Cluster Headache Decreases Life Expectancy: A Longitudinal Assessment During 40 Years in a Headache Clinic Cohort
Abstract
Background: Cluster headache (CH) is one of the most disabling primary headaches. Nowadays, it is unknown if it has an impact on reducing life expectancy.
Methods: We calculated years of potential life lost (YPLL) in deceased individuals from a CH registry of a third-level hospital, using as cutoff the estimated life expectancy for our general population according to their sex and year of death. Furthermore, a descriptive and comparative analysis of the main causes of death, risk factors, and toxic habits was carried out.
Results: There were 25 deaths among the 152 individuals included. Twenty-one (84%) died earlier than expected with a mean of 9.14 YPLL (p = 0.001). Cancer was the most common cause of death in CH patients (64% of deaths vs. 28.5% expected in general population, p ≤ 0.001). Eighty percent and 45% of our deceased patients were smokers and 60% and 45% regular alcohol consumers at the diagnosis of CH and at death, respectively. The percentage of smokers at diagnosis was significantly higher than that in the reference population (80% vs. 33.2%, p < 0.001). There was a significantly higher frequency of arterial hypertension (76% vs. 19.82%, p < 0.001) and diabetes mellitus (40% vs. 7.8%, p < 0.001) at death in CH individuals compared to general population.
Conclusions: CH implies a loss of almost one decade of life expectancy by an increase in cancer deaths. Tobacco and alcohol consumption seem to be the main underlying causes. These results call for an action plan for a better management of CH patients since their diagnosis.
1. Introduction
Cluster headache (CH) is the most common trigeminal-autonomic cephalalgia and one of the most disabling primary headaches. Its relatively low incidence and its relevant diagnostic delay [1], as well a diagnosis purely based on clinical criteria [2], explain that there is still scarce knowledge of some of the characteristics of this disease, such as its potential long-term consequences in terms of morbi-mortality. In spite of this, it is well known that individuals who suffer from CH frequently associate unhealthy lifestyle habits, mainly regular consumption of different toxic substances as alcohol, tobacco, or other illicit drugs, which can contribute to a higher mortality [3]. The consumption of these substances has been associated with a wide list of potentially fatal conditions, highlighting, due to their frequency, cardiovascular diseases and cancer [4–6]. Up to now, there are no studies analyzing morbi-mortality risk in CH patients; hence, it is unknown whether suffering from this entity implies a risk of premature mortality and if there are modifiable factors or individuals who may benefit from preventive measures and changes in lifestyle habits.
There are different ways of evaluating the mortality associated with a disease or certain factors, among which the concept years of potential life lost (YPLL) stands out as a measure to determine more precisely the mortality and its impact, especially in younger individuals. This term refers to the average number of years that a person has not been able to live due to having died prematurely, and one of the ways to calculate it is by subtracting the age at death from a selected cutoff’s age [7, 8]. One of the issues related to this index is that there is a need to conduct studies with long-term follow-up, but CH patients are diagnosed at young age. In relation to this statement, our Headache Clinic maintains a longitudinal registry of patients diagnosed with CH since 1984 [9]. Our aim was to determine whether patients with CH in our registry had a reduced life expectancy compared to the general population of our region and to analyze the possible associated risk factors.
2. Methods
Review of data from a CH registry of a tertiary, university hospital in north of Spain. The study was approved by our Ethics Committee (registration number 137/2021). We performed a descriptive analysis of the causes and age at death of the individuals who had been diagnosed as CH in our Headache Clinic since January 1984. Our Headache Clinic is the reference center for diagnosis and management of patients with CH and the only existing (including private practice) in our region. CH diagnosis was performed by a neurologist with experience in headache according to the current ICHD-3 criteria [2]. We excluded patients with other trigeminal-autonomic headaches, with less than 1 year of follow-up or lack of information in their medical charts, and patients with cardiovascular diseases or cancer at the moment of diagnosis. Dates and causes of death were obtained from death certificates and clinical data including demographics and risk factors from health records.
In order to assess the morbidity and mortality associated with this entity, we calculated the YPLL, comparing the age at death of these patients with the expected life expectancy for their sex and year of death estimated for the general population of our region, according to the “Instituto Nacional de Estadística” annual report [10]. As per our official census, the population of our Health Area has ranged from 295,565 in 1984 to 321,553 in 2023.
