Prevalence of Human Intestinal Parasitic Infections and Associated Risk Factors among School Children in Hakim District, Harari Regional State, Eastern Ethiopia
Abstract
Background. The goal of this study was to determine the prevalence of intestinal parasitic infections and associated risk factors in the Hakim district of Harari Regional state, Eastern Ethiopia. This region is known for its high incidence of intestinal parasitic infections among socioeconomically disadvantaged communities in the tropics and subtropics. Materials and Methods. A cross-sectional study was carried out in a school setting from September 2021 to May 2022. The study involved 333 participants, including 158 males and 175 females, who were selected using a stratified systematic random sampling method. The stool samples were analyzed using both direct wet mount and formal ether concentration techniques, which were examined microscopically. A structured questionnaire was used to gather information on potential risk factors, and the data were analyzed using SPSS version 20. The P-value < 0.05 was considered statistically significant. Results. Out of 333 students screened, 96 (28.8%) tested positive for one or more intestinal parasites. The highest infection rate was recorded for G. lamblia at 28 (8.8%), followed by E. histolytica at 27 (8.1%). The overall prevalence of parasitic infections was 55 (16.5%). The lowest helminth infection rates were found for A. lumbricoides at 13 (3.9%), hookworm at 11 (3.3%), and T. trichiura at 10 (3%). The most significant risk factors associated with a high risk of Intestinal Parasitic Infections (IPIs) were sex, family size, latrine availability, defecation habit, frequency of hand washing, regular latrine cleaning habit, water source, and knowledge (P < 0.05). However, there was no correlation between IPI prevalence and age, latrine type, or hand washing facility. Conclusion. Based on the research, it was found that IPIs are commonly seen among elementary school children in the Hakim district. To address this issue, it is recommended that the study area implement intensive healthcare interventions, trainings, and mass treatments for the treatment of IPIs.
1. Introduction
In tropical and subtropical regions of the world, intestinal parasite infections (IPIs) are common and endemic in socioeconomically disadvantaged populations [1]. IPIs have a severe negative influence on an infant’s nutritional status, growth, cognitive abilities, and aptitude for learning, making them some of the most important public health issues [2]. The prevalence of intestinal parasites in a given nation is influenced by environmental, social, and demographic factors, such as the population’s health-related behavior and availability to clean water and sanitary latrines [2, 3].
Significant morbidity and mortality rates are caused by intestinal parasites, particularly in underdeveloped nations [4, 5]. Nonetheless, socioeconomic issues and limited access to healthcare services are associated with a higher prevalence of them. In addition to resulting in death and illness, intestinal parasite infection has been linked to undernourishment, reduced linear growth, cognitive function, linguistic proficiency, physical debility, and poor academic performance in school-age children [6]. Geographical and socioeconomic factors that affect the distribution of parasitic infections include climate, poverty, hunger, hygienic practices, population density, lack of access to drinking water, and unsanitary facilities [7]. These lead to hundreds of thousands of preventable deaths annually and are among the most prevalent infectious diseases in the world. In the tropics, the infections are more common, particularly in underprivileged areas and researches show that helminthiasis is on the rise in such areas [8, 9].
The capital of the Harari region is Harar, located on a mountaintop in the eastern region of the nation. The town is overpopulated and has a shortage of potable water [10]. The city’s population projection is expected to be 183,415 people living in 311.25 km2 of land [11]. As demonstrated by earlier researches carried out in several Ethiopian regions [12, 13, 14, 15], school children are extremely susceptible to intestinal parasite infections. There are numerous research conducted in various locations of Ethiopia; however, there is a lack of published information about intestinal parasite infections in Harar Town. Thus, the purpose of this research is to ascertain the frequency of intestinal parasite infections and related risk factors in school-age children in Hakim district, Harari regional state of Eastern Ethiopia.
2. Materials and Methods
2.1. Study Area
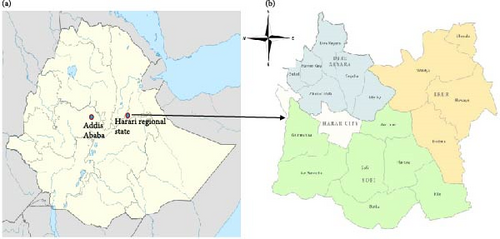
The study was conducted in Harar town, Hakim district (Figure 1), which is one of the nine districts in Harari region, Eastern Ethiopia. The town is located 526 km east of the capital city of Ethiopia, Addis Ababa. It is located between 9°11"49′N, 9°24”42′N latitude, 42°3”30′E, and 42°16"24′E longitude and the elevation ranges from 1,300 to 2,200 m above sea level. Based on the 2007 census conducted by Central Statistical Agency of Ethiopia [11], the town had a total population of 183,415 of whom 92,316 were men and 91,099 were women. Out of which, 54.18% of the population dwell in urban with an estimated area of 311.25 km2 and the rest is rural. This region estimated density of 589.05 per square kilometer.
