[Retracted] Analysis of the Effect of Mindfulness Behavior Intervention Combined with Progressive Breathing Training on Pulmonary Function Rehabilitation in Patients with Chronic Obstructive Pulmonary Disease
Abstract
Purpose. Studies have shown that 50%–70% of patients with chronic obstructive pulmonary disease (COPD) have fatigue in addition to respiratory symptoms, so relieving respiratory symptoms and reducing fatigue are the main treatment objectives for COPD patients. This study focuses on the effect of positive behavioral intervention combined with progressive breathing training on pulmonary function rehabilitation in patients with COPD. Methods. 86 patients who underwent COPD treatment in our hospital between August 2020 and December 2021 were selected as study subjects and were divided into control (n = 43) and study groups (n = 43) using the random number table method. Patients in the control group were given conventional care, treatment, and health guidance, while patients in the study group were given positive behavioral intervention combined with progressive breathing training on this basis. Patients in both groups were compared on the basis of Multidimensional Fatigue Inventory 20 (MFI-20) score, the Medical Coping Questionnaire (MCMQ score), the Massive Attentional Awareness Scale (MAAS) score, and pulmonary function indicators (including the percentage of forced expiratory volume one second (FEV1%), peak expiratory flow (PEF), forced vital capacity (FVC), and 6-min walk distance (6MWD)) and quality of life (MCMQ) scores before and after 12 weeks of intervention. Results. After 12 weeks of intervention, the study group had higher MFI-20 scores (comprehensive fatigue, physical fatigue, reduced activity, decreased power, and mental fatigue), confrontation scores on the MCMQ scale, MAAS scores (observation, description, nonjudgmental to intrinsic experience, nonresponsiveness to intrinsic experience, and perceived behavior), FEV1%, PEF, FVC, and 6MWD levels than the control group (P < 0.05). The scores of avoidance and submission on the MCMQ scale, and all scores of quality of life (cough, expectoration, shortness of breath, chest tightness, housework, going out, sleep, and energy) were lower than those of the control group (P < 0.05). Conclusion. Positive behavioral interventions combined with progressive breathing training have a strengthening effect on the clinical treatment of COPD patients. Positive behavioral interventions combined with progressive breathing training are simple to implement as individual self-regulation methods and can be practiced on their own after being familiar with certain methods and techniques, and long-term adherence helps individuals cope with the stimulation of adverse events. Trail Registration. The clinical registration number for this research is L2020083.
1. Introduction
Chronic obstructive pulmonary disease (COPD), a common disease in the elderly population, is characterized by airflow limitation, and patients mainly suffer from dyspnea, cough, shortness of breath, and wheezing, which can lead to chronic respiratory failure and spontaneous pneumothorax as the disease progresses, thus seriously affecting their daily lives [1]. Our COPD surveillance report [2] showed that the prevalence of COPD in people aged ≥40 years was about 13.6%. In reality, COPD patients suffer from long-term physical and psychological symptoms such as dyspnea, fatigue, cough and sputum, decreased activity endurance, anxiety, and depression, and they have physical and psychological disorders that lead to limitations in daily activities, decreased quality of life, and high readmission and mortality rates [3, 4].
There is no curative treatment for COPD, and treatment measures mainly consist of pharmacological and nonpharmacological treatments, and pharmacological treatments are mostly used to control the disease and delay its progression [5]. However, medications cannot address the de-adaptation effect of COPD patients due to dyspnea and limited mobility, and this de-adaptation can cause a further decrease in mobility, creating a vicious cycle [6]. Therefore, pharmacological treatment needs to be accompanied by long-term nonpharmacological treatment. Pulmonary rehabilitation exercises are considered the cornerstone of pulmonary rehabilitation programs and are essential in the rehabilitation of COPD patients to prevent and improve dyspnea and motor dysfunction due to airflow limitation and respiratory and skeletal muscle dysfunction in COPD patients [7, 8]. Progressive breathing training enhances ventilation and ventilation, improves respiratory muscle endurance, corrects pathological breathing patterns, promotes sputum expulsion, and enhances cardiac and pulmonary aerobic endurance, thereby improving the patient’s ability to perform activities of daily living [9]. However, patients are prone to fatigue, poor results, and poor compliance with respiratory muscle function training alone. Mindfulness behavior intervention originated from ancient Eastern meditation. Originating from ancient Eastern meditation practices, positive behavioral interventions aim to emphasize the individual’s ability to maintain attention and alertness to the task at hand, focus the mind on the activity being performed, promote rehabilitative exercise, and reduce the psychological burden of the patient. The efficacy of mindfulness therapy on clinical patients’ quality of life, sleep quality, negative emotions, and postoperative pain has been widely recognized in recent years among a variety of psychological interventions [10, 11].
