Factors Influencing Insulin Adherence among Outpatients with Type 2 Diabetes Mellitus and the Impact of Pharmaceutical Intervention: A Randomized Clinical Trial
Abstract
Aims. This study aimed to identify and analyze the factors significantly influencing long-term insulin medication adherence among outpatients and to evaluate whether pharmaceutical interventions targeting these factors can improve patient medication adherence and glycemic control. Methods. A cohort of 180 patients was recruited from a tertiary hospital in Nanjing, China. Factors potentially influencing insulin adherence were scrutinized employing the KAP (knowledge, attitude/belief, and practice) health behavior model. Baseline characteristics were extracted from the hospital information system, while patient knowledge of the disease and medication, medication adherence, medication beliefs, and management self-efficacy were assessed, respectively, using self-developed questionnaires, MMAS-8, C-DMSES, and BMQ scales. Univariate and multivariate analyses were conducted to determine the impact of these factors on insulin adherence. Following this, participants were randomly allocated to either the intervention or control group. The intervention group received three months of weekly telephone sessions and educational interventions targeting facets such as medication knowledge and beliefs, while the control group received standard care. After the intervention, insulin adherence and glycemic control conditions of both groups were collected and re-evaluated. Results. After excluding lost-to-follow-up patients, 152 individuals were analyzed (intervention: 75 and control: 77). Multivariate analyses revealed factors influencing insulin adherence, including age, diabetes duration, health insurance status, HbA1c level, disease and medication knowledge, diabetes management self-efficacy, and medication beliefs (P < 0.05). Before targeted pharmaceutical care, no significant differences existed in insulin adherence, HbA1c levels, management self-efficacy, knowledge, or medication beliefs between intervention and control groups (P > 0.05). However, subsequent pharmaceutical intervention notably improved adherence, HbA1c levels, self-efficacy, knowledge, and medication beliefs (P < 0.05). Conclusion. This study examines the impact of glycemic control, health insurance status, management self-efficacy, level of knowledge, and medication beliefs on improving insulin medication adherence in patients with type 2 diabetes mellitus. Targeted pharmaceutical intervention can enhance medication adherence, improve glucose control, and promote rational insulin use. This trial is registered with ChiCTR2300074444.
1. Introduction
In recent years, the incidence of diabetes has markedly increased in China, from 0.67% in 1980 to 11.2% in 2017, with type 2 diabetes (T2DM) accounting for over 90% of cases [1, 2]. As diabetes progresses, patients’ pancreatic β-cell function gradually declines, prompting the significance of insulin therapy for glycemic management [3–6]. It is estimated that approximately one-third of Chinese diabetes patients receive insulin therapy for glycemic control [7].
The optimal insulin treatment regimen offers potential reductions in the risks associated with diabetes complications, healthcare costs, and mortality rates. However, achieving these benefits necessitates patients maintaining a high level of adherence [8], wherein the timing and dosage of insulin administration align with recommendations from healthcare professionals. Despite this, global survey data suggest a widespread lack of adherence to insulin therapy among T2DM patients [9, 10]. A meta-analysis encompassing 57 studies, and 125,241 patients revealed that the average adherence to insulin among individuals with T2DM stood at a mere 52.55% (95% CI: 43.08%–62.01%) [9].
Prior research has underscored the association between insulin adherence and various factors. These encompass aspects related to both medication and disease, such as insulin cost, injection apprehension, discomfort at injection sites, weight changes, and the potential for hypoglycemia [11, 12]. Moreover, individual traits, including patient age and regional, geographic, and ethnic disparities, may also exert an influence on medication adherence [13].
Several studies have implemented ongoing educational interventions for discharged patients with the aim of improving medication adherence and glycemic control [14–20]. For example, Ranjbaran et al. [14] conducted a dietary and medication education program among 124 Iranian T2DM patients using the health action process approach (HAPA). Following a six-month period, noteworthy enhancements were observed in patients’ adherence to dietary and medication regimens, as well as in their intention and self-efficacy. On the other hand, Simon et al. [15] demonstrated that pharmacist-led counseling interventions enhance patient compliance, quality of life, and satisfaction with care among diabetic patients in India. Similar outcomes have been reported in studies conducted in Brazil [16]. Nevertheless, in the context of China, there remains insufficient evidence to support the effectiveness of such outpatient educational interventions. Given potential disparities in socioeconomic conditions and healthcare resource allocation, the factors influencing patient insulin adherence may differ from those observed in other countries or regions. Consequently, there is a pressing need for a comprehensive analysis of these obstacles and the implementation of targeted educational interventions.
