followed by carboxytherapies at 35% and chemical peels at 34%. Autologous fat transfer treatments exhibited a rate of 27%, laser therapies of 24%, and filler treatments of 18%. Data for combination treatment in this category were not reported (Figure 2(b)).
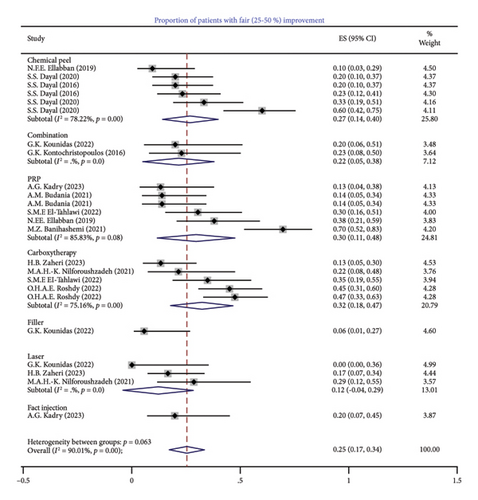
Regarding the fair improvement rate (25%–50%), carboxytherapies and PRP treatments were at rates of 32% and 30%, respectively. This was followed by chemical peelings at 27% and autologous fat transfer at 20%. Laser therapies showed a rate of 12%, and combination treatments of 22%. Filler treatments, despite their high rate in the excellent improvement category, showed a lower rate in the fair improvement category at 6% (Figure 2(c)).
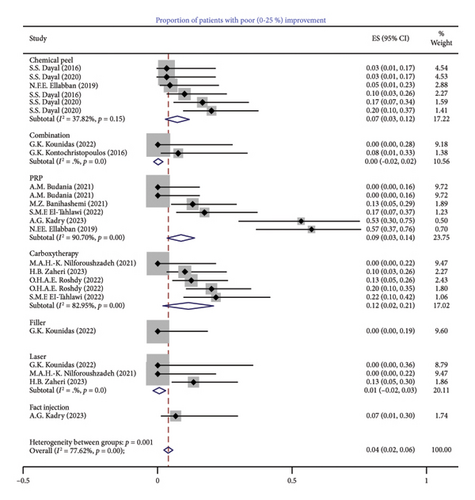
In the category of poor improvement rates (< 25%), PRP treatments showed the highest rate at 9%, with carboxytherapy following at 12%. Autologous fat transfer and chemical peels were recorded at 7%. The lowest rate was observed in laser therapies at 1%, and both fillers and combination treatments did not exhibit poor improvement rates (Figure 2(d)).
In summary, while filler treatments demonstrate a high rate of excellent improvement, the findings must be interpreted with caution due to the limitations of single-study data. Both laser and combination treatments showed substantial effectiveness, particularly in achieving excellent outcomes. Fat transfer treatments also indicated significant efficacy across various improvement categories.
PRP treatments, while not achieving high rates in the excellent category, were prominent in the good improvement category, suggesting efficacy in moderately effective outcomes. Chemical peelings and carboxytherapies exhibited balanced outcomes across the different improvement categories.
Conclusively, the data indicate that filler treatments may be highly effective in achieving excellent outcomes, but the generalizability of this result is constrained. Laser and combination treatments were discovered to be considerably effective, and fat transfer treatment demonstrates notable efficacy. PRP, chemical peelings, and carboxytherapies exhibit a consistent range of outcomes across the spectrum of improvement categories.
3.3. Meta-Analysis of Satisfaction Rates
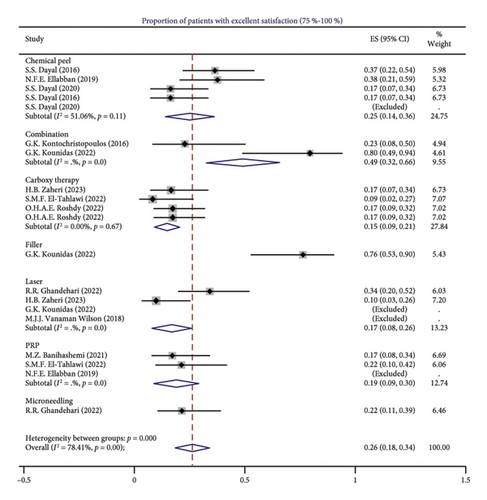
The meta-analysis of pooled satisfaction rates revealed that combination treatments were the most favorable, with 49% of patients reporting an excellent satisfaction rate (> 75%). This was followed by chemical peel treatments and PRP treatments, with respective rates of 25% and 19%. Laser and carboxytherapies were associated with lower proportions of excellent satisfaction, at 17% and 15%, respectively (Figure 3(a)).