However, few studies have been reported on the combined use of positive behavioral intervention and progressive breathing training in COPD in China. The aim of this study was to investigate the effects of mindfulness behavioral intervention and progressive breathing training on fatigue and cardiopulmonary function in stable COPD patients, with the aim of providing a theoretical basis for the clinical implementation of this combined training for COPD patients.
2. Information and Methods
2.1. Study Population and Grouping
In this study, 86 patients who underwent COPD treatment in our hospital between August 2020 and December 2021 were selected as study subjects and were divided into control (n = 43) and study groups (n = 43) using the random number table method.
2.1.1. Inclusion Criteria
- (i)
Those who were conscious, thinking normally, and able to communicate verbally.
- (ii)
Patients who met the diagnostic criteria for chronic obstructive pulmonary disease [12].
- (iii)
Patients and their families who gave informed consent to participate in the study program.
- (iv)
Stable condition with treatment.
- (v)
Primary school and above with basic literacy skills.
- (vi)
GOLD graded as I-III [13].
2.1.2. Exclusion Criteria
- (i)
Those with a history of mental illness and serious complications such as impaired consciousness, chronic respiratory failure, or pulmonary encephalopathy.
- (ii)
Those with combined cancer and combined tuberculosis.
- (iii)
those who required continuous noninvasive or invasive mechanical ventilation and hemodynamic instability.
- (iv)
Combination of other diseases that affect daily activities, such as muscle, joint, and vascular diseases.
2.2. Methods
2.2.1. Control Group
Patients in the control group were given symptomatic treatment such as expectorants and bronchodilators during hospitalization and routine nursing measures in internal medicine. After admission, the responsible nurse gave targeted nursing interventions according to the patients’ complaints and physical symptoms and also provided verbal health education and psychological guidance.
2.2.2. Study Group
- (1)
A multidisciplinary COPD management team was established. The team members received unified theoretical training and passed the operational skills test, and were proficient in the theories and intervention methods related to positive behavioral intervention and progressive breathing training.
- (2)
Assess the cognitive ability of the patient. The nurse-in-charge fully understood the patient’s condition and past medical history and took the initiative to communicate with the patient and family members to understand their awareness of COPD and self-care ability, to identify the patient’s problems in the process of disease treatment and rehabilitation, and to develop a targeted cognitive-behavioral intervention plan accordingly.
- (3)
Carry out cognitive-behavioral interventions.
- (i)
Cognitive interventions. The patients and their families were introduced to the etiology, causes, symptoms, treatment, and prognosis of COPD by means of multimedia lectures and the distribution of brochures, and a good patient-nurse relationship was established by using empathy and listening, and the adverse beliefs of the patients were identified through communication. Guide patients to ask questions about bad beliefs and debate with bad beliefs in a way that constantly asks questions to find reasonable solutions and correct misconceptions. When necessary, we could organize a patient meeting to encourage benign communication among patients, share treatment experience, and analyze the bias of disease and treatment perception to establish a correct disease perception.
- (ii)
Behavioral interventions (progressive breathing exercises) Relaxation training: I. Sitting relaxation involves the patient remaining seated, bending the torso forward 20°, both elbows flexed, the upper arms and shoulder joints doing circular movements, and slowly rotating the head. II. Standing relaxed, the patient stood with feet shoulder-width apart, arms naturally dropping and swinging back and forth, while the trunk rotates left and right, and the above actions were repeated 10∼15 times for one group.
- (iii)
Respiratory muscle training: I. In lip retraction training, the patient was kept in a sitting or standing position, and the physician instructed him/her to inhale through the nose and relax the abdominal muscles, followed by lip retraction and slow exhalation, ensuring that the breathing time was 4∼6 s. During the training process, a candle was placed 15–20 cm in front of the patient, and the exhalation strength was appropriate to make the flame tilt but not blow out the flame, while ensuring that the degree of lip retraction was consistent during breathing. II. In abdominal breathing, the patient maintained a lying or standing position, hands were placed on the chest and abdomen, breathing as much as possible to ensure that the chest does not move, exhale when the palm of the hand slightly forces down the abdomen, so that the abdomen retracts, and inhale when the abdomen forces up the palm of the hand. The training time was 15∼30 min, 2∼4 times/d.