The knowledge, attitude/belief, and practice (KAP) model serves as a conceptual framework for understanding how individual knowledge and beliefs shape health behavior, with widespread application in diabetes intervention research [21, 22]. According to this model, understanding of the disease and medication forms the cornerstone of behavior modification, while patients’ beliefs and attitudes act as internal drivers for behavioral change. Together, knowledge and beliefs exert a collective influence on health behavior, ultimately impacting health outcomes. In this study, the theoretical framework of KAP (depicted in Figure 1) is utilized to assess the influence of medication knowledge, medication beliefs, and other potential factors on insulin adherence. Subsequently, targeted medication education interventions are implemented to address these influencing factors. The primary objective is to bolster patient knowledge and reinforce their beliefs about medication. Ultimately, the aim is to facilitate the rational utilization of insulin and improve glycemic control.

2. Material and Methods
2.1. Study Design and Participants
This was a 3-month, single-center, open-labeled, randomized clinical trial conducted between 2022 and 2023 at Nanjing Drum Tower Hospital, Affiliated Hospital of Medical School, Nanjing University, Nanjing, China. The study protocol received approval from the hospital’s Medical Ethics Committee (grant no. 2020-233-02) and has been publicly registered in the Chinese Clinical Trial Registry (ChiCTR) (registration no. ChiCTR2300074444). The trial rigorously followed ethical principles outlined in the Declaration of Helsinki to ensure comprehensive protection of participants’ safety, rights, and confidentiality throughout the entire study duration.
Patients meeting the following inclusion criteria were recruited: (1) diagnosed with T2DM according to 2020 Chinese Diabetes Society Guidelines [1], (2) aged between 18 and 70 years with clear consciousness and the ability to independently respond to questions, (3) received insulin therapy for over 3 months, and (4) signed informed consent and were willing to participate in follow-up. Exclusion criteria included those who (1) were unable to complete follow-ups on time or were lost to follow-up, (2) discontinued insulin therapy, or (3) declined pharmaceutical interventions.
2.2. Study Protocol
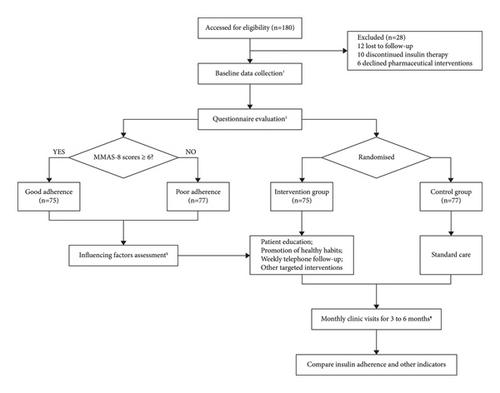
All participants underwent a rigorous screening process based on the aforementioned criteria. Baseline characteristics and glycemic control data were collected and organized through the hospital information system on the hospital intranet. Subsequently, a series of questionnaires were administered to assess insulin adherence and relevant factors, such as disease and medication knowledge, management self-efficacy, and medication beliefs. These measurement scales have been validated for good reliability and validity in previous research [23–30]. Following the questionnaire assessment, participants were randomly assigned to either the intervention or control group using the random number table method. The intervention group received weekly follow-up visits and pharmaceutical interventions targeted at the identified influencing factors for three months, while in the control group, standard care was adopted. Patients in both groups attend monthly clinic visits to collect their glycemic control data. If glucose levels remained normal for three consecutive months, both the control and intervention groups concluded the trial prematurely. Conversely, if a patient’s glucose indices persisted as abnormal or failed to normalize, the trial was extended for up to 6 months. Participants received a minimum of 12 pharmaceutical interventions within the initial 3 months and a maximum of 24 interventions within 6 months. After follow-up, questionnaires were administered to all participants again to compare medication compliance and other indicators between the two groups both before and after the intervention. The flowchart of the trial protocol can be found in Figure 2.
2.2.1. Baseline Characteristics
The basic information of patients was collected and organized through the hospital information system on the hospital intranet, which included patient general data (age, sex, educational level, marital status, payment methods, and body mass index [BMI]), as well as disease and medication data, including diabetes condition (blood glucose, glycated hemoglobin [HbA1c], fasting C-peptide, 2-hour postprandial C-peptide, diabetes duration, and insulin adverse reactions), liver and kidney function (serum creatinine [Cr], blood urea nitrogen [BUN], aspartate aminotransferase [AST], and alanine aminotransferase [ALT]), and other indicators (low-density lipoprotein cholesterol [LDL-C], diastolic blood pressure [DBP], and systolic blood pressure [SBP]). Presently, the HbA1c level stands as the gold standard for assessing diabetes management effectiveness. For global T2DM cases, a commonly embraced threshold is HbA1c < 7.0% (53 mmol/mol), indicative of favorable glycemic control [1, 4, 5]. Thus, in this study, the participants with HbA1c < 7.0% were categorized as achieving stable disease control, whereas those with HbA1c ≥ 7.0% were classified as achieving poor glycemic control.