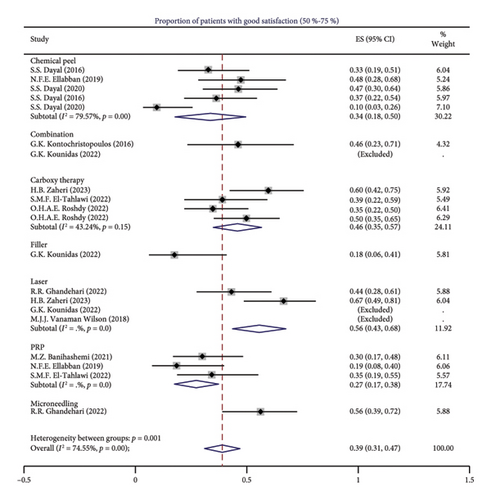
Within the good satisfaction rate (50%–75%) category, laser treatments were predominant, with 56% of patients expressing good satisfaction. Carboxytherapies also demonstrated notable satisfaction rates, with 46% of patients reporting contentment with the outcomes. Chemical peel and PRP treatments exhibited comparable trends, with approximately one-third of patients (34% and 27%, respectively) categorizing their satisfaction as good (Figure 3(b)).
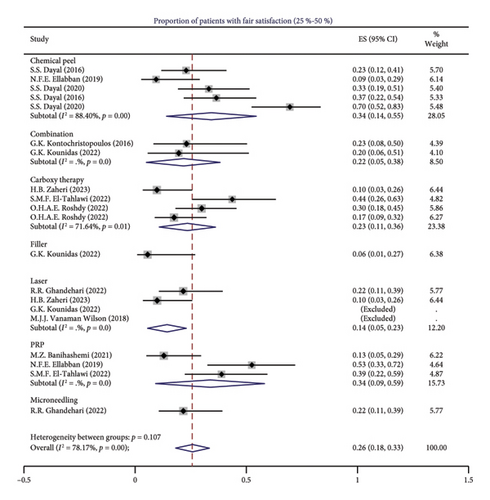
The rates of patients reporting fair satisfaction (25%–50%) were relatively similar across treatment modalities. Chemical peel and PRP treatments both reported 34%, while carboxytherapy, combination, and laser treatments recorded rates of 23%, 22%, and 14%, respectively (Figure 3(c)).
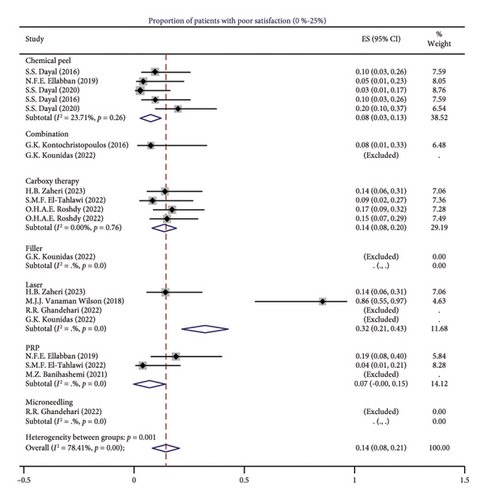
In the poor satisfaction category (< 25%), the highest proportion was observed in laser treatments at 32%, followed by carboxytherapy at 14%, and chemical peel and PRP treatments at 8% and 7%, respectively (Figure 3(d)).
Summarizing the overall satisfaction rates, patients demonstrated a marked preference for combination therapies, particularly with nearly half reporting excellent satisfaction. While laser treatments were notable in the good satisfaction category, the elevated rates of poor satisfaction warrant further investigation. Both chemical peel and PRP treatments exhibited limited patient satisfaction, with only 24% and 17% of patients, respectively, reporting excellent or good satisfaction levels. Although studies for fillers yielded high satisfaction rates, the inclusion of only one study precluded its analysis in this meta-review. Consequently, the cumulative satisfaction rates rank the treatment modalities as follows: combination therapies, lasers, chemical peelings, PRP, and carboxytherapy.
3.4. Analysis of Adverse Events
The meta-analysis of adverse events was not achievable given the lack of consistent measurement of adverse events across studies. Almost all the mentioned side effects in eligible studies were mild, tolerable, and transient. Common side effects of lasers were transient burning sensation and erythema lasting for a week [36]. Adverse events related to CO2 laser were discomfort and local pain, erythema, and edema [12, 13, 16]. PIH was mentioned in only one study which lasted 8 weeks. These side effects were minor and temporary and did not significantly different from carboxytherapy [13]. The duration of edema, burning sensation, and itching persisted were not significantly different from microneedling, but erythema with microneedling did significantly last longer than fractional CO2 laser [16].
The combination of PRP and CO2 laser was associated with a significantly shorter duration of swelling (2.94 ± 0.68 days) and erythema (3.40 ± 0.76 days) compared to CO2 laser alone (swelling: 4.58 ± 0.61 days, erythema: 5.20 ± 0.76 days; p < 0.001).
The average patient receiving combination laser treatments in a single session experienced a reduced healing time of 2-3 days, compared to those previously treated with CO2 laser alone (7–10 days vs. 9–12 days) [30].
Side effects with Q-switched and picosecond ND:YAG laser were tolerable pain, transient edema, and erythema [27, 32, 37]. It is noticeable that the higher rate of PIH with this specific laser was mentioned which was last on day 60 of the follow-up session [27, 37]. Side effects were not observed by picosecond 755-nm alexandrite laser [27] and were less in the carboxytherapy group [37].