- (i)
Patients’ training intensity should be adjusted according to their heart rate and respiratory rate monitoring results during exercise to avoid sports injuries. At least one caregiver should accompany the patient during the training period and take appropriate treatment measures in time if the patient becomes unwell.
2.3. Observed Indicators
2.3.1. General Information
The data were obtained by reviewing the patients’ case data, including age, gender, duration of COPD, GOLD class, education level, family and economic status, whether they had a history of smoking, and comorbidities.
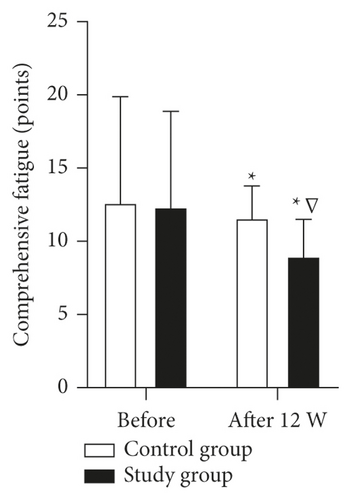
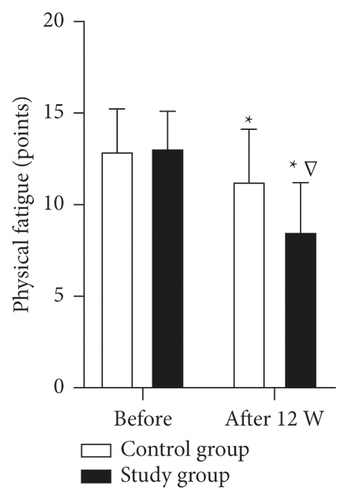
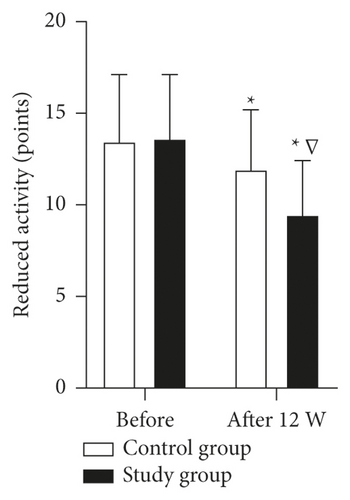
2.3.2. Fatigue Level
The Multidimensional Fatigue Inventory 20 (MFI-20) [14] was used to assess the degree of fatigue before and 12 weeks after the intervention in both groups, which included a total of 20 entries for 5 factors: general fatigue, physical fatigue, reduced activity, decreased motivation, and mental fatigue, with each factor containing 4 entries. A total score of 100 was assigned on a 5-point Likert scale (1 to 5), with higher scores indicating greater fatigue.
2.3.3. Lung Function Indicators
The percentages of forced expiratory volume one second (FEV1%), peak expiratory flow (PEF), and forced vital capacity (FVC), were compared between the two groups before and 12 weeks after the intervention. All of the above indicators were tested using the Japanese CHEST portable spirometer HI-101.
2.3.4. 6-Minute Walking Distance (6MWD)
The 6MWD was measured using a 6-minute walking test, in which the patient was asked to walk for 6 minutes at maximum speed in a quiet 30 m long corridor, and the distance walked was measured. It is important to note that the test should be terminated immediately if the patient experiences chest pain, unbearable dyspnea, lower limb cramps, pallor, or sweating during walking.
2.3.5. Coping Styles
The Medical Coping Modality Questionnaire (MCMQ) [15] was used to assess patients’ coping styles, including three dimensions of avoidance, submission, and confrontation, with a total of 20 entries, 8 of which were reverse scored, with a total score of 20 to 80, with higher scores on a dimension indicating a greater tendency for the patient to respond in that way.
2.3.6. Level of Positive Thoughts
The patients’ level of positive thinking was assessed with the Mindful Attention Awareness Scale (MAAS) [16], which included 5 dimensions of observation, description, nonjudgmental to internal experience, nonresponsiveness to internal experience, and the act of awareness, with 15 entries. A Likert 6-point scale (1 to 6) was used for scoring, with a total score of 15 to 90, and the score was positively correlated with the level of positive thinking.
2.3.7. Quality of Life
The Chinese version of the COPD Assessment Test scale (COPD Assessment Test, CAT) [17] was used to measure the patient’s quality of life. The scale contains 8 items: cough, expectoration, chest tightness, shortness of breath, ability to perform daily activities, ability to go out, sleep, and energy, and each item has a score of 0–5, with a total score of 0–40. 0–10 indicated mild, 11–20 was moderate, 21–30 was severe, and 31–40 was very severe, with higher scores indicating a more severe impact of the disease on quality of life.