2.2.2. Evaluation of Insulin Adherence
The 8-item Morisky Medication Adherence Scale (MMAS-8) questionnaire was used to assess insulin adherence among patients [24–26]. The details of the questionnaire are shown in Table 1. Each of the 8 items in the MMAS-8 was assigned 1 point, resulting in a total score of 8 points. The options for items 1–4, 6, and 7 were “yes” and “no,” with 1 point given for “no” and 0 points for “yes;” the options for item 5 were also “yes” and “no,” with 1 point given for “yes” and 0 points for “no;” the Linker 5 scoring method was applied in item 8, with the options set as “never,” “occasionally,” “sometimes,” “often,” and “always,” with “never” scored as 1 point and the subsequent options scored in 0.25-point decrements. The final score of ≥6 indicated good adherence, while the score of <6 demonstrated poor adherence [24]. Furthermore, the changes in medication adherence of patients at enrollment and after follow-up were also recorded.
| Items | Option (score) |
|---|---|
| (1) Do you sometimes forget to inject insulin? | Yes (0) |
| No (1) | |
| (2) Over the past two weeks, were there any days when you did not inject insulin? | Yes (0) |
| No (1) | |
| (3) Have you ever cut back or stopped administration without telling your doctor because you felt worse when you took it? | Yes (0) |
| No (1) | |
| (4) When you travel or leave home, do you sometimes forget to bring along your insulin? | Yes (0) |
| No (1) | |
| (5) Did you inject insulin yesterday? | Yes (0) |
| No (1) | |
| (6) When you feel like your diabetes is under control, do you sometimes stop taking your medicine? | Yes (0) |
| No (1) | |
| (7) Injecting insulin every day is a real inconvenience for some people. Do you ever feel hassled about sticking to your diabetes treatment plan? | Yes (0) |
| No (1) | |
| (8) How often do you have difficulty remembering to inject insulin? | Never (1) |
| Almost never (0.75) | |
| Sometimes (0.5) | |
| Quite often (0.25) | |
| Always (0) | |
- The objective of this scale is to evaluate the adherence of patients with type 2 diabetes to insulin treatment plans. The scale comprises eight items, contributing to a cumulative score of eight points. Patients selected responses to each question based on their individual situations. Researchers computed the sum of scores indicated within the parentheses beside the answers. A final score of ≥6 signifies satisfactory adherence, while a score of <6 signifies inadequate adherence. The MMAS-8 Scale (TX0008632533), content, name, and trademarks are protected by US copyright and trademark laws. Permission for use of the scale and its coding is required. A license agreement is available from MMAR, LLC., https://www.moriskyscale.com. (©2007 Donald E. Morisky).
2.2.3. Patient Knowledge of the Disease and Medication
Based on the results of the literature review and consultations with endocrinology experts, we designed a knowledge questionnaire concerning T2DM and insulin usage, which consisted of 15 questions and covered various aspects, including glycemic control targets, diabetes complications, indications for insulin use, mechanism of action, injection timing and techniques, adverse drug reactions, and the importance of follow-up. Each question was assigned one point for a correct answer, with a total score of 15 points. Higher scores indicate greater knowledge and understanding. We conducted a pilot test among 50 T2DM patients hospitalized in our endocrinology department, followed by a remote retest administered two weeks after their discharge. The overall Cronbach’s α coefficient was 0.823, while the test-retest reliability stood at 0.797. Furthermore, the overall content validity index was 0.845. Therefore, our questionnaire demonstrates robust reliability and validity, serving as an effective tool for evaluating patients’ comprehension of the disease and insulin usage.
2.2.4. Medication Beliefs
The Chinese version of the Beliefs about Medication Questionnaire (BMQ)-specific scale was applied [27, 28]. There were 2 dimensions in the scale, each with 5 independent items. One dimension measured patient demands for insulin administration, while the other measured patient concerns about insulin-related adverse reactions and other aspects. The 5-level Likert scoring method was adopted. The options were set as “strongly disagree,” “disagree,” “unsure,” “agree,” and “strongly agree,” with the first option “strongly disagree” given 1 point, and the following options scored in 1-point increments. The score differences between the two dimensions (the former minus the latter) reflected the risk benefit of medication administration. A positive difference value suggested that insulin demands of patients outweighed the concerns about insulin-related adverse reactions, while a negative difference value indicated the opposite.
2.2.5. Management Self-Efficacy
In addition to the two primary influencing factors on health behavior highlighted in the KAP model, knowledge and belief, we also investigated the impact of patient self-efficacy on medication adherence. Self-efficacy, defined as an individual’s subjective assessment of their capabilities in executing a particular task, has been recognized in prior research as a critical factor in diabetes management [29–31]. To assess this aspect, this study employed the Chinese version of the Diabetes Management Self-Efficacy Scale (C-DMSES), which comprised 20 items with a total score of 200 points [30]. Each item is rated on a scale of 0–10 points, with higher scores representing better self-efficacy.
