A Case of Anti-SAE1 Dermatomyositis
Abstract
Introduction. Anti-SAE1 antibodies have a low prevalence in dermatomyositis patients. Case Description. A 61-year-old woman presented with progressive shortness of breath, arthralgia, heliotrope rash, Gottron’s papules, and erythematous rash. She had an interstitial lung disease (ILD) with a significant decrease in lung function. There was no muscle involvement. Immunological laboratory test results showed strongly positive anti-SAE1 antibodies. Glucocorticoid treatment resulted in remission of dermatomyositis. Conclusion. Anti-SAE antibodies in dermatomyositis patients are closely linked to unique clinical features.
1. Introduction
Dermatomyositis is an idiopathic inflammatory myopathy with a wide variability in clinical presentation due to a range of cutaneous and systemic manifestations. This includes variety in muscle and joint manifestation, pulmonary manifestation, and association with malignancy. This inconsistency creates a diagnostic challenge for physicians. Myositis-specific autoantibodies (MSAs) are antibodies which are only found in inflammatory myopathies, and some MSAs are specific for dermatomyositis [1]. Every MSA is closely linked to both unique clinical features, response to treatment and prognosis [2]. In 2007, antismall ubiquitin-like modifier 1-activating enzyme (SAE1) antibodies were identified as a dermatomyositis-specific MSA [3]. Its frequency among dermatomyositis patients is very low, ranging from 1.5% to 8.0% [4]. As few patients with anti-SAE1 dermatomyositis have been described, it is important to describe more cases of this rare subtype. We describe one patient with anti-SAE1 dermatomyositis.
2. Case Presentation
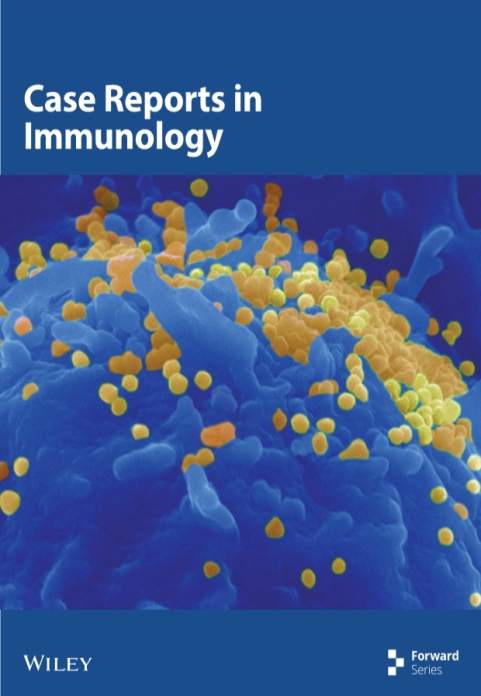
The patient characteristics and the main clinical features are given in Table 1. A 61-year-old Caucasian woman with a medical history of hypertension, interstitial cystitis, and anteroseptal myocardial infarction presented to our outpatient clinic. For her comorbidities, she used the following medication: carbasalate calcium, perindopril, nitrofurantoin, celecoxib, and amitriptyline. She presented with progressive shortness of breath, fatigue, arthralgia, and skin alterations. The skin alterations were the initial complaints; she suffered from and was thought to have antibiotic hypersensitivity. She was treated with amoxicillin clavulanate for pneumonia. However, skin alterations persisted after discontinuation of the antibiotics. She had no complaints of dysphagia, muscle pain, or proximal muscle weakness. Her vital signs were normal. Physical examination revealed a heliotrope rash and Gottron’s papules on the dorsal metacarpophalangeal and proximal interphalangeal joints and an erythematous rash on her back and upper leg. Laboratory test results are given in Table 1. Pulmonary function testing showed a vital capacity of 2.08 L, which was 70% of the predicted value, and a diffusing capacity for carbon monoxide of 54% of the predicted value. CT scan showed diffuse consolidations, suspect for interstitial lung disease (ILD) (Figure 1(a)).