2.2. Study Design and Period
A school-based cross-sectional study was conducted between September 2021 to May 2022 in three selected primary schools of Hakim District, Harar town.
2.3. Inclusion and Exclusion Criteria
All children enrolled in grades 1 through 8 from the selected schools, between the ages of 5 and 12, whose parents provided permission to be included in the study, were included. All children who were very sick at the time of the survey and whose parents did not offer to give consent were omitted.
2.4. Study Population
The study population was all school children enrolled in three governmental primary schools (Qundudo, Nugus-Shira, and Ganda Gobe) in Hakim district, who were attending grades 1–8 in the 2021–2022 academic year. The three schools were purposively selected due to their location in the town and proximity for data collection and among the total of 333 selected students 158 were males and 175 were females.
2.5. Sampling and Sample Size Determination
In Qundudo, Nugus-Shira, and Ganda Gobe primary schools, the total enrolled student population for the 2021/2022 academic year was 1,250 (600 males and 650 females), 946 (360 males and 586 females), and 836 (412 males and 424 females), respectively. Since no prior research of this kind had been done in the area, it was assumed that IPIs were substantially more common among kids in the schools, and a 50% prevalence rate was used. Next, using a statistical formula (n = z2p(1−p)/d2) as detailed in [5], the sample size for a single population was determined based on the 95% confidence limits and 5% sampling error, where n = sample size, d = precision, p = expected prevalence or proportion, z = statistic for a level of confidence. Since the target population was less than 10,000 (N = 2,004, used as a sample frame), 333 was the total population that was determined using the corrected formula (n/1 + n/N). Proportionate stratification based on student size was used to choose study participants from each school. As a result, a systematic random sampling procedure was used to choose the actual number of study participants from each institution.
2.6. Questionnaire Survey
A pretested, structured questionnaire written in English and translated into the local languages was used to collect data on the sociodemographic traits of the research respondents as well as risk factors that put school children at risk for parasite infections.
2.7. Data Collection Procedure and Specimen Examination
Stool samples were collected in accordance with standard procedure as per WHO [16]. A field worker verified that all specimens had the correct label, quantity, time, and procedure of collection (along with appropriate hygienic and biosafety measures) before transferring them to the regional laboratory and Harari Health Research for microscopic and gross stool examinations. In the lab, slides were prepared for wet mount directly in saline and iodine solutions, and they were subsequently inspected under a microscope.
2.8. Data Analysis
SPSS version 20 was utilized for data analysis after the data were coded and saved in Microsoft Excel. The relationship between each risk factor and IPIs was evaluated using univariate logistic regression analysis. The adjusted odds ratio with a 95% confidence interval was used in multiple logistic regression analysis to identify the independent risk variables for infection. P values less than 0.05 indicated that the association’s finding was statistically significant.
2.9. Ethical Considerations
Before the start of the investigation, ethical approval was granted by the Dire-Dawa University Ethics Committee. In order to prevent any confusion in their minds, explanations were provided to study participants and other relevant parties. Additionally, consent was acquired from the parents and/or guardians of the children.
3. Results
3.1. Sociodemographic Characteristics
The study comprised 333 students from three elementary schools, 158 of whom were male (47.44%) and 175 of whom were female (52.55%). In total, 160.4% of them attended Qundudo Primary School, 14.71% attended Ganda Gobe Primary School, and 37.23% attended Nigus Shira Primary School. In terms of age group, 238 (71.74%) of the participants were older than 13 years, while 95 (28.52%) were between the ages of 5 and 12. Out of the three schools, 70.57% of the students said that they knew nothing about intestinal parasite illnesses before, and only 29.42 said they did (Table 1).