2.2.6. Pharmaceutical Interventions
This study implemented sustained pharmaceutical education interventions for outpatient T2DM patients based on the KAP theoretical model. The primary objective was to enhance patient medication adherence by augmenting their knowledge, reinforcing medication beliefs, nurturing self-management efficacy, and addressing other inhibiting factors. The intervention group was subjected to specific strategies: (1) Patient education: the patients received comprehensive education on diabetes and insulin, such as insulin injection techniques and management of adverse drug reactions. (2) Promotion of healthy habits: patients were encouraged to adopt and maintain a balanced diet, increase physical activity, and enhance their self-management skills for effective diabetes control. (3)Weekly telephone follow-up: a weekly telephone follow-up was conducted over a three-month period. During these scheduled calls, patients received continuous support and guidance to address any concerns or fears related to insulin therapy and enhance their confidence in diabetes management. (4) Monthly clinic visits: patients were reminded to attend monthly clinic visits to assess their glycemic control condition and monitor overall progress. (5) Others: targeted interventions and improvements were implemented based on the analysis of factors influencing insulin adherence. The control group only underwent standard care, comprising monthly clinic visits for glucose monitoring, medication prescription, and dosage adjustment guidance.
2.3. Statistical Methods
Statistical analysis was performed using SPSS version 23.0, with a significance level set at P < 0.05. Questionnaires with ≥20% missing data were excluded from the analysis. Continuous variables with a normal distribution were presented as mean ± standard deviation, while categorical data were expressed as frequencies (percentages).
In the analysis of factors influencing medication adherence, we initially examined differences between the high adherence and low adherence groups. Two independent sample t-tests were employed for continuous variables, and chi-square tests were utilized for categorical variables. Subsequently, the logistic regression model was applied to conduct multivariate analysis on variables demonstrating significant differences between groups. In the analysis of the pharmaceutical intervention effect, comparisons between the intervention and control groups were conducted using independent sample t-tests.
3. Results
3.1. Patient Recruitment, Dropout, and Overall Evaluation of the MMAS-8 Score
During the recruitment phase, a total of 180 patients who completed the questionnaires and expressed their willingness to participate in the follow-up were included. However, throughout the course of the trial, patients who did not attend regular follow-up visits (n = 12), discontinued their medication (n = 10), or declined pharmaceutical interventions (n = 6) were excluded. As a result, the insulin adherence of 152 patients was ultimately analyzed (Figure 2). The mean medication adherence score was 4.79 ± 1.92, among whom 75 cases (49.34%) had higher adherence with the mean score being 6.37 ± 0.59 and 77 cases (50.66%) presented with lower adherence with the mean score being 3.22 ± 1.45.
3.2. Univariate Analysis of Insulin Adherence
The results of univariate sensitivity analysis of the t-test and Chi-square test on factors affecting patient medication adherence are presented in Table 2. Factors such as sex, educational levels, marital status, BMI, blood pressure, blood lipids, liver and kidney function, fasting C-peptide, 2-h postprandial C-peptide, and adverse reactions did not have significant effects (P > 0.05), while patient age (P < 0.001), diabetes duration (P < 0.001), health insurance payment methods (P = 0.03), HbA1c (P < 0.001), diabetes and medication knowledge (P < 0.001), management of self-efficacy (P < 0.001), and medication beliefs (P < 0.001) were found to have a significant impact on patient medication adherence.
| Factors | Good adherence | Poor adherence | t/x2 | P |
|---|---|---|---|---|
| (n = 75) | (n = 77) | |||
| Age (year) | 60.85 ± 13.90 | 51.18 ± 16.41 | 3.90 | <0.001 ∗∗ |
| Sex | ||||
| Men | 50 (66.67%) | 49 (63.64%) | 0.12 | 0.73 |
| Women | 25 (33.33%) | 28 (36.36%) | ||
| Education background | ||||