2.4. Data Analysis Methods
The statistical software SPSS23.0 was used to process and analyze the collected data, and the general data such as gender and age of COPD patients were statistically described by frequency and percentage, and the χ2 test and rank sum test were used for statistical analysis. The mean and standard deviation were used to statistically describe the “MFI-20 score,” “MAAS score,” and “lung function” of COPD patients before and after the intervention, and the t-test of two independent samples was applied for comparison. Differences were statistically significant as indicated by P < 0.05.
3. Results
3.1. Comparison of Baseline Data between the Two Groups before the Intervention
Analysis of the general information of the two groups showed no statistically significant differences in gender, age, disease duration, smoking status, GOLD classification, education level, per capita monthly income, and comorbid diseases (P > 0.05) (Table 1).
| Indicator | Control group (n = 43) | Study group (n = 43) | t/χ2 value | P Value | |
|---|---|---|---|---|---|
| Gender (n, %) | Male | 27 (62.79) | 30 (69.77) | 0.468 | 0.494 |
| Female | 16 (37.21) | 13 (30.23) | |||
| Age (years; mean, SD) | 66.70 ± 4.23 | 67.16 ± 4.49 | 0.489 | 0.626 | |
| Duration of disease (years; mean, SD) | 6.84 ± 2.22 | 7.12 ± 2.42 | 0.559 | 0.578 | |
| Smoking status (n, %) | Never | 8 (18.60) | 9 (20.93) | 1.074 | 0.584 |
| Quit | 32 (74.42) | 33 (76.74) | |||
| Still smoking | 3 (6.98) | 1 (2.33) | |||
| GOLD grading (n, %) | Grade I | 5 (11.63) | 7 (16.28) | 0.392 | 0.822 |
| Grade II | 14 (32.56) | 13 (30.23) | |||
| Grade III | 24 (55.81) | 23 (53.49) | |||
| Education level (n, %) | Primary school | 17 (39.53) | 15 (34.88) | 1.525 | 0.676 |
| Junior high school | 14 (32.56) | 11 (25.58) | |||
| High school | 8 (18.60) | 10 (23.26) | |||
| College and above | 4 (9.30) | 7 (16.28) | |||
| Per capita monthly income (n, %) | <1000 yuan | 7 (16.28) | 8 (18.60) | 0.329 | 0.954 |
| 1000∼3000 yuan | 13 (30.23) | 14 (32.56) | |||
| 3001∼5000 yuan | 20 (46.51) | 19 (44.19) | |||
| >5000 yuan | 3 (6.98) | 2 (4.65) | |||
| Combined diseases (n, %) | Hypertension | 23 (53.49) | 25 (58.14) | 0.233 | 0.994 |
| Coronary heart disease | 6 (13.95) | 5 (11.63) | |||
| Cerebrovascular disease | 4 (9.30) | 4 (9.30) | |||
| Diabetes | 9 (20.93) | 8 (18.60) | |||
| Other | 1 (2.33) | 1 (2.33) | |||
3.2. Comparison of MFI-20 Scores before and after the Intervention between the Two Groups
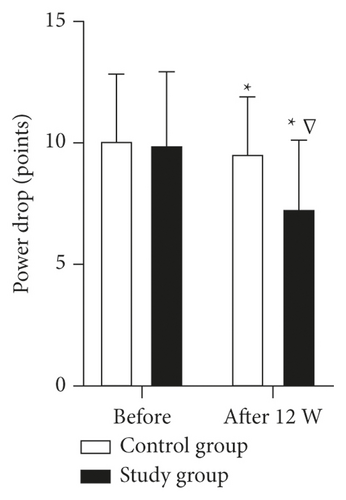
There was no statistically significant difference in the scores of comprehensive fatigue, physical fatigue, reduced activity, power drop, and mental fatigue between the two groups before the intervention (P > 0.05); the scores of comprehensive fatigue, physical fatigue, reduced activity, power drop, and mental fatigue in the study group were lower than those in the control group after 12 weeks of intervention (P < 0.05) (Figure 1).