| Gender | Female |
|---|---|
| Age | 61 years |
| Medical history | Hypertension, interstitial cystitis, and anteroseptal myocardial infarction |
| Symptoms | Progressive shortness of breath, fatigue, arthralgia, and skin alterations |
| Physical examination | Heliotrope rash, Gottron’s papules on the dorsal metacarpophalangeal and proximal interphalangeal joint, and an erythematous rash on back and upper leg. There was no muscle weakness |
| Laboratory test results | 2018: hemoglobin 8.8 mmol/L; leucocytes 4.4 10 ∗ 9/L; CRP 5 mg/L; ASAT 332 IU/L; ALAT 282 IU/L; LDH 377 IU/L; ALP 170 IU/L; GGT 101 IU/L; bilirubin 9 µmol/L; CK 198 IU/L; complement analysis: normal; ANA: positive (nuclear dense speckled (AC-2) and nuclear fine speckled (AC-4) pattern); ANCA (MPO/PR3): normal; rheumatoid factor IgM: normal; CCP antibody: normal |
| Immunological laboratory tests |
|
| Histology | Skin biopsy: H&E staining showed vacuolar changes in the basal layer of the epidermis and perivascular lymphocytic infiltration of the dermis. Immunofluorescence: dispositions of IgA, IgG, and IgM in the basal membrane which is compatible with dermatomyositis and cutaneous lupus erythematosus |
| Pulmonary function testing | 2018: vital capacity: 2.08 L (70% of the predicted value); diffusing capacity for carbon monoxide: 54% of the predicted value |
| Imaging | See Figure 1 |
| Treatment | Methylprednisolone (1000 mg a day for three days) followed by prednisolone 60 mg every day, which eventually was tapered down to 5 mg every day. Azathioprine was discontinued because of thrombocytopenia |
- CRP, C-reactive protein; ASAT, aspartate aminotransferase; ALAT, alanine aminotransferase; LDH, lactate dehydrogenase; ALP, alkaline phosphatase; GGT, gamma-glutamyl transpeptidase; CK, creatinine kinase; ANA, antinuclear antibodies; ANCA, antineutrophil cytoplasmic antibodies; CCP, cyclic citrullinated peptide. ∗Systemic sclerosis and myositis antibodies were determined by line immune assay (Euroline profile, Euroimmun, Lübeck, Germany, according to manufacturer’s instructions).

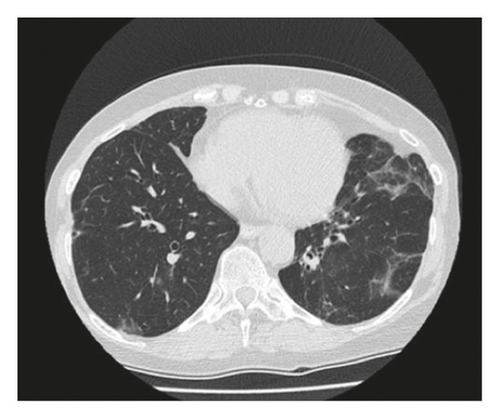
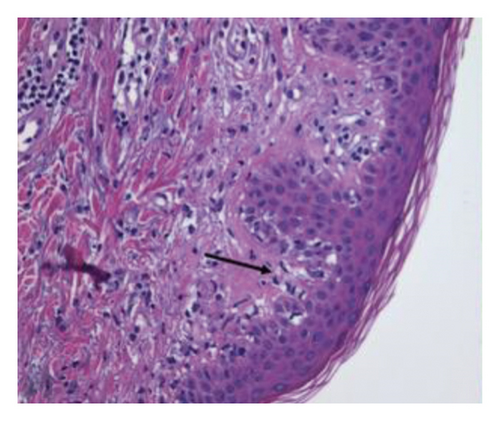
Skin biopsy hematoxylin and eosin (H&E) staining showed vacuolar changes in the basal layer of the epidermis and mild perivascular lymphocytic infiltration of the dermis (Figure 2(a)). Direct immunofluorescence showed depositions of IgA, IgG, and IgM in the basal membrane zone which is compatible with dermatomyositis and cutaneous lupus erythematosus. Immunological laboratory test results showed strongly positive anti-SAE1 antibodies. The antinuclear antibodies (ANA) determination by indirect immunofluorescence (IIF) on HEp-2 cells is shown in Figure 2(b). This shows a positive ANA with both nuclear dense speckled (AC-2) and nuclear fine speckled (AC-4) pattern, the latter being compatible with anti-SAE1 reactivity.