Side effects of Er:YAG laser treatment include contact dermatitis, redness, and dryness of the skin [4].
Residual hypochromia was presented in 58.33% of the patients receiving IPL for POH. Of these, 57.1% presented disappearance of the hypochromia after a median of 7.11 months [31]. Following PDL treatments, all lesions immediately turned purpuric, with the purpura resolving within 7–10 days without any pigmentary changes or scarring [30].
Regarding treatment of POH with chemical peeling, the most common adverse effect was erythema following mild discomfort and burning, irritation, edema, itching, and dryness; however, these were only temporary and did not warrant cessation of treatment. PIH and hypopigmentation were not observed in any study [8, 10, 18, 21]. Maximum incidence of side effects was observed with GA peel [21]. The occurrence of adverse events with chemical peeling was not significantly different from the PRP method [18]. In a study comparing carboxytherapy, chemical peeling, and mesotherapy, though no significant differences were found in overall complications, the carboxytherapy group reported more pain and eyelid edema (26.7%) and hematoma (20%), while the vitamin C mesotherapy group experienced more frequent burning sensations (26.7%) [33]. Reported side effects in combination of microneedling with 10% trichloroacetic acid (TCA) peels were temporary mild discomfort, transient erythema, and edema with only one patient developing periorbital dermatitis which resolved with a 1-week treatment with topical corticosteroid [10].
Pain, edema, and ecchymosis were the most considered side effects of PRP. The pain would subside in a few hours, and the edema and bruising would resolve in about 3 days [5, 11, 35]. No noticeable difference was detected between novel and conventional PRP regarding complications [11]. Side effects of plasma gel were significantly more severe than PRP [34].
In three studies comparing PRP to carboxytherapy, all mentioned significantly higher incidence of edema and swelling in the carboxytherapy group and ecchymosis in the PRP group. There was no significant difference regarding the pain of these procedures, and it was tolerable [20, 25, 26]. One study mentioned shorter down time with PRP intervention compared to carboxytherapy [26].
Carboxytherapy has been described as a painless procedure [7]. Edema, erythema, and ecchymosis along with headaches were among reported side effects which was notably higher in the higher rate carboxytherapy group [29].
Bruising (60.61%) was the most common side effect of hyaluronic acid (HA) injection following the Tyndall effect (1.82%) and swelling (1.21%). Visible eyelid bumps were resolved in 4 days [24]. Three considerable complications of calcium hydroxyl-apatite injections were migration of filler, worsening of the appearance, and overcorrection, while no palpable lumpiness or unevenness was detected [6].
Erythema was the most common adverse effect of microneedling which disappeared in a day with nano–micro needling [9]. No side effects were reported in the microneedling fractional radiofrequency system [28]. Microneedling with topical glutathione caused ecchymosis, while carboxytherapy reported no side effects [15].
3.5. Evaluation of Heterogeneity Among Studies
Despite the evident benefits of various treatments for POH, a high heterogeneity among the treatment categories was noticed. This heterogeneity is evident in the chemical peel, carboxytherapy, and PRP treatments, as indicated by their respective I2 value. Moreover, the calculation of I2 index was not procurable due to much fewer studies in fillers, autologous fat injection, and combination treatments.
The subgroup analysis, which aimed to reduce variability by pooling data from analogous treatment modalities, revealed that the I2 index remained elevated. For instance, the chemical peeling treatment demonstrated significant heterogeneity across all improvement rates, ranging from 28.30% to 87.57%. Carboxytherapies were similar with I2 indexes from 56.6% to 75.81%, and PRP showed considerable heterogeneity in the good and fair improvement rates, reaching up to 97.24%. The lowest heterogeneity in excellent improvement rates was for PRP treatments at 50.02% and for chemical peelings across good improvement rates, at 28.30% revealing more consistent results.
Further efforts were made to reduce heterogeneity within subgroup categories by distinguishing studies based on specific modality settings and also based on the country of study. For example, for PRP treatments, studies were differentiated based on the number of sessions and intervals between each session. Similarly, for chemical peel treatments, effect sizes were stratified based on the type of peeling agent used. Laser treatments were similarly categorized by laser type. Despite these stratifications, it was observed that such distinctions did not significantly decrease the heterogeneity. This persistence of heterogeneity underscores the complexity of these treatment modalities for POH and suggests the influence of additional, possibly unmeasured, variables that might contribute to the observed variability in outcomes. Therefore, interpretation of the results warrants extra caution, as the variability can mask the true effects of the treatments and impede the generalizability of the results.
4. Discussion
4.1. Summary of Findings
From a pool of 33 selected articles, 12 studies investigated the effectiveness and safety of lasers in addressing POH. The CO2 laser emerged as the most commonly used laser, demonstrating significant outcomes and presenting a promising approach for POH treatment. Conversely, the Nd:YAG laser yielded inconclusive results, showing improved efficacy in treating pigmented types of POH.
Six studies explored the use of chemical peels, with TCA being the most extensively studied. Notably, GA was identified as the most efficient peeling agent, despite its association with higher complication rates.