3.3. Comparison of MCMQ Scores between the Two Groups before and after the Intervention
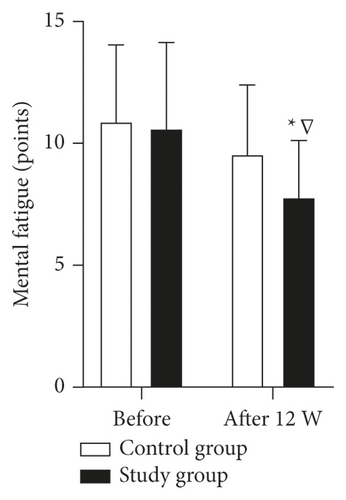
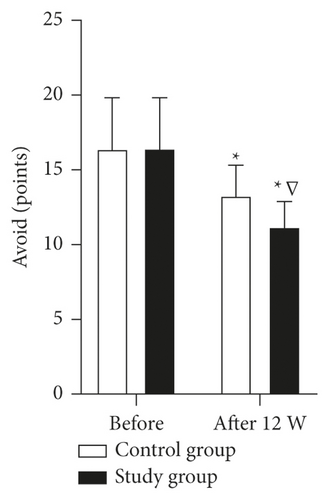
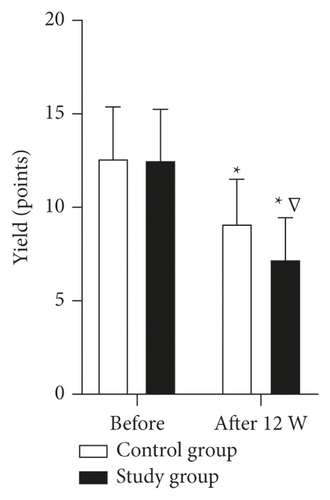
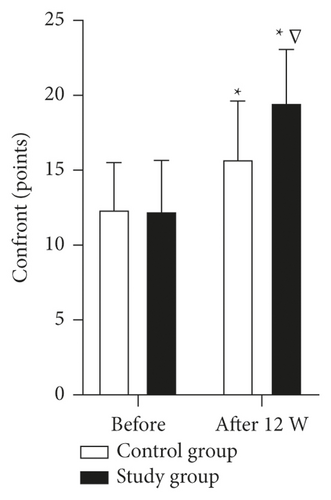
There was no statistically significant difference between the avoid, yield, and confront scores of the two groups before the intervention (P > 0.05); the avoid and yield scores of the patients in the study group were lower than those of the control group after 12 weeks of intervention, and the confront item scores were higher than those of the control group (P < 0.05) (Figure 2).
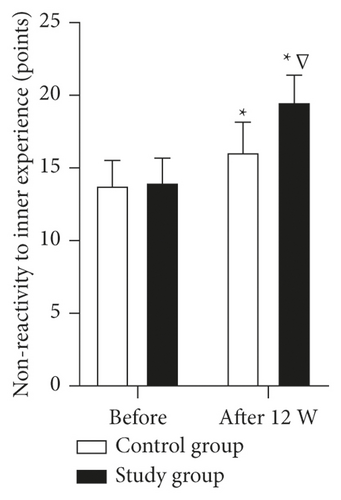
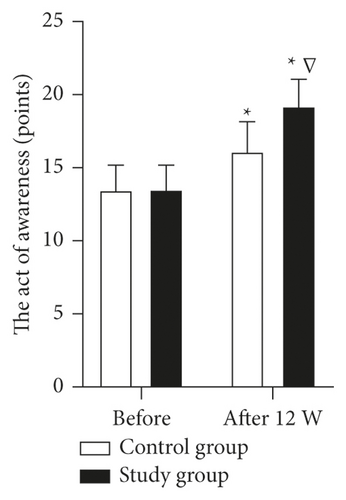
3.4. Comparison of MAAS Scores before and after the Intervention between the Two Groups
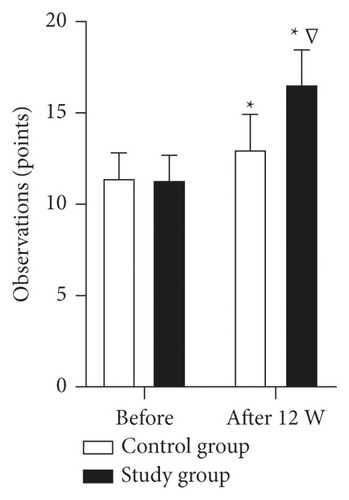
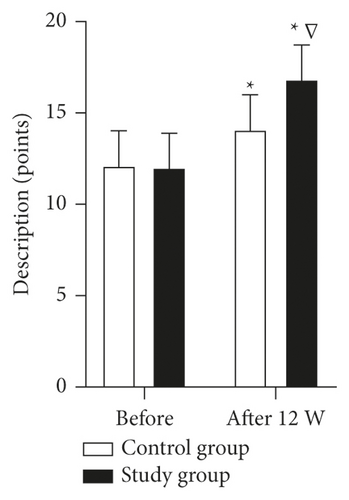
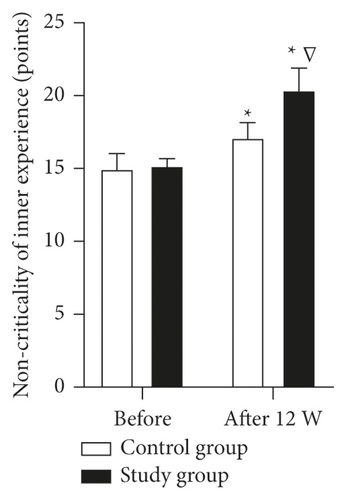
There was no statistically significant difference in the scores of observation, description, noncriticality to intrinsic experience, nonreactivity to intrinsic experience, and behavior of awareness between the two groups before the intervention (P > 0.05); the scores of observation, description, noncriticality to intrinsic experience, nonreactivity to intrinsic experience, and behavior of awareness were higher in the study group than in the control group 12 weeks after the intervention (P < 0.05) (Figure 3).