| Illiterate or elementary school | 3 (4%) | 3 (3.89%) | 0.23 | 0.89 |
| High school | 52 (69.33%) | 56 (72.73%) | ||
| College, university, or above | 20 (26.67%) | 18 (23.38%) | ||
| Marital status | ||||
| Married | 72 (96%) | 69 (89.61%) | 2.31 | 0.13 |
| Others | 3 (4%) | 8 (10.39%) | ||
| Medical insurance | ||||
| Self-pay | 13 (17.33%) | 27 (35.06%) | 8.87 | 0.03 ∗ |
| Employee essential medical insurance | 49 (65.33%) | 43 (55.85%) | ||
| Free medical care | 8 (10.67%) | 2 (2.6%) | ||
| Resident essential medical insurance | 5 (6.67%) | 5 (6.49%) | ||
| Diabetes duration (year) | 15.70 ± 9.77 | 8.77 ± 8.03 | 4.74 | <0.001 ∗∗ |
| BMI (kg/m2) | 24.27 ± 2.61 | 24.44 ± 3.91 | −2.56 | 0.60 |
| SBP (mmHg) | 124.67 ± 16.81 | 125.59 ± 18.36 | −0.32 | 0.75 |
| DBP (mmHg) | 84.42 ± 78.17 | 77.77 ± 10.98 | 0.73 | 0.47 |
| LDL-C (mmol/L) | 2.37 ± 0.815 | 2.53 ± 1.00 | −3.09 | 0.12 |
| Cr (umol/L) | 69.77 ± 43.93 | 60.27 ± 16.08 | 1 .76 | 0.08 |
| ALT (U/L) | 25.69 ± 17.26 | 28.08 ± 21.59 | −0.75 | 0.46 |
| AST (U/L) | 22.94 ± 10.58 | 22.52 ± 15.71 | 0.19 | 0.85 |
| Fasting C-peptide (pmol/L) | 552.08 ± 366.87 | 604.63 ± 350.04 | −0.90 | 0.37 |
| 2-h Postprandial C-peptide (pmol/L) | 1329.74 ± 830.96 | 1162.35 ± 871.31 | 1.20 | 0.23 |
| HbA1c (%) | 7.28 ± 1.33 | 9.77 ± 2.41 | −7.78 | <0.001 ∗∗ |
| Adverse reactions | ||||
| No | 58 (77.33%) | 67 (87.01%) | 2.44 | 0.12 |
| Yes | 17 (22.67%) | 10 (12.99%) | ||
| Diabetes and medication knowledge | 11.70 ± 1.04 | 7.03 ± 1.53 | 20.69 | <0.001 ∗∗ |
| Management of self-efficacy | 36.85 ± 14.18 | 79.32 ± 21.17 | 19.61 | <0.001 ∗∗ |
| Medication beliefs | 9.29 ± 2.19 | −1.69 ± 3.60 | 22.78 | <0.001 ∗∗ |
- Demographic characteristics, laboratory biochemical indicators, and scores from questionnaire surveys were systematically gathered from a total of 152 participants. Based on the MMAS-8 scores (≥6 representing good adherence and <6 representing poor adherence), patients were categorized into distinct groups. Differences of diverse variables between these groups were examined using appropriate statistical methods (the t-test for normally distributed continuous variables and the Chi-square test for categorical variables). Significance levels were marked as ∗P < 0.05 and ∗∗P < 0.01. Abbreviations: BMI, body mass index; SBP, systolic blood pressure; DBP, diastolic blood pressure; LDL-C, low-density lipoprotein cholesterol; Cr, serum creatinine; ALT, alanine aminotransferase; AST, aspartate aminotransferase; HbA1c, glycated hemoglobin.
3.3. Multivariate Analysis of Insulin Adherence
Patient adherence was taken as the dependent variable, while the factors exhibiting significant differences in the univariate analysis were considered as the independent variables. Continuous variables were categorized based on previous research [32–34], and the assignment details are presented in Table 3. The regression analysis results are listed in Table 4, which shows that factors positively correlated with patient insulin adherence included diabetes duration (OR = 1.031, P = 0.008), payment methods (OR = 1.590, P = 0.040), knowledge understanding (OR = 1.051, P = 0.005), management of self-efficacy (OR = 1.005, P = 0.002), and medication beliefs (OR = 1.506, P < 0.001), while HbA1c was negatively associated with insulin adherence (OR = 0.954, P = 0.006). Among these factors, in terms of the magnitude of the absolute β values, the payment method of medical insurance had the greatest impact on patient medication adherence (β = 0.463, P = 0.040).
| Variables | Assignment | |||||
|---|---|---|---|---|---|---|
| 0 | 1 | 2 | 3 | 4 | 5 | |
| Age (year) | 18∼29 | 30∼39 | 40∼49 | 50∼59 | 60∼70 | |
| Diabetes duration (year) | 0∼5 | 6∼10 | >10 | |||
| Medical insurance | Self-pay | Employee essential medical insurance | Free medical care | Resident essential medical insurance | ||
| HbA1c (%) | <6.5 | 6.5∼7.0 | 7.1∼9.9 | 10.0∼12.0 | >12.0 | |
| Diabetes and medication knowledge | 0∼5 | 6∼7 | 8∼9 | 10∼11 | 12∼13 | 14∼15 |
| Management of self-efficacy | <0.40 | 0.40∼0.54 | 0.55∼0.69 | 0.70∼0.84 | ≥0.85 | |
| Medication beliefs | <−5 | −5∼−2 | −1∼2 | 3∼6 | ≥7 | |
- Based on previous research and clinical experience, continuous variables among the influencing factors were transformed into categorical variables. Values were assigned to each level, facilitating subsequent logistic regression analysis.