A comparative analysis was made between the main characteristics (toxic habits and vascular risk factors) at diagnosis and at death of the deceased CH patients and the estimated prevalence of these factors in our general population. We selected for this comparative analysis the highest prevalence collected for these factors in general population since 1987, according to the “Encuesta Nacional de Salud.” “Encuesta Nacional de Salud” is a national registry with information from a serial set of surveys (every 2–5 years) that constitute the main source of information about health perceived by the population residing in our country, being one of the greatest data collection programs of our Ministry of Health. It provides data on population health and its determinants, the magnitude and distribution of the illness and disability, and access to and use of health services on the population living in main family homes (n = 37,500) at national and regional level [11].
2.1. Statistical Analysis
SPSS software was used to perform the statistical analysis. Kolmogorov–Smirnov test was used to determine if the continuous variables met characteristics of a normal distribution. The results obtained in the descriptive analysis were expressed with a measure of central tendency (mean or median) and a measure of dispersion (standard deviation or interquartile range). Wilcoxon rank-sum test was used for the comparative analysis between the age at death of CH patients and their estimated life expectancy according to their sex and year of death (given that the estimated life expectancy sample did not follow a normal distribution), and Student’s t-test was used to compare the average of YPLL between episodic cluster headache (eCH) and chronic cluster headache (cCH) subgroups. For the comparative analysis between the characteristics of the deceased individuals with eCH and cCH, Mann–Whitney U test was used for continuous variables and Fisher’s exact test for the dichotomic ones. A significant difference was considered to exist if p < 0.05.
3. Results
Our CH registry contains a total of 155 patients, of whom 152 fulfilled the study criteria. One hundred and twenty-nine (84.9%) met criteria for eCH and 23 (15.1%) for cCH. Most of them were males (137, 90.1%) with a mean age of 60.6 years old at the time of this analysis (standard deviation 13.8) and a follow-up time range of 1–37 years. The mean age at the onset of symptoms was 32.6 (standard deviation 11.2 years) and the median age at diagnosis was 38 years (interquartile range 17.5), which represents a mean diagnostic delay of 6 years.
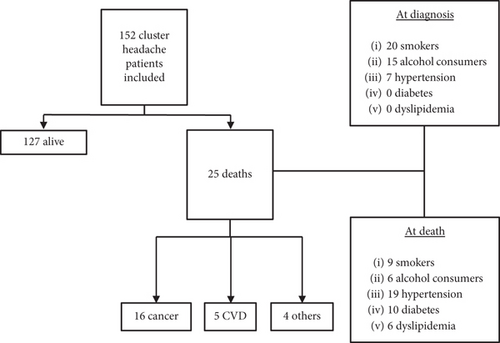
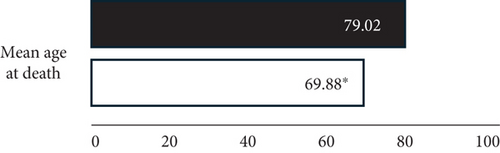
There were 25 (16.1%) deaths at the time of the analysis (Figure 1). Comparing their ages at death with their assumed life expectancy, 21 (84%) deceased CH patients lived less than expected. The global average of YPLL was 9.14 years (p = 0.001) (Table 1 and Figure 2). A comparative analysis was carried out between the number of deaths in the eCH and cCH subgroups. Deaths were significantly higher in individuals with cCH (8/23, 34.8%) than in those with eCH (17/129, 13.2%) (χ2 = 6.6298, p = 0.010), and individuals with cCH presented a higher average of YPLL than eCH (13.50 vs. 7.08), although this difference was not significant (mean difference: 6.41 [95% CI −3.31 to 16.14], p = 0.186). The comparative analysis between the characteristics of the deceased individuals with eCH and those with cCH did not show significant differences (Table 2).
| Patient | Sex | Diagnosis | Cause of death | Age (year) at death | Estimated life expectancy | YPLL |
|---|---|---|---|---|---|---|
| 1 | M | cCH | Rectal cancer | 62 (2019) | 80.93 | 18.93 |
| 2 | M | eCH | Hypertensive cardiomyopathy | 92 (2017) | 80.34 | −11.66 |
| 3 | M | cCH | Pancreatic cancer | 69 (2017) | 80.34 | 11.34 |
| 4 | M | eCH | Lung cancer | 69 (2015) | 79.74 | 10.74 |
| 5 | M | cCH | Prostatic cancer | 72 (2007) | 77.42 | 5.42 |
| 6 | M | eCH | Peritonitis | 82 (2011) | 79.07 | −2.93 |
| 7 | M | eCH | Pancreatic cancer | 78 (2008) | 78.22 | 0.22 |
| 8 | M | eCH | Colon cancer | 66 (2017) | 80.34 | 14.34 |
| 9 | M | eCH | Rectal cancer | 76 (2013) | 80.00 | 4.00 |
| 10 | M | eCH | Bladder cancer | 76 (2016) | 80.12 | 4.12 |
| 11 | M | cCH | Duodenal cancer | 72 (1994) | 74.71 | 2.71 |
| 12 | M | cCH | Heart attack | 62 (2014) | 79.63 | 17.63 |
| 13 | F | Cluster-TIC | Iatrogenic brain hematoma | 59 (2003) | 84.13 | 25.13 |
| 14 | M | eCH | Leukemia | 56 (1992) | 73.64 | 17.64 |
| 15 | M | eCH | Myelodysplastic syndrome | 76 (2012) | 79.34 | 3.34 |
| 16 | M | eCH | Stroke | 87 (2013) | 80.00 | −7.00 |
| 17 | M | cCH | Lung cancer | 63 (2011) | 79.07 | 16.07 |
| 18 | M | eCH | Lung cancer | 65 (1997) | 74.90 | 9.90 |
| 19 | F | eCH | Thyroid cancer | 77 (1996) | 82.60 | 5.60 |
| 20 | M | eCH | Esophagus cancer | 63 (1995) | 74.27 | 11.27 |
| 21 | M | eCH | Suicide (drug overdose) | 43 (2011) | 79.07 | 36.07 |
| 22 | M | eCH | Gastric cancer | 50 (2004) | 76.99 | 26.99 |
| 23 | M | eCH | Traumatic brain injury | 74 (2012) | 79.34 | 5.34 |
| 24 | F | cCH | Heart attack | 75 (2013) | 85.81 | 10.81 |
| 25 | M | eCH | Cardiac failure | 83 (1998) | 75.51 | −7.49 |
| eCH (n = 17) | cCH (n = 8) | p | |
|---|---|---|---|
| Male sex | 16 (94.1%) | 6 (75.4%) | 0.231 |
| Mean age at onset | 40.60 (n = 15) | 47.50 | 0.130 |
| Mean age at death | 71.35 | 66.75 | 0.353 |
| YPLL | 7.08 | 13.50 | 0.186 |
| Tobacco at diagnosis | 14 (82.4%) | 6 (75.0%) | 1.000 |
| Tobacco at death | 5 (29.4%) | 4 (50%) | 0.394 |
| Alcohol at diagnosis | 11 (64.7%) | 4 (50%) | 0.667 |
| Alcohol at death | 5 (29.4%) | 1 (12.5%) | 0.362 |
| Hypertension at diagnosis | 3 (17.6%) | 4 (50%) | 0.156 |
| Hypertension at death | 12 (70.6%) | 7 (87.5%) | 0.624 |
| Diabetes at diagnosis | 0 | 0 | — |
| Diabetes at death | 7 (41.2%) | 3 (37.5%) | 1.000 |
| Dyslipidemia at diagnosis | 0 | 0 | — |
| Dyslipidemia at death | 3 (17.6%) | 3 (37.5%) | 0.344 |
We performed an analysis of the causes of death in individuals with CH, grouping the different causes of death into three categories: cancer, cardiovascular diseases, and other causes. Cancer was the most common cause of death among them (16/25, 64%), followed by cardiovascular diseases (5/25, 20%). Only one of the deceased patients committed suicide. Subsequently, a comparative analysis was carried out between the percentage of deaths for each of the categories in CH patients and in our general population, according to data from the “Encuesta Nacional de Salud” [11]. The percentage of cancer deaths was significantly higher in those with CH than those in general population (64% vs. 28.5%, p < 0.001), while no significant differences were observed in the percentage of deaths from cardiovascular disease between both subgroups (Table 3).
| Causes of mortality | General population | Cluster headache registry | p | ||
|---|---|---|---|---|---|
| N | % | N | % | ||
| Cancer | 31,937 | 28.5 | 16 | 64 | ≤ 0.001 |
| Cardiovascular diseases | 33,230 | 29.6 | 5 | 20 | 0.292 |
| Other causes | 47,032 | 41.9 | 4 | 16 | 0.008 |
| Total | 112,199 | 100 | 25 | 100 | |
Regarding cardiovascular risk factors, among the 25 CH died patients, 20 (80%) were smokers at diagnosis and 9 (45%) continued smoking until death. The 11 former smokers had stopped smoking at an average of 16 years before death. Only 3 of the 17 (17.6%) deceased patients who died from cancer were not smokers at diagnosis of the headache. Regarding alcohol consumption, and considering as regular alcohol drinkers those who consumed 5 or more alcoholic drinks a day [10], 15 (60%) of the deceased patients were regular alcohol consumers at diagnosis, and 40% (6/15) of them maintained alcohol consumption until their death. None of the deceased patients had a previous history of other toxic substance consumption. In addition, 7 (28%) of the CH patients who had died had arterial hypertension at diagnosis, and this percentage increased to 76% (19/25) at the time of death. No patient had a previous history of diabetes or dyslipidemia at diagnosis, although 10 (40%) developed diabetes at follow-up and 6 patients (24%) had dyslipidemia at death. No significant differences in these factors were observed between patients with eCH and cCH.
Finally, we carried out a comparative analysis between the prevalence of these factors at diagnosis and at death in the deceased CH patients from the registry and the general population (the highest prevalence recorded since 1987 for our population according to the “Encuesta Nacional de Salud”). We found a significantly higher percentage of smokers at diagnosis and of arterial hypertension and diabetes at death in the CH patients who had died compared to the overall population of our region (Table 4).
| Risk factor | General population | Cluster headache registry | p | ||
|---|---|---|---|---|---|
| % | N | % | |||
| Tobacco | 33.18 | At diagnosis | 20 | 80 | <0.001 |
| Alcohol | 48.35 | At diagnosis | 15 | 60 | 0.244 |
| Hypertension | 9.82 | At diagnosis | 7 | 28 | 0.305 |
| At death | 19 | 76 | <0.001 | ||
| Diabetes | 7.8 | At diagnosis | 0 | 0 | — |
| At death | 10 | 40 | <0.001 | ||
| Dyslipidemia | 17.92 | At diagnosis | 0 | 0 | — |
| At death | 6 | 24 | 0.428 | ||
4. Discussion
According to our findings, CH implies a potential decrease in the life expectancy of almost one decade. Mortality can be assessed in different ways. YPLL is a measure that the Global Burden Disease Group (GBDG) has used extensively in its reports [8]. This measure is complementary to mortality rate, offers a public health view, and allows comparisons of results between different populations and the impact of the disease on mortality [12]. To calculate YPLL, we carefully used as cutoff age the estimated life expectancy in their year of death according to their sex. It was decided to select this cutoff and not others, such as 65 or 70 years old used in other studies [7, 8], because we considered that the estimated life expectancy represents more faithfully the YPLL from a health point of view [13]. To our knowledge, these results are the first description of the existence of a premature mortality in patients with CH. It is important to note, therefore, that the diagnosis of CH not only entails a significant loss of quality of life due to economic burdens and job-related issues because of its disabling nature [14] but is also a risk of premature mortality with the relevance that this implies and the need for increased awareness by the clinicians.
The premature mortality observed here in CH patients is mainly explained by a greater number of deaths associated with neoplasms compared to the general population. Cancer is the second most common cause of death in our country [15], only behind cardiovascular events. Research has shown that certain risk factors may increase an individual’s chances of developing cancer. Most cancer risk factors are identified in epidemiology studies and include genetic and epigenetic factors, lifestyle habits as consumption of toxic substances and others as diet, infectious agents, or radiation exposure. Tobacco has been identified as the main single cause of cancer incidence and mortality worldwide, being one of the main risk factors for suffering from a wide variety of neoplasms (lung, oral cavity, pharynx, nasal cavity, larynx, esophagus, stomach, pancreas, uterine cervix, kidney, and others) [16]. Based on our results, it is very likely that the underlying cause of the increase in cancer deaths among this CH cohort is the high prevalence of smokers [17]. This fact is also supported by the cancer subtypes identified at death (lung, colorectal, gastroduodenal, and pancreatic cancers), whose relationship with tobacco is well established [16]. In accordance with the previous studies [18], our CH cohort had a high prevalence of active smoking habit, much higher than that recorded in our overall population. Several studies have shown that tobacco exposure is associated with CH chronification, attack frequency, bout duration, and headache-related disability [19], and the long-term effects of smoking in our patients (most of the patients continued smoking to death) may contribute to the risk of developing cancer. Although we have not observed a significant difference in the percentage of regular alcohol consumers between individuals with CH and the general population (60% vs. 48.3%, p : 0.244), alcohol is a known carcinogen, whose consumption is proportionally related to the risk of developing upper gastrointestinal tract, liver, or breast cancer [20] and it surely exerts a synergistic deleterious effect with tobacco in this regard [21]. These results are superimposable to those well demonstrated in neuropsychiatric disorders such as schizophrenia [22].
On the other hand, although the existence of a higher proportion of fatal vascular events among deceased individuals with CH has not been confirmed, we have observed a higher proportion of arterial hypertension and diabetes mellitus at the time of their death than the estimated in general population of our region. As with cancer, alcohol and tobacco are two known risk factors for the development of hypertension and diabetes [23–25], so the excessive consumption of these two substances could explain these findings. Furthermore, patients with CH usually receive corticosteroid treatment throughout their illness, and this could also contribute to the development of both comorbidities [26].
Finally, as a notable finding, we have observed a significantly higher percentage of deaths in individuals with cCH compared to those with an episodic form. According to our results and given that both populations presented similar risk factors and toxic habits, the underlying cause of this finding is unknown, and more studies will be necessary to determine whether truly presenting a chronic form implies an even greater risk of death.
Tobacco is responsible of approximately 5,000,000 deaths per year worldwide and leads to a reduction in lifespan of at least one decade. However, recently, studies showed that stopping its consumption before age 40 avoids about 90% of the excess risk of death as compared to those who continued, and for those quitting by age 30, the benefit approaches the rate of never-smokers [27]. Possibly, the underlying cause of the high frequency of substance abuse in patients with CH is a personality trait characteristic of this entity, which makes them especially prone to these unhealthy habits [28] or the existence of a common pathophysiological pathway between CH and substance abuse, in which dopamine and orexins could be involved [29]. Even though there is a significant diagnostic delay in many CH patients [30–32], they present their first symptoms around the age of 30, which should be an ideal moment to establish measures aimed at cessation of toxic consumption in order to try to reduce their mortality. Neurologists are used to encourage the cessation of tobacco and alcohol consumption in other patients (mainly with neurovascular disorders), but we must also keep this in mind in patients with headache disorders considering that probably, given that these are diseases that mostly affect young people, the benefit here would be much greater.
Our study has some potential limitations. Even though we collected patients prospectively and most of them were followed at least annually, in this work, we analyzed patients’ charts retrospectively, which could possibly underestimate, for instance, data on associated morbidities. In addition, there was no ad hoc matched control group with longitudinal follow-up as would have been desirable. The general population report chosen was not specifically designed for this study, and therefore, both groups might be not fully comparable. However, in order to avoid false significant differences, we selected the highest prevalence reported of the different vascular risk factors and toxic habits in the general population of our region since 1987 for the comparative analysis. Finally, the study was carried out in a rather small CH population sample from a specialized Headache Clinic, and our results are not necessarily extrapolated to the whole patients with CH.
5. Conclusion
In our longitudinal experience, the diagnosis of CH implies a loss of almost 10 years of potential life. This fact is justified mainly by a significant increase in deaths from cancer. Tobacco consumption, significantly higher in CH patients than in the general population, could be the underlying cause of the increase in deaths from cancer, and alcohol intake probably exerts a synergistic effect. Considering the relevant prevalence of CH (at least 1 case per 2074 persons in the general population according to our data), its nature as a chronic disease, and its usual onset at early ages, this incremental morbi-mortality shows that it would be essential to establish an action plan for a prompt diagnosis and a better management of this condition. Physicians must be aware of these risk factors since CH diagnosis and should include promotion of healthy lifestyle habits with emphasis in stopping tobacco consumption in the therapeutic program of patients with CH.
Conflicts of Interest
The authors declare no conflicts of interest.
Funding
No funding was received for this manuscript.
Open Research
Data Availability Statement
The data that support the findings of this study are available on request from the corresponding author. The data are not publicly available due to privacy or ethical restrictions.