In 11 articles, PRP was investigated as a therapeutic option for under-eye circles. While most trials reported promising results for POH treatment, there was considerable diversity in the centrifugation settings employed across these studies.
Nine eligible studies incorporated carboxytherapy as a treatment for POH, yielding noteworthy outcomes. Additionally, six studies utilized HA and calcium hydroxyapatite (CaHa) fillers, vitamin C mesotherapy, and nanofat injection. Microneedling was mentioned in six clinical trials. Finally, a combination of different procedures was employed in the treatment of under-eye hyperpigmentation, leading to a spectrum of outcomes.
4.2. Lasers and Light Therapies
Lasers and light modalities have been extensively explored for the treatment of POH, with various studies employing different laser types and combinations. Twelve out of 33 eligible studies utilized various modalities, including fractional CO2 laser, Nd:YAG laser, picosecond 755-nm alexandrite laser, Er:YAG laser, IPL, and laser combinations as therapeutic procedures for POH.
The fractional CO2 laser emerged as a frequently studied modality in the context of infraorbital hyperpigmentation. This procedure resulted in remarkable improvement of POH in all studies. Most employed protocol was three monthly sessions. Reported side effects were mild and temporary. The study by West and Alster demonstrated a 50% improvement in hyperpigmentation following CO2 laser resurfacing. However, it is noteworthy that melanin reflectance spectrometry did not align with clinical findings, and transient PIH occurred in 33% of patients [22].
Zaheri et al.’s split-face randomized clinical trial favored CO2 laser over carboxytherapy in four sessions at 2-week interval, showing higher patient and physician assessments and no significant side effects post-treatment [13].
The study by Zamanian et al., which compared three monthly sessions of fractional CO2 laser (power 15; stack 1; pulse duration 1000; and spacing 1000), three-session combination of microneedling and topical TCA 10% 1 month apart, revealed interesting insights. The laser group resulted in significantly higher improvement in both patient and physician satisfaction than the use of 10% TCA after microneedling. While the trend of the change in ΔE (the difference in the intensity of darkening at the periorbital region and other points of the face) was decreasing in the laser group, it was inconsistent in the other groups. Reported complications in the laser group were temporary erythema and pain [12]. Another study incorporating topical tranexamic acid post-treatment showed significant improvement with both methods, with the laser side exhibiting superior results on day 60 (p value = 0.008). The average number of days that edema, burning sensation, and itching persisted were not significantly different between both sides, but erythema with microneedling did significantly last longer than fractional CO2 laser [16] (p value = 0.014).
Combining three monthly sessions of CO2 laser with PRP in the treatment of POH yielded promising results. The study by Behrangi et al. demonstrated a 25% reduction in hyperpigmentation when PRP was added to CO2 laser, along with increased satisfaction among patients and physicians. The duration of swelling and erythema post-treatment was significantly reduced in the combined treatment group (p < 0.001) [17].
The second most investigated laser was the Nd-YAG laser. Xu et al. demonstrated that eight sessions three to four days apart of the low-fluence 1064-nm Q-switched neodymium-doped yttrium aluminum garnet (QSNY) laser, set at spot size of 3.5 mm, fluence of 4.2 J/cm2, repetition rate of 5 Hz, and with two passes resulted in 93.3% patient satisfaction and substantial reductions in the melanin index (MI) from 225.84 at baseline to 182.65 after eight treatment sessions (p > 0.05). Reported complications were mild pain (mean score of 2.43 on a scale of 1–10), transient erythema, and slight edema [32].
Another study comparing six weekly sessions of Q-switched Nd:YAG laser (fluency of 1.3 J/cm2, pulse rate of 5 Hz, the spot size of 7 × 7 mm, energy 500, pulse duration of 5 ns), with carboxytherapy (2 mL of gas per side), for pigmented and vascular types of dark circles showed a significant difference in the melanin content of the periorbital skin before and after treatment in the carboxytherapy group (200.19 ± 75.94 and 101.25 ± 12.24) compared to the Q-switched Nd:YAG laser group (220.19 ± 75.94 and 151.25 ± 12.24), respectively (p < 0.05). The results showed that both are effective in the treatment of periorbital dark circles, favoring carboxytherapy, demonstrating superior effectiveness and minimal side effects such as erythema and PIH [37]. Opposed to the CO2 laser discussed earlier, carboxytherapy was more effective than the Nd-YAG laser.
In a clinical trial, the dual wavelengths of 532 and 1064 nm in consecutive passes were compared to the picosecond 755-nm laser. Despite the dual-wavelength group, the mean hyperpigmentation score at day 60 in the picosecond 755 laser group decreased significantly from the baseline. Adverse events were mild and temporary, including edema, pain, bruising, and hyperpigmentation [27].
Nilforoushzadeh et al. concluded that the combination of fractional Er-YAG laser with autologous PRP demonstrated significant changes in periorbital skin color, with decreased melanin content and increased skin lightness compared to Er-YAG laser alone. The percentage of change in the color of the periorbital skin after treatment on the combination side was 34.67 ± 12.16, and on the Er-YAG laser side was 17.01 ± 12.14 (p < 0.05). The patients and physician assessments confirmed the measured results [4].