| Factors | β | SE | Wald | P | OR | 95% CI |
|---|---|---|---|---|---|---|
| Age | 0.003 | 0.003 | 1.034 | 0.309 | 1.003 | 0.997∼1.008 |
| Diabetes duration | 0.030 | 0.011 | 7.120 | 0.008 ∗∗ | 1.031 | 1.008∼1.054 |
| Medical insurance | 0.463 | 0.225 | 4.233 | 0.040 ∗ | 1.590 | 1.022∼2.470 |
| HbA1c | −0.047 | 0.017 | 7.585 | 0.006 ∗∗ | 0.954 | 0.923∼0.987 |
| Diabetes and medication knowledge | 0.049 | 0.018 | 7.882 | 0.005 ∗∗ | 1.051 | 1.015∼1.087 |
| Management of self-efficacy | 0.005 | 0.002 | 9.395 | 0.002 ∗∗ | 1.005 | 1.002∼1.008 |
| Medication beliefs | 0.410 | 0.067 | 37.920 | <0.001 ∗∗ | 1.506 | 1.322∼1.716 |
- The statistically significant indicators identified through univariate analysis served as independent variables, while patients’ levels of medication adherence were used as the dependent variable for constructing a binary logistic regression model. The magnitude and direction of regression coefficients (β) elucidate the relationship between the log odds of influencing factors and medication adherence. A positive β value implies that the log odds increase with the elevation of the independent variable, whereas a negative β value signifies a reduction in log odds. The odds ratio (OR) quantifies the extent to which log odds change per unit increase in the independent variable. An OR value of 1 denotes the absence of correlation between the independent and dependent variables. An OR value exceeding 1 indicates an augmented odds with the increase of the independent variable, while an OR value less than 1 indicates a decreased odds. Significance levels were denoted as ∗P < 0.05 and ∗∗P < 0.01.
3.4. Pharmaceutical Intervention Results
Based on the analysis of influencing factors, the observational indicators for the pharmaceutical intervention trial included insulin adherence, HbA1c level, self-efficacy, knowledge understanding, and medication beliefs. Prior to the targeted intervention, there were no statistical differences observed in these five indicators between the intervention group and the control group (P > 0.05). Following a minimum of three months of pharmaceutical intervention, patients in the intervention group demonstrated notable improvements compared to those in the control group in terms of knowledge scores (P = 0.01), BMQ scores (P < 0.001), and C-DMSES scores (P < 0.001). Moreover, medication adherence (P < 0.001) and HbA1c levels (P < 0.001) showed significant enhancements in the intervention group. Details of the results are shown in Table 5.
| Factors | Intervention group | Control group | t | P | |
|---|---|---|---|---|---|
| Insulin adherence | Before | 5.12 ± 1.15 | 5.02 ± 0.96 | 0.58 | 0.56 |
| After | 6.65 ± 0.98 | 5.56 ± 1.46 | 5.39 | <0.001 ∗∗ | |
| HbA1c (%) | Before | 8.73 ± 2.61 | 9.02 ± 2.35 | −0.72 | 0.47 |
| After | 7.73 ± 2.66 | 9.00 ± 2.35 | −5.89 | <0.001 ∗∗ | |
| Management of self-efficacy | Before | 127.12 ± 15.69 | 129.26 ± 12.69 | −0.93 | 0.36 |
| After | 147.09 ± 20.44 | 128.10 ± 19.43 | 5.87 | <0.001 ∗∗ | |
| Diabetes and medication knowledge | Before | 10.25 ± 1.01 | 10.01 ± 1.22 | 1.32 | 0.19 |
| After | 13.56 ± 1.33 | 12.12 ± 3.27 | 3.38 | 0.01 ∗ | |
| Medication beliefs | Before | 7.75 ± 1.91 | 7.28 ± 3.21 | 1.09 | 0.28 |
| After | 10.88 ± 3.97 | 7.41 ± 6.42 | 3.99 | <0.001 ∗∗ | |
- A total of 152 participants were randomly divided into an intervention group and a control group. The intervention group underwent a comprehensive 3-month pharmaceutical intervention program, encompassing patient education, promotion of healthy habits, weekly telephone follow-up, and monthly clinic visits. Conversely, the control group solely received standard care. Disease and medication details of all patients were gathered at the beginning of the study and at the conclusion of the follow-up period. Variations in insulin adherence and its associated factors between the groups were assessed. Statistical significance was denoted as ∗P < 0.05 and ∗∗P < 0.01.
4. Discussion
Insulin therapy has been shown to be effective in improving β-cell function, rapidly relieving glucotoxicity, achieving standard blood glucose levels, and reducing the risk of microvascular complications in T2DM patients [3–7]. However, long-term insulin administration and patient follow-up require patients to possess excellent self-behavioral management capacity and medication adherence. Therefore, it is of great significance to analyze the factors that affect insulin adherence and implement pharmaceutical interventions based on these factors.
4.1. Analysis of Factors Associated with Patient Insulin Adherence
4.1.1. Age
As individuals age, the physiological functions of the human body tend to decline, especially in elderly patients who are susceptible to developing multiple diseases and complications. Managing the healthcare needs of these patients becomes more complex due to the greater variety and larger quantities of medications needed, resulting in potential challenges related to medication adherence [35]. Moreover, diabetes is associated with a higher prevalence and incidence of geriatric syndromes, including cognitive impairment, depression, and falls, which further complicate diabetes care and medication compliance [36].