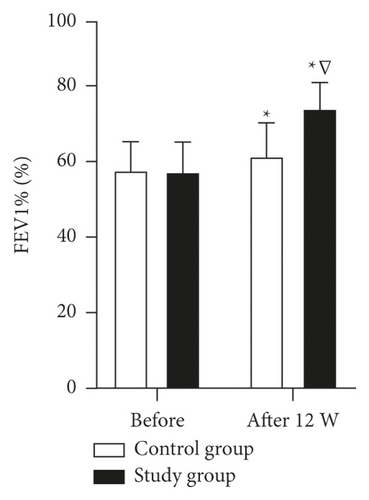
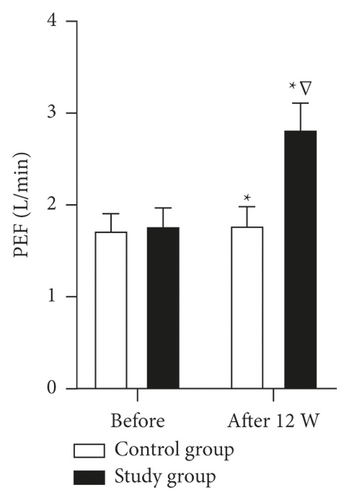
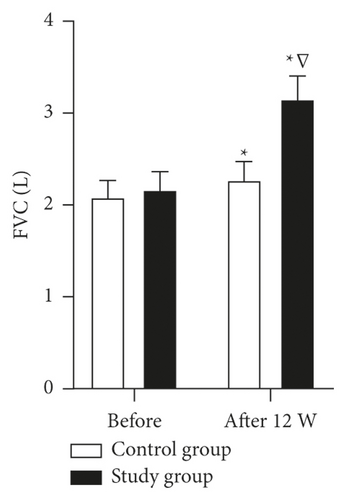
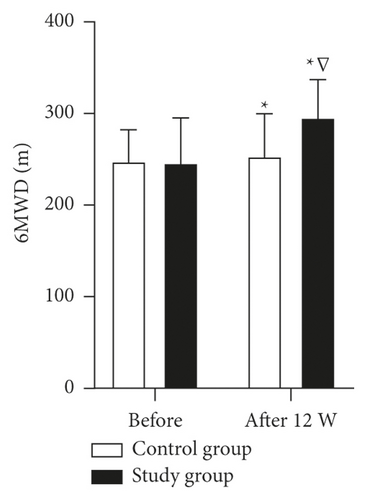
3.5. Comparison of Pulmonary Function Indexes before and after the Intervention between the Two Groups
There was no statistically significant difference between the FEV1%, PEF, FVC, and 6MWD levels of the two groups before the intervention (P > 0.05); the FEV1%, PEF, FVC, and 6MWD levels of the patients in the study group were higher than those in the control group after 12 weeks of intervention (P < 0.05) (Figure 4).