Interestingly, one study revealed that the combination of lasers, such as the Q-switched alexandrite laser immediately following the pulsed CO2 laser, proved highly effective, achieving 75%–100% clearing of brown hyperpigmentation by 6 months after treatment [30].
While light therapy, specifically IPL, was explored in only one study, it showed statistically significant results, both clinical and histopathological, in clearing lower eyelid skin with maintained effects over a year. However, discomfort, erythema, edema, and alterations in skin color were observed during sessions [31].
Altogether, the most reported efficient laser was the CO2 laser. The side effects were minor, and some studies reported contact dermatitis, dryness of the skin, erythema, local pain, transient (for 8 weeks) infraorbital hyperpigmentation postoperatively, and edema. Lasers were reported as a tolerable procedure.
4.3. Chemical Peelings
Six studies out of 33 included studies have investigated chemical peelings for the treatment of POH.
The efficacy of different chemical peelings has been compared in a couple of studies. In a triple-arm study, Dayal et al. evaluated the application of a 20% GA peel every 3 weeks, a 15% lactic acid (LA) peel every 3 weeks, and daily 20% vitamin C for 12 weeks for periorbital melanosis. Improvement of at least 50% in POH grade was observed in 73.34% of patients on the GA peel, 56.67% on the LA peel, and 26.67% on topical vitamin C application. The most efficient procedure, albeit accompanied by a higher rate of complications, was GA, followed by LA and topical vitamin C. Reported adverse events included erythema, burning, irritation, itching, and dryness, with rates of 33.33%, 20%, and 10%, respectively [8].
In another triple-arm clinical trial, Dayal, Sangal, and Sahu compared three different chemical peelings: 20% GA peeling, 15% LA peeling, and 12% ferulic acid peeling in three different groups, performed at 3-week intervals for 12 weeks. At least a 50% improvement in POH grade was observed in 76.66% of patients in the GA peel group, 23.33% in the LA peel group, and 46.66% in the ferulic acid peel group. Physician and patient global assessments were significantly higher in the GA peeling group, while there was no significant difference in the other two groups. In terms of safety and tolerability, 12% ferulic acid was the best peel, followed by 15% LA and 20% GA. Reported side effects included itching, dryness, erythema, and a burning sensation [21].
Chemical peels have been compared with different modalities regarding POH treatment efficacy. Ahmed, Mohammed, and Fatani evaluated three different modalities for POH treatment: carboxytherapy, 3.75% TCA, and 15% LA gel with vitamin C mesotherapy administered once a week for 5 weeks. According to their data, no significant differences were observed among these three modalities regarding the improvement of POH score, patient satisfaction, and side effects [33].
Another modality compared to chemical peeling is PRP. The data demonstrated that TCA 3.75% and LA 15% in a gel formula significantly improved the degree of POH with better patient satisfaction compared to PRP. Additionally, there was no significant difference in adverse events among these modalities. The peeling group reported redness, itching, burning, edema, and pain [18].
Totally, the most commonly used peeling was TCA. The most effective peeling reported was GA; however, the adverse effects of using this chemical were higher among these peelings. Adverse effects observed included erythema, burning, irritation, itching, and dryness.
4.4. PRP/Platelet Poor Plasma
Out of the 33 articles considered, 11 explored PRP and plasma extractions as therapeutic options for POH. In a clinical trial led by Banihashemi et al., the effectiveness of two sessions of PRP separated by a 3-month interval was assessed for facial rejuvenation using the mesotherapy technique. The PRP was prepared through a two-step centrifugation process: first at 2000g for 2 min, followed by a second centrifugation at 4000g for 8 min. The study demonstrated optimal outcomes in the reduction of periorbital dark circles and wrinkles. A 3- and 6-month follow-up revealed significant improvements according to patient evaluation (47.8%, 60.9%), therapeutic physician’s evaluation (47.9%, 74%), and blind dermatologist assessment (34.8%, 52.2%). Side effects included transient edema and bruising [35]. Mehryan et al. confirmed these results, with statistically significant improvement in infraorbital color homogeneity (p = 0.010) and 80% of patients achieving fair-to-good improvement after 3 months. Although no statistically significant changes were observed in melanin content, side effects were transient bruising and a burning sensation. PRP was employed in a single session with centrifugation setting 1600–1800 G/6 min for the first cycle and 2000 G/5 min for the second cycle [5].
Several studies evaluated plasma extractions for POH treatment. In a split-face clinical trial comparing two monthly sessions of PRP and plasma gel of PPP for periorbital rejuvenation, no significant improvement in melanin concentration was observed at any follow-up visits. Side effects included pain, erythema, ecchymoses, swelling, and a feeling of pressure. The centrifugation setting in this study was 320 g for 15 min at 4°C followed by 1000 g for 5 min [34].