4.1.2. Diabetes Duration
Patients with a longer course of disease exhibited higher medication adherence compared to those with a shorter disease duration (P < 0.05), which might be because with the prolonging course of disease, patients were more aware of the disease and could use insulin in a more standardized manner. They also formed habits such as carrying insulin with them, responding to adverse reactions timely, and having a more positive outlook on treatment as their conditions improved, thereby leading to better medication adherence.
4.1.3. Payment Methods
Patients who were covered by medical insurance exhibited higher adherence compared to those who paid for their own treatments (P < 0.05). This finding supports previous research, indicating a strong correlation between medication costs and compliance rates in various chronic diseases, including diabetes [37–40]. As insulin and injection consumables have consistently been associated with high costs, self-pay patients may be worried about the financial burden on themselves or their families and may be more inclined to skip doses or modify their treatment regimen to minimize expenses, resulting in lower adherence [11, 12].
4.1.4. Glycemic Control
Patients with poor glycemic control had evidently lower adherence compared to those achieving favorable conditions (P < 0.05). Poor glycemic control can undermine patients’ confidence in their current insulin therapy regimen. Consequently, they may feel compelled to rapidly achieve the standard level, leading to haphazard adjustments in insulin dosages or unauthorized changes in medication types, ultimately resulting in poorer adherence. In contrast, patients who maintain favorable conditions exhibit strong beliefs in conquering their disease and adhere to their insulin regimen as prescribed, fostering a positive feedback loop that reinforces medication compliance.
4.1.5. Knowledge and Understanding
Patients with a better understanding of diabetes, insulin, glycemic control goals, diet, and exercise precautions exhibited higher insulin adherence (P < 0.05). This finding supports the theoretical underpinning of the KAP model, which asserts that knowledge serves as the cornerstone of health behavior. Enhancing patients’ knowledge levels stimulates them to modify their existing health behaviors. Well-informed patients are more inclined to adhere to physicians’ instructions and, consequently, are more likely to comply with their medication regimen.
4.1.6. Management of Self-Efficacy
Patients with higher scores on the C-DMSES scale exhibited higher medication adherence (P < 0.05). They held stronger beliefs and confidence in taking specific measures, such as blood glucose monitoring, diet modification, and exercise, so as to achieve desired outcomes. Besides, these patients boasted strong persistence and were able to overcome difficulties, thereby showing elevated medication adherence [41, 42].
4.1.7. Medication Beliefs
The present study demonstrated that patients with higher BMQ scores exhibited higher insulin adherence (P < 0.05). Home et al. reported that 27.63% of patients had intense concerns about insulin-related adverse reactions and other aspects, which outweighed their needs for the medication [43]. This finding is consistent with our results and further emphasizes the importance of pharmaceutical interventions. When providing pharmaceutical care, pharmacists should thoroughly analyze the benefits and drawbacks of insulin use with patients so as to alleviate their fear of insulin administration, diminish their worries about adverse reactions, reinforce their beliefs in insulin administration, and ultimately improve their medication adherence.
This study adopts the KAP model, primarily focusing on the influence of knowledge and belief on patients’ medication adherence. In contrast, other studies have utilized the HAPA model structure [14, 44], which further breaks down self-efficacy into task, coping, and recovery self-efficacy. The aim is to bolster self-efficacy throughout interventions and emphasize the mediating role of planning between intention and action. Moreover, Babazadeh et al. [45] applied the Extended Theory of Reasoned Action (ETRA) to forecast self-care behaviors and HbA1c levels among patients with type 2 diabetes in Iran. In this model, ETRA constructs and self-care behavior emerged as the primary determinants of HbA1c levels in type 2 diabetes, suggesting its potential applicability in designing intervention programs to enhance HbA1c levels in these patient groups. However, it is worth noting that the survey tools utilized in the aforementioned studies are self-compiled questionnaire scales. In contrast, the MMAS-8 scale, BMQ scale, and C-DMSES scale used in this study are well-established tools widely used in clinical practice and research in China. They have undergone rigorous validation among Chinese populations, rendering them more suitable for use in this context. Regarding the structural aspect of the models, although the KAP model offers a relatively simplistic framework, it demonstrates a certain degree of predictive capability in elucidating the relationship between knowledge and health behavior. Conversely, the HAPA model and ETRA model, due to their structural complexity, may exhibit higher predictive performance in forecasting health behavior changes, albeit requiring additional data support. In clinical practice and research, the KAP model is widely adopted due to its simplicity and ease of operation. However, further investigation is warranted to ascertain whether this simplification compromises predictive performance. Meanwhile, the HAPA model and ETRA model may find particular applicability in certain domains, especially when a deeper understanding of behavior change processes is required.