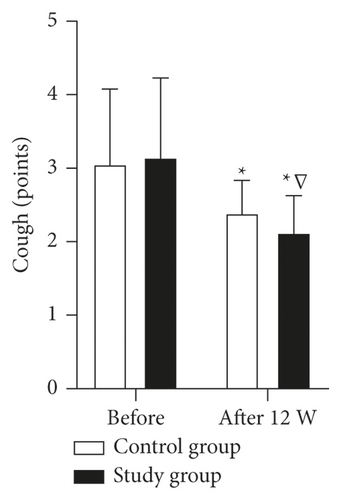
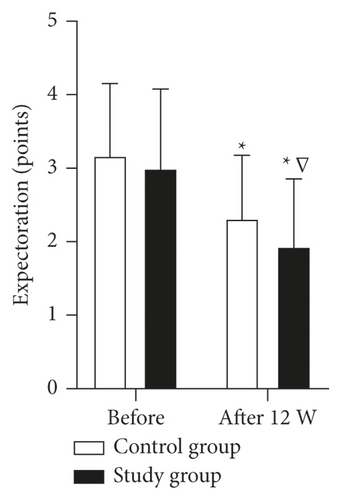
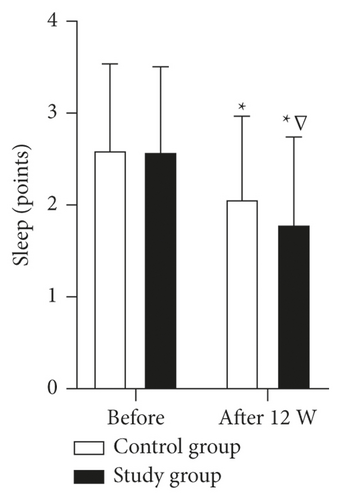
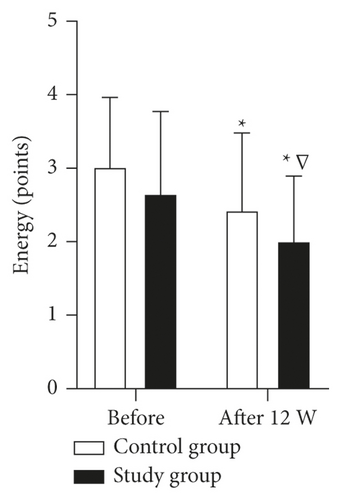
3.6. Comparison of the Quality of Life of the Two Intervention Groups
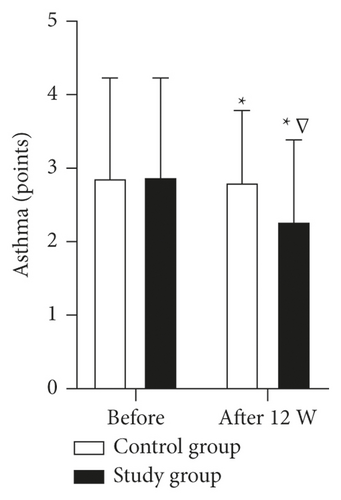
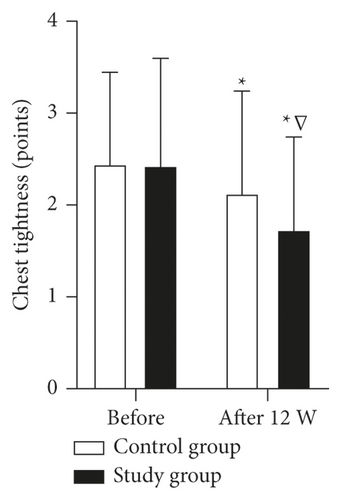
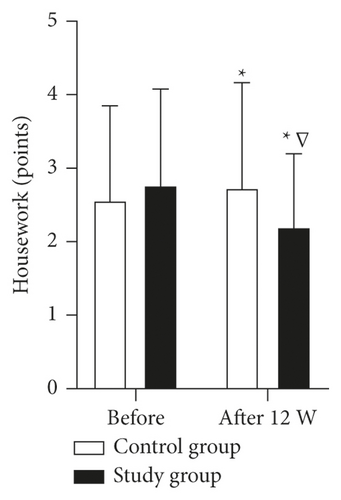
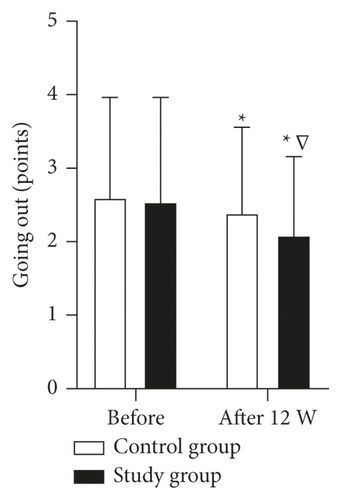
There was no statistically significant difference in the scores of cough, expectoration, asthma, chest tightness, housework, going out, sleep, and energy between the two groups before the intervention (P > 0.05); the scores of cough, expectoration, asthma, chest tightness, housework, going out, sleep, and energy in the study group were lower than those in the control group after 12 weeks of intervention (P < 0.05) (Figure 5).