Another study compared novel PRP (using a single centrifuge done at 100g for 10 min without a calcium activator) with conventional PRP (with double-spin method 160 g for 10 min followed by 400 g for 10 min) injected in three sessions at 4-week intervals for POH treatment. No significant differences in growth factors or platelet count were found between groups. While the mean improvement of POH and visual analog scale (VAS) score change significantly improved after treatment, the difference between the two modalities was not significant. The Dermatology Life Quality Index (DLQI) decreased significantly, with side effects being mild pain and bruising [11].
In a different study, PRP showed a significantly better response (p = 0.002), shorter downtime, and tolerable side effects compared to carboxytherapy. Reduction in melanin area percent after PRP injections showed a 46.6% improvement, while carboxytherapy showed only a 14.3% improvement [26].
Chemical peeling was reported to be more effective for POH treatment compared to PRP, although both modalities showed effective results, with reported side effects of pain, edema, and ecchymosis [18].
Finally, Kadry et al. compared autologous fat transfer with nanofat with PRP, finding statistically significant differences favoring the autologous fat transfer group in clinical improvement and patient satisfaction. Minimal bruises and ecchymosis were reported as adverse events [19].
4.5. Carboxytherapy
Carboxytherapy was employed as a therapeutic procedure in 9 out of 33 eligible studies. Eyraud et al. treated 35 patients with under-eye circles through three weekly carboxytherapy sessions. After 6 months, the mean score of POH significantly improved, as assessed by three graders and patient evaluations. Only slight discomfort and a burning sensation were reported [7].
In another study by Roshdy, Abd Elall, and Eid, the impact of flow rates (30 vs. 60 mL/min) on the therapeutic outcome of 6 weekly sessions of carboxytherapy for infraorbital dark circles was assessed. Dark circle grade, infraorbital hollow scale, melanin, and erythema indices significantly improved in both groups, but the difference between the two flow rates was not significant. Side effects were notably higher in the group receiving the higher flow rate, including heaviness, puffiness, headaches, pain, erythema, and ecchymosis [29].
Various therapeutic procedures, such as laser, chemical peeling, and PRP, have been compared with carboxytherapy, as discussed previously. Carboxytherapy was favored over Q-switched Nd:YAG laser [13] but proved less effective than fractional CO2 laser [37] for POH. No significant difference was found between carboxytherapy and chemical peeling regarding POH improvement [33]. While two studies indicated carboxytherapy’s effectiveness similar to PRP, another study suggested carboxytherapy to be less effective with more adverse effects.
In a split-face clinical trial comparing microneedling, Assaf, Ahmed, and Abdelhamed found that carboxytherapy showed higher efficacy than microneedling with topical glutathione in POH patients. This was evident in VAS evaluation; dermoscopic vascular, skin, and pigmentation evaluation; DLQI; and patient satisfaction, with no reported side effects [15].
4.6. Fillers and Injections
In 6 out of 33 studies, fillers and other injections were employed for the treatment of POH. Shah-Desai and Joganathan introduced a novel technique involving HA filler injection under the eyes. Microdroplets of a low molecular weight cross-linked stabilized HA filler were subdermally injected into the lower eyelid and medial zone of the tear trough. This approach resulted in a reported visual improvement in dark circles for 98% of patients at the 3-month follow-up, with 97% showing enhancement in the Global Aesthetic Improvement Scale (GAIS) scoring at the 6-month follow-up. Adverse effects included bruising, eyelid bumps, swelling, and the Tyndall effect [24].
Bernardini et al. used calcium hydroxyl-apatite (CaHa) fillers subcutaneously with a 25-gauge cannula for dark circle and tear trough correction. At the 1-month follow-up, patients reported a 92% improvement rate, supported by a 92.5% improvement in objective assessment. Notably, patients with the chief complaint of “infraorbital hollows” showed the highest subjective satisfaction rate (98% improvement) followed by “dark circles” improvement in 68% of patients. Complications included mild erythema, swelling, superficial dermal yellowish discoloration (“Pseudoxanthelasma” effect), migration of the product, worsening appearance, and overcorrection [6].
Kounidas, Kastora, and Rajpara evaluated nonsurgical options, including two sessions biweekly HA fillers with cannula used in the tear trough area and lower eyelids, three sessions 6 weeks apart lasers, and combinations thereof, for dark circles. All options were effective with minimal side effects, and no statistically significant difference was found among the treatment groups. Overall, 82% of patients rated the improvement in their appearance as excellent, with common side effects for fillers being transient redness and swelling, along with bruising [14].
Mesotherapy, beyond filler injection, was explored by Ahmet, Mohammed, and Fatani who conducted vit C mesotherapy for 5 weekly sessions. Comparisons with carboxytherapy and chemical peeling showed no statistically significant differences in pigmentation improvement or patient satisfaction. However, the mesotherapy group reported a higher incidence of a burning sensation post-treatment, despite exhibiting a significant improvement in pigmentation and satisfaction compared to the carboxytherapy group [33].
In a study by Karty et al., autologous fat transfer with emulsified fat injection was found to be superior to PRP in terms of patient satisfaction and POH improvement [19]. Adverse effects were minimal, including bruises and ecchymoses [19].