| Variable | Attribute | Number | Percentage | |
|---|---|---|---|---|
| Sex | Male | 158 | 47.44 | |
| Female | 175 | 52.55 | ||
| Age (years) | 5–12 | 95 | 28.52 | |
| 13–17 | 238 | 71.74 | ||
| School and sex | NugusShira | Male | 59 | 47.58 |
| Female | 65 | 52.41 | ||
| GandaGobe | Male | 34 | 69.38 | |
| Female | 15 | 30.61 | ||
| Qundudo | Male | 65 | 40.62 | |
| Female | 95 | 59.37 | ||
| Water source | Unprotected | 100 | 30.03 | |
| Protected | 233 | 69.96 | ||
| IPI knowledge | Yes | 98 | 29.42 | |
| No | 235 | 70.57 | ||
3.2. Overall Prevalence
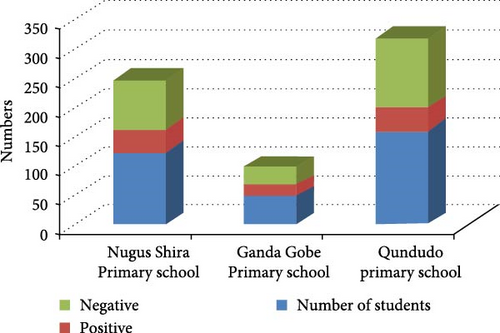
The overall prevalence of intestinal parasitic infections (IPIs) was found to be 28.8% of which 16.21% were males while 12.61% were females (Figure 2).The highest infection rate (34.69%) was recorded at Ganda Gobe Primary School followed by Nigus Shira Primary School (30.6%) and Qundudo Primary School (25.6%).
3.3. Risk Factors Associated with Intestinal Parasitic Infections
Chi-square (χ2) test analysis of the risk factors showed a significant associations between the prevalence of IPIs and the risk factors including participants sex (χ2 = 4.196, P = 0.035) with OR = 1.6, family size (χ2 = 7.7248, P ≤ 0.001) with OR = 7.72, latrine availability (χ2 = 4.1,P = 0.038) with OR = 4.1, defecation habits (χ2 = 12.47, P = 0.006) with OR = 12.47, hand washing habit (χ2 = 9.75, P = 0.008) with OR = 9.75, latrine cleaning habit (χ2 = 30.9, P ≤ 0.001) with OR = 30.91, and water source (χ2 = 44.55, P ≤ 0.001) with OR = 60.96. However, prevalence of IPIs was not associated with age groups, types of latrine, and hand washing facility (P > 0.05) (Table 2).
| Risk factor | Variable | Number of respondents (%) | IPI +ve (%) | IPI −ve (%) | OR | χ2 | P-value |
|---|---|---|---|---|---|---|---|
| Sex | Male | 158 (47.44) | 54 (16.21) | 104 (31.2) | 1.64 | 4.20 | 0.035 ∗ |
| Female | 175 (52.55) | 42 (12.61) | 133 (39.9) | ||||
| Age | ≤9 | 95 (28.52) | 34 (10.21) | 61 (18.31) | 1.58 | 3.15 | 0.072 |
| ≥10 | 238 (71.74) | 62 (18.61) | 176 (52.8) | ||||
| Family size | ≥6 | 192 (57.65) | 44 (13.21) | 148 (44.4) | 0.50 | 7.72 | 0.00 ∗ |
| ≤5 | 141 (42.34) | 52 (15.61) | 89 (26.72) | ||||
| Latrine availability | No | 263 (78.97) | 69 (20.72) | 194 (58.2) | 0.56 | 4.10 | 0.038 ∗ |
| Yes | 70 (21.02) | 27 (8.10) | 43 (12.91) | ||||
| Defecation habit/no latrine | In-pit | 33 (47.14) | 22 (6.60) | 11 (3.30) | — | 12.47 | 0.006 ∗ |
| Near the stream/dish | 7 (10) | 4 (1.20) | 3 (0.909) | — | |||
| In the field | 30 (42.85) | 17 (5.10) | 13 (3.90) | — | |||
| Bucket | 25 (9.50) | 20 (6.00) | 5 (1.50) | — | |||
| Type latrine | Tr/pit latrine | 109 (41.44) | 35 (10.51) | 74 (22.22) | — | 0.81 | 0.666 |
| Flush toilet | 89 (33.84) | 33 (9.90) | 56 (16.81) | — | |||
| Open defecation | 40 (15.20) | 28 (8.40) | 12 (3.60) | — | |||
| Hand washing facility | Yes | 99 (37.64) | 35 (10.51) | 64 (19.21) | 0.92 | 0.09 | 0.763 |
| No | 164 (62.37) | 61 (18.31) | 103 (30.93) | ||||
| Frequent hand washing habit | Yes | 16 (16.16) | 15 (4.50) | 1 (0.30) | — | 9.75 | 0.008 ∗ |
| Sometimes | 23 (23.23) | 21 (6.30) | 2 (0.60) | — | |||
| No | 60 (60.60) | 36 (10.81) | 24 (7.0) | — | |||
