Native Valve Endocarditis due to Ralstonia pickettii: A Case Report and Literature Review
Abstract
Ralstonia pickettii is a rare pathogen and even more rare in healthy individuals. Here we report a case of R. pickettii bacteremia leading to aortic valve abscess and complete heart block. To our knowledge this is the first case report of Ralstonia species causing infective endocarditis with perivalvular abscess.
1. Case Report
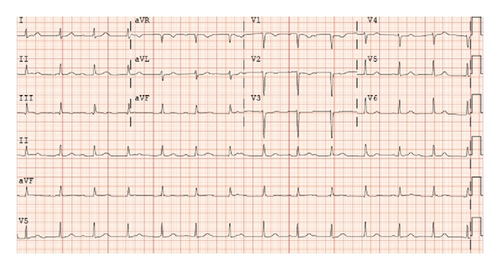
A 51-year-old female with a past medical history of deep vein thrombosis (DVT), pulmonary embolism, and well controlled diabetes mellitus type 2 (hemoglobin A1c 6.1%) presented after several days of worsening chest pain, low-grade fevers, and chills. Several weeks prior to presentation patient had a central venous catheter placed for intravenous iron infusions to treat refractory iron-deficiency anemia. Three weeks prior to presentation, the patient had left tarsal tunnel release with no postoperative complications. Upon presentation, to the hospital for evaluation she was bradycardic with a pulse of 48 beats per minute, hypotensive with a blood pressure of 106/54 mmHg (as compared to her baseline hypertension), and febrile to 101.3°C. Given her history of DVT, a computed tomography (CT) angiogram was ordered that revealed no new pulmonary emboli but showed cavitary lung lesions suggestive of septic emboli. An electrocardiogram (ECG) demonstrated