The final procedure discussed in this part is the conditioned media of stem cells. Employment of stem cells has been expanded in various medical fields during recent years. Bhat et al. used the condition media of human bone marrow mesenchymal stem cells (MSC-CM) to prepare a homogeneous bioactive formulation. This topical solution was applied over periorbital skin area of 20 Indian female participants twice a day for the duration of 12 weeks. It was concluded that this production is nonirritant and significantly effective in reducing the under-eye dark circles, and eye puffiness. The adverse events were not observed in any of the subjects [23].
4.7. Microneedling
In six eligible studies, microneedling was evaluated as the therapeutic option for POH. A study by Yu et al. revealed that daily application of phenylethyl resorcinol under the eye, in conjunction with microneedling twice a week for 8 weeks, significantly enhanced treatment efficacy for POH without any observed side effects [9].
Wu et al. conducted a study treating infraorbital dark circles unilaterally with three sessions of microneedle fractional radiofrequency (MR) at 2-month intervals. The MR settings included a penetration depth of 0.5 mm, fluency level 2, power 12.5 W, and a duration of 50 ms. The procedure demonstrated significant improvement in infraorbital dark circles. However, MI was not meaningfully different between treated and control sides. No side effects were reported, and participants found the treatment tolerable [28].
Comparisons of microneedling efficacy for POH treatment were made with other procedures. Ghandehari et al. conducted a split-face clinical trial comparing three monthly sessions of CO2 fractional laser and microneedling, both combined with topically applied tranexamic acid. Both modalities significantly improved POH (p value < 0.05), with no meaningful differences in patient satisfaction, evaluator assessment, side effects, or tolerability. However, microneedling induced longer-lasting erythema compared to fractional CO2 laser (p value = 0.014) [16].
Carboxytherapy was also compared to microneedling. Assaf et al. demonstrated that six biweekly sessions of carboxytherapy injected four to six puffs of 5 cc gas at the lateral one-third of each eyelid were more efficient than microneedling with 0.25 mL/session glutathione for POH, based on VAS evaluation and dermoscopic assessments of vascular, skin, and pigmentation improvements during treatment (p = 0.001) and follow-up (p = 0.006). Microneedling with topical glutathione caused ecchymosis, while carboxytherapy reported no side effects [15].
4.8. Combination Therapies
It is widely acknowledged that integrating multiple therapeutic approaches in a single session yields more successful outcomes. Several studies have logged the implementation of various combinations such as different lasers, laser combined with PRP, microneedling, and diverse agents for treating POH.
Two studies explored combinations of lasers. In one, the combination of two wavelengths of picosecond Nd: YAG in a single session was compared to three sessions at 3-week intervals using a picosecond 755-nm alexandrite laser. Vanaman Wilson et al. applied Nd:YAG laser with a single pass of 1064 nm at, mmm 1.3 J/cm2 and 5 Hz, immediately followed by a single pass of 532 nm at 0.16 J/cm2 at 5 Hz for a total of 250 pulses for POH treatment. Blinded investigator assessment revealed a significant improvement with the alexandrite laser unlike the combination group [27].
Manuskiatti, Fitzpatrick, and Goldman used QS alexandrite laser with a 3-mm spot size at a fluence of 8.0 J/cm2 following resurfacing CO2 laser for treating brown POH, achieving 75%–100% clearing in all patients within 6 months after treatment. The sign of improvement developed 6–8 weeks after the treatment [30] (treatment of facial skin using combinations of CO2, Q-switched alexandrite, flashlamp-pumped pulsed dye, and Er: YAG lasers in the same treatment session).
PRP was combined with two different lasers. While CO2 laser alone is effective, Behrangi et al. found that adding PRP significantly decreased hyperpigmentation by 25%, accompanied by increased satisfaction from both patients and physicians, and a shorter duration of erythema and swelling (p < 0.001) [17].
Nilforoushzadeh et al. combined PRP in injected and topical forms with fractional long-pulse Er:YAG laser with energy of 500–700 mJ in three monthly sessions for periorbital dark circles, leading to a significant decrease in melanin content and improved subjective and objective outcomes (p < 0.05) [4].
Koundias, Kastora, and Rajpara combined fillers with lasers, comparing the efficacy of two filler sessions 2 weeks apart with three laser sessions every 6 weeks in India and the United Kingdom. All three approaches proved effective in treating POH, with no significant differences among them. Tear trough and hollow eyes responded well to fillers, Q-switched Nd:YAG laser was preferred for pigmented POH, long-pulsed Nd: YAG laser for vascular type, and fractional CO2 for loose skin and wrinkles [14].
Microneedling combined with various agents, including peeling, tranexamic acid, and glutathione, was explored. Adding 10% TCA cream to microneedling showed no superiority over fractional CO2 laser, with the combination group reporting no serious complications, while the laser group experienced erythema and pain [12].
Paradoxically, Kontochistopoulos et al. conducted four biweekly sessions of under-eye microneedling following a five-minute application of 10% TCA solution, yielding promising esthetic results with no recurrence after 4 months, albeit with mild discomfort and transient erythema as reported side effects [10]. Both studies included patients with Skin Types II–IV.
In a split-face, controlled pilot clinical trial, six biweekly sessions of microneedling following topical glutathione (0.25 mL/session) were compared to carboxytherapy. This combination proved less effective than carboxytherapy and resulted in more complications [15].
4.9. Limitations and Suggestions
The primary limitation of this study is the absence of uniform objective measurements across the included studies for assessing postoperative POH. This inconsistency impeded the inclusion of some relevant studies in our quantitative synthesis, possibly impacting the overall findings. Specifically, only two studies employed reliable objective measurement tools, such as the Mexameter, to assess POH severity. The Mexameter is a device that quantitatively measures skin pigmentation and erythema by assessing melanin and hemoglobin levels, providing a more standardized and reproducible assessment of pigmentation. However, due to the limited number of studies utilizing this method, these data could not be included in the meta-analysis. Despite concerted efforts, the persisting high heterogeneity among studies poses challenges to the generalizability and robustness of our results. For future research, it is crucial to adopt more objective assessment methods, such as established POH scoring systems, Mexameter measurements, and computer-assisted visual evaluations of pigmentation and wrinkles, to ensure methodological uniformity and enhance the comparability of results.
Additionally, conducting studies with larger sample sizes, employing split-face designs, and increasing follow-up duration are imperative to strengthen the validity of the findings and to better represent the diverse patient population affected by POH. It is important to note that the studies included in this review had follow-up periods of less than 6 months, which limits our ability to assess the long-term sustainability and safety of the treatment effects. To address this gap, future research should prioritize extended follow-up durations to verify the durability of treatment outcomes and monitor potential long-term adverse events. This approach will help provide a more comprehensive evaluation of the treatments’ effectiveness over time.
The etiology of POH plays a crucial role in selecting the most suitable treatment modality. Given that POH often results from a combination of different underlying factors—such as vascular, pigmented, and structural causes—it is essential to tailor treatments accordingly. For instance, vascular POH may respond best to laser therapies targeting blood vessels, while pigmented POH might benefit from chemical peels and topical agents, such as mesotherapy solutions, that reduce melanin [38]. However, in the majority of studies included in this review, the exact etiology of POH could not be clearly extracted from the patients, complicating efforts to attain treatment efficacy based on etiologic factors. Because multiple etiologies frequently contribute to POH in a single patient, combination therapies, including the use of lasers, chemical peels, and mesotherapy, are often necessary to achieve optimal results, addressing each contributing factor simultaneously.
It is important to recognize the absence of a formal cost-effectiveness analysis. Cost-effectiveness is a crucial factor in clinical decision-making. For instance, while fillers and autologous fat grafting are could be potentially effective for structural POH, they are also among the most expensive treatments with potential for repeat sessions, making them less cost-effective compared to topical treatments or chemical peels, which offer a more affordable option albeit with comparable efficacy. Future studies should incorporate cost-effectiveness analyses to guide clinicians and patients in making more informed, value-based decisions when selecting treatment options.
5. Conclusion
In conclusion, this systematic review provides a comprehensive overview of the efficacy, patient satisfaction, and adverse events associated with various treatment modalities for POH including lasers and light therapies, chemical Peels, carboxytherapy, PRP, microneedling, autologous fat transfer, fillers, and combination treatments. According to the meta-analysis, filler treatments exhibited the highest rate of excellent improvement, though these results, derived from a single study, warrant cautious interpretation. Laser and combination treatments also demonstrated substantial effectiveness, especially in achieving excellent outcomes, while autologous fat transfer and chemical peels showed notable efficacy. PRP treatments, although not achieving high rates in the excellent category, were prominent in the good improvement category.
Regarding patient satisfaction, combination treatments were most favorable, with a significant proportion of patients reporting excellent satisfaction. Laser treatments, despite their notable good satisfaction rates, showed elevated poor satisfaction rates, highlighting the need for further investigation. Chemical peel and PRP treatments presented limited patient satisfaction.
Adverse events across these treatments were generally mild, tolerable, and transient. Common side effects included a transient burning sensation and erythema for lasers, discomfort, and local pain for CO2 laser treatments and contact dermatitis for Er: YAG laser treatments. Notably, the combination of PRP and CO2 laser significantly reduced the duration of swelling and erythema compared to CO2 laser alone.
Overall, these findings underscore the importance of individualized treatment approaches, considering patient needs, expectations, and specific etiological factors of POH. Future research with an increased follow-up period implementing multiple treatment arms should aim to enhance these findings with larger, multistudy analyses to ensure broader applicability and understanding of the efficacy and safety profile of the various modalities in the treatment of POH.
Conflicts of Interest
The authors declare no conflicts of interest.
Funding
No funding was received for conducting this study.
Acknowledgments
The authors would like to thank Rasool Akram Medical Complex Clinical Research Development Center (RCRDC), especially Mrs Farahnaz Nikkhah for their technical and editorial assistance.
Open Research
Data Availability Statement
The data for meta-analysis are available from the corresponding author upon a reasonable request.