4.2. Analysis of the Effects of Pharmaceutical Interventions
T2DM is a chronic disease that requires most patients to remain on medication to control or delay its progression. By implementing pharmaceutical interventions targeting factors that affect the adherence of patients undergoing long-term insulin administration, patients can learn more about disease and treatment in a short duration, possess continuously enhanced self-management capacity, and suffer from fewer adverse reactions, which are favorable to the better control of blood glucose levels and disease progression, thereby resulting in a higher utilization efficiency of medical resources [14–20]. In the meantime, pharmacists further improve patient medication adherence and enhance medication safety through pharmacological monitoring, medication guidance, and follow-up [15]. After pharmaceutical interventions in this study, patients in the intervention group demonstrated significantly better glycemic control, medication adherence, knowledge understanding, management of self-efficacy, and medication beliefs compared to control group patients (P < 0.05). Furthermore, significant differences were observed in the intervention group’s values before and after the interventions (P < 0.05), further confirming the efficacy of pharmaceutical interventions.
5. Conclusion
Medication compliance plays a crucial role in achieving effective glycemic control among T2DM outpatients undergoing long-term insulin administration. Our study identified several significant factors that influence insulin adherence, including age, duration of diabetes, health insurance payment methods, HbA1c level, disease and medication knowledge, diabetes management self-efficacy, and medication beliefs.
A notable strength of our investigation is its departure from the conventional diagnostic and treatment paradigm, highlighting the integral role of pharmacists in enhancing medication adherence. Our findings demonstrate the effectiveness of clinical-pharmacist-led pharmaceutical interventions in improving patient compliance, enhancing blood glucose control, and promoting rational insulin use. Furthermore, our study underscores the predictive utility of the KAP model in gauging medication adherence among T2DM outpatients.
However, it is important to acknowledge the limitations of our study, such as the limited sample size and short follow-up period. While these findings provide data-based support for diabetes management, further investigations are warranted to deepen our understanding and inform clinical practice. Future studies should consider longer follow-up periods, such as 12 or 24 months, to ascertain the sustainability of dietary and medication behaviors. Additionally, the generalizability of our findings beyond the outpatient endocrinology clinic at a tertiary care hospital in Nanjing, China, necessitates investigation across diverse regions and populations. Furthermore, given the single-center nature of our study, validation of our model’s applicability in other settings is warranted.
Additional Points
Highlights. What is already known? Insulin therapy is vital for effective glucose control in type 2 diabetes patients. Nevertheless, suboptimal adherence often results in inadequate glucose management. What has this study found? This study reveals a notable portion of outpatients (50.66%) with subpar medication adherence. Pharmaceutical intervention involving education and follow-up significantly improved medication adherence and its influencing factors, encompassing self-efficacy, knowledge comprehension, and medication beliefs. What are the implications of the study? These findings emphasize the potential of targeted pharmaceutical interventions to promote rational insulin use and improve glucose control, contributing to better management of diabetes and its associated complications.
Ethical Approval
The protocol for this research project has been approved by the Medical Ethics Committee of Nanjing Drum Tower Hospital (grant no. 2020-233-02) and has been publicly registered in the Chinese Clinical Trial Registry (ChiCTR) (registration no. ChiCTR2300074444). Throughout the entirety of the study, ethical principles and the Helsinki Declaration were strictly adhered to, with risks and discomfort to participants minimized and their personal privacy and rights protected.
Consent
All participants provided written, informed consent. Prior to the commencement of the study, the participants were clearly informed of the research purpose and were assured that all collected data would be used solely for research purposes.
Disclosure
The funding sources did not impact the design, conduct, or interpretation of the study. The MMAS-8 Scale (TX0008632533), content, name, and trademarks are protected by US copyright and trademark laws. Permission for use of the scale and its coding is required. A license agreement is available from MMAR, LLC., https://www.moriskyscale.com. (©2007 Donald E. Morisky).
Conflicts of Interest
The authors declare that there are no conflicts of interest.
Authors’ Contributions
The author list was collectively determined by the research team, with the order of authors reflecting their actual contributions to the article, in accordance with academic ethics and research integrity. Specifically, Ting He and Hao Wang share joint first authorship and made significant contributions to the investigation, data curation, and primary writing of the manuscript. Wen Sun and Lintong Li, crucial members of the clinical pharmacotherapy team, provided ancillary support, particularly in patient follow-up and medication education. The corresponding authors, Li Li and Cheng Ji, were responsible for project conceptualization, methodology, supervision, and securing funding for the research. All authors have reviewed the entire content of the manuscript and take full responsibility for its contents. Ting He and Hao Wang contributed equally to this work.
Acknowledgments
This study received support from three funding sources: Clinical Research Special Funds from Nanjing Drum Tower Hospital (grant no. 2021-LCYJ-PY-33), Research Special Funds for Lean Medication Use from Jiangsu Research Hospital Association (grant no. JY202019), and the Project of Modern Hospital Management and Development Institute, Nanjing University (grant no. NDYG2020003).
Open Research
Data Availability
The datasets generated and analyzed during the current study are available from the corresponding author on reasonable request.