| Regular latrine cleaning habit | Always | 47 (17.87) | 6 (1.80) | 41 (12.31) | — | 30.91 | 0.00 ∗ |
| Once per week | 91 (34.60) | 28 (8.40) | 63 (18.91) | — | |||
| Twice per week | 42 (15.96) | 14 (4.20) | 28 (8.40) | — | |||
| Not at all | 84 (31.93) | 40 (12.01) | 44 (13.21) | — | |||
| Water source | Unprotected | 100 (30.03) | 54 (16.21) | 46 (13.81) | — | 60.96 | 0.005 ∗ |
| Protected | 233 (69.96) | 31 (9.30) | 202 (60.66) | — | |||
| IPI knowledge | Yes | 98 (29.42) | 37 (11.11) | 61 (13.31) | 1.80 | 5.39 | 0.015 ∗ |
| No | 235 (70.57) | 59 (17.71) | 176 (52.8) |
- ∗ and bold value shows statistically significant values.
3.4. Major Intestinal Parasites
As shown in Table 3, out of the infecting parasites, protozoan infection (G. lamblia and E. histolytica) showed the highest prevalence of 14 (50%) in Nigus Shira, 10 (66.66%) in Ganda Gobe, and 31 (58.49%) in Qundudo primary schools, respectively, followed by Helminth infection (A. lumbricoide, T. trichiura, and Hookworms) and double infections.
| School | Parasite (type and species) | Number | Frequency total (%) | ||
|---|---|---|---|---|---|
| Male | Female | ||||
| Nigus Shira Primary School | Protozoan | G. lamblia | 2 | 5 | 7 (25) |
| E. histolytica | 3 | 4 | 7 (25) | ||
| Helminth | A. lumbricoide | 2 | 2 | 4 (14.28) | |
| T. trichiura | 1 | 3 | 4 (14.28) | ||
| Hookworms | 1 | 2 | 3 (10.71) | ||
| Double infections | A. lumbricoide and E. histolytica | 2 | 1 | 3 (10.71) | |
| Total | 11 | 17 | 28 (100) | ||
| Ganda Gobe Primary School | Protozoan | G. lamblia | 2 | 3 | 5 (33.33) |
| E. histolytica | 3 | 2 | 5 (33.33) | ||
| Helminth | A. lumbricoide | 1 | — | 1 (6.66) | |
| T. trichiura | 2 | — | 2 (13.33) | ||
| Hookworms | 2 | — | 2 (13.33) | ||
| Total | 10 | 5 | 15 (100) | ||
| Qundudo Primary ScHool | Protozoan | G. lamblia | 12 | 4 | 16 (30.19) |
| E. histolytica | 10 | 5 | 15 (28.30) | ||
| Helminth | A. lumbricoide | 5 | 3 | 8 (15.09) | |
| T. trichiura | 3 | 1 | 4 (7.5) | ||
| Hookworms | 2 | 4 | 6 (11.32) | ||
| Double infections | E. histolytica and Hookworms | 2 | 2 | 4 (7.5) | |
| Total | 34 | 19 | 53 (100) | ||
4. Discussion
The study showed an overall prevalence of 28.82% which is lower than previous studies conducted in various parts of Ethiopia [14, 17, 18]. On the other hand, the study was shown to be higher than a study conducted in Hawasa (26.6%) [19]. But, slightly comparable with a study conducted in Arba Minch (Southern Ethiopia) (27.7%) [20]. These variations could be due to health facility statuses in the regions, water sanitation level, endemicity, geographical condition, population density, methods employed for stool examination, cultural differences, and others. The higher prevalence in males (16.21%) than females (12.61%) of the present study is in agreement with studies in Merawi town (Northwestern Ethiopia) [21], Delgi [22], and Yemen [18]. The higher incidence in males may be due to the fact that men engage in more field activities such as farming, fetching water, and swimming in unprotected pools on more frequent than the female counterparts, making them more susceptible to parasite infections.