4. Discussion
Patients with COPD have severe activity limitations in daily life, especially when performing exercise, due to, for example, restricted airflow, which in turn affects their quality of life [18]. Currently, exercise and respiratory training have become routine care for patients in the stable phase of COPD, but some studies [19, 20] have pointed out that routine care is more about following the treatment plan and observing the condition, while respiratory training alone tends to make patients tired, ineffective, and poorly adhered to. This shows that in addition to effective treatments to control symptoms, COPD patients should be given more behavioral guidance and psychological care during treatment and training to help them develop healthy behaviors.
Progressive respiratory training is based on the individualized situation of the patient to develop exercise prescriptions, adjust the intensity of training in stages, and complete lip retraction training, abdominal breathing, and other training, through such exercises to enhance the strength of respiratory muscles and expand the range of motion of the thorax and diaphragm, in order to effectively expand the airway, reduce resistance, and improve the quality of breathing [21, 22]. In addition, respiratory muscle training can inhibit the reduction of lung tissue elasticity caused by activity limitation, atrophy, and partial loss of function of disused respiratory muscles; improve lung ventilation and alveolar opening rate; maintain lung tissue elasticity, small airway patency, and thoracic mobility; delay the process of alveolar thickening and aging caused by inactivity; and improve the lung function of the body [23]. Mindful behavioral intervention is a psychological intervention model that helps patients to consciously maintain their attention on internal or external experiences and to self-regulate without making any judgments [24]. At present, mindfulness behavior intervention is widely used in the psychological intervention of chronic pain diseases, anxiety and depressive disorders, and cancer patients, and has achieved good results. Some studies [25] have shown that mindfulness behavior intervention can help patients develop good behavioral habits, strengthen lung function through breathing training, reasonable exercise, etc., balance sympathetic nerve activity, and enhance the quality of life. In addition, the behavioral intervention carried out health behavior guidance based on progressive breathing training, by encouraging patients to ask and answer questions and encouraging positive communication between patients and friends can strengthen their beliefs to cope with the disease and cooperate with treatment and breathing training in a good state [26].
The results of this study showed that after 12 weeks of intervention, the study group had higher levels of each score on the MFI-20 scale (comprehensive fatigue, physical fatigue, reduced activity, power drop, and mental fatigue), each score on the MAAS scale (observation, description, noncriticality to intrinsic experience, nonreactivity to intrinsic experience, and perceived behavior), FEV1%, PEF, FVC, and 6MWD than the control group. The results show that mindfulness behavior intervention combined with progressive breathing training can effectively reduce the fatigue of COPD patients, train patients’ observation ability, do not evaluate the observed things and feelings, or even accept the things and feelings, thereby enhancing patients’ awareness of stressful events, which has an important role in improving patients’ quality of life and guaranteeing physical and mental rehabilitation effects from multiple perspectives. In terms of coping style and quality of life, after 12 weeks of intervention, the study group had higher confrontation scores than the control group, lower avoid and yield scores, and each CAT scale score (cough, expectoration, asthma, chest tightness, housework, going out, sleep, and energy) than the control group. This suggests that mindful behavioral interventions combined with progressive breathing training can patiently guide patients to release processing from inertial thinking and automatic behaviors, focus on the functional state of the present moment and then face the new experience with new thinking patterns and ways, thus gradually developing a positive way of coping. In addition, the full combination of mindfulness behavior intervention and progressive breathing training can effectively adjust the psychological and physiological functions of patients and comprehensively improve the quality of life of COPD patients.
5. Summary
The results of this study showed that mindfulness behavioral intervention combined with progressive breathing training has a strengthening effect on the clinical treatment of COPD patients. Mindfulness behavioral intervention combined with progressive breathing training is simple to implement as an individual self-regulation method, which can be practiced by oneself after being familiar with certain methods and techniques, and long-term adherence helps individuals cope with the stimulation of adverse events. However, the effect of the positive behavioral intervention combined with progressive breathing training on the patient’s consolidation period was not studied in this study, and the patient’s practice will be followed up in future studies to further verify the effectiveness of the protocol.
Ethical Approval
This study was approved by the ethics committee of our hospital (EA2020024).
Conflicts of Interest
The authors declare that they have no conflicts of interest in any respect.
Open Research
Data Availability
All data in this trial are reasonably available from the authors.