Our patient was admitted to the hospital for methylprednisolone treatment (1000 mg a day for three days). An abdominal ultrasound was preformed to screen for malignancy and because of the elevated liver enzymes, but no abnormalities were found. After three days of treatment with methylprednisolone, we started prednisolone 60 mg every day, which eventually was tapered down to 5 mg every day. She was shortly treated with azathioprine. This was discontinued due to thrombocytopenia. Monotreatment with low-dose prednisone 5 mg/day was, however, sufficient. The elevated liver enzymes abated during treatment. The dermatomyositis is in remission. Last control was in November 2021 (2 years after start of treatment).
3. Discussion
Anti-SAE1 antibodies are relatively rare in dermatomyositis patients with a very low prevalence ranging between 1.5 and 8.0%, and only few patients have been described so far. There is heterogeneity in clinical features among patients. Moreover, there seems to be difference in clinical presentation between Western and Asian populations, which creates a diagnostic challenge for clinicians [5].
Cutaneous disease was the initial manifestation of the dermatomyositis in our patient, which is a frequent finding in anti-SAE1-positive dermatomyositis patients. However, there is also a subset which presents with skin and muscle disease simultaneously. Typical findings in anti-SAE1 positive patients are heliotrope rash, Gottron’s sign, and papules. An erythematous rash is also described in a subset of patients [1]. Dysphagia is present in 47% of patients [5].
The prevalence of ILD among anti-SAE1 positive patients is nearly 50% and is usually mild, with few patients having respiratory complaints despite having abnormalities on imaging, which are compatible with ILD. However, our patient did experience respiratory symptoms and had significant decrease in lung function. The characteristics of ILD in anti-SAE1 patients on chest HRCT are subpleural peripheral-dominant small ground glass opacities, corresponding to organizing pneumonia [2].
As other MSAs, anti-SAE1 antibodies may be associated with an increased risk of cancer. Therefore, tumor screening is recommended after initial diagnosis in all dermatomyositis patients [6]. Most studies on anti-SAE1 antibodies and cancer show a positive association [5, 7–9]. All anti-SAE1 positive patients who developed cancer suffered from adenocarcinoma. These adenocarcinomas were from cervical, pulmonary, esophageal, or rectal origin. The frequency of cancer in anti-SAE1-positive patients in studies included by Lu et al. ranged between 14% and 57% [10]. However, a common denominator of these studies was a small sample size.
Glucocorticoid treatment is the preferred treatment in dermatomyositis patients. Both monotherapy with glucocorticoids as combined treatment with glucocorticoid and immunosuppressive agents (methotrexate, cyclophosphamide, cyclosporine, tacrolimus, rituximab, thalidomide, or immunoglobulins) are described as treatment for anti-SAE1 positive patients [4].
In conclusion, anti-SAE1 antibodies are relatively rare in dermatomyositis patients. Classical findings in anti-SAE1 positive patients are heliotrope rash, Gottron’s sign, and papules, muscle weakness, and dysphagia. Additional findings include mild interstitial lung disease, and there may be an increased risk of cancer. Glucocorticoid treatment is the preferred first-line treatment in dermatomyositis patients.
Conflicts of Interest
The authors declare that they have no conflicts of interest.
Open Research
Data Availability
The clinical data used to support the findings of this study are included within the article.