Age group was also considered to be a potential risk factor for IPIs. Thus, the study showed a higher prevalence rate of IPIs (18.61%) in students between 13 and 17 years than those between 5 and 12 years (10.21%). Similar results were also found by Tandukar et al. [23] who studied in school children of Lalitpur district and Shrestha et al. [24] who studied in schoolchildren in Dolakha and Ramechhap districts of Nepal. Children at this age group are more likely to participate in outdoor activities and consume fast foods from the market, which could be a major risk factor for IPIs. In addition, out of the infected students above 13 years of age category, 11.11% were males and 7.50% were females. The reason for higher prevalence might be due to a more exposure of male students with the risk factors due to their playing habits than females.
In the study, a higher degree of association (P < 0.005) of the prevalence of IPIs and risk factors such as family size where the family size is more than six is highly associated with IPIs, latrine availability where students without latrine facilities are more vulnerable than those that use latrine, frequent hand washing habit where students with nonfrequent hand washing habit are more infected, latrine cleaning habit. The present study indicated a high amount of possible fecal contamination, indicating the urgent need for efficient management of the provision of safe drinking water promptly and effectively. A higher prevalence (16.21%) of IPIs was observed in children who drink water from unprotected water sources. A similar result was also reported by Gupta et al. [25] in school children of Saptari district, Nepal. Harari regional state is also known for its problem with availability of safe and clean drinking water [15].
In this study, the most common protozoan infection was found to be G. lambilia with a prevalence rate of 8% which is in agreement with a study in primary school of Southwest Ethiopia (8.1%) [26] and lower than reports in Dona Berber Primary School, Bahirdar (24.5%) [27], among school children in White Nile state, Sudan (31.2%) [28] and Rwanda (25.95%) [29]. Though it is slightly greater than studies among Jawi primary school children, Jawi town, Ethiopia (5.9%) [30], among primary school children in Birbir town, Southern Ethiopia (2.6%) [13], and among school children in Taif, Western Saudi Arabia (2%) [31]. The variations in the prevalence rates may be related to variations in school and environmental sanitation in different environmental settings.
The study also showed the highly prevalent soil-transmitted Helminth parasite A. Lumbricoides with a prevalence rate of 3.9% which is less than studies among primary school children in Gurage Zone, Ethiopia (9.4%) [12], among school children at Sekela Primary School, Western Ethiopia (9.86%) [32], among mentally disabled and nondisabled primary school students, Bahir Dar, Ethiopia (13.6%) [33], among rural school children Birbir town, Southern Ethiopia (8.8%) [13], among the first-cycle primary school children in Sasiga District, Southwest Ethiopia (22.7%) [26]. However, it is greater than Delo-Mena district, Ethiopia (3.7%) [34], Glomekeda district, Northern Ethiopia (3.3%) [35]. Improved sanitation, health education, and morbidity management through deworming could be some potential causes for the decline in the prevalence of STH infections.
5. Conclusions
From the present study, it was concluded that there is a higher prevalence of IPI in the selected schools causing a tremendous public health threat. It was also seen a higher infection rate for G. lamblia followed by E. histolytica. The prevalence of IPIs were highly associated with common risk factors such as sex, family size, latrine availability, defecation habit, frequency of hand washing, regular latrine cleaning habit, water source, and knowledge.
From the study, it was recommended that a community-based health education, mass treatment, and school-based deworming without interruption should be considered. It is also critically necessary to expand the infrastructures to provide access to safe drinking water for all of the residences in Hakim district.
Additional Points
Study Limitations. This research has been limited to primarily being conducted among students in the Hakim District of the Harari regional state. It would have been preferable to include students from outside the town to acquire a more complete picture of the incidence of IPIs and the associated usual and common risk factors. Second, the prevalence of IPIs may have been understated due to the use of a single fecal sampling approach. Third, a more sensitive diagnostic technique that could distinguish the morphologically identical separate IPIs was not used in the study. Finally, the study does not use methods for detection of coccidian parasites (e.g., Cryptosporidium, Isospora, and Cyclospora) and microsporidia.
Disclosure
The funder did not allocate budget for publication.
Conflicts of Interest
The authors declare that they have no conflicts of interest.
Acknowledgments
The authors acknowledge Harari Health Bureau for providing laboratory facilities during sample collection and testing. This piece of work was supported by the Ministry of Education (Ethiopia).
Open Research
Data Availability
The data that support the findings of this study are available upon request from the corresponding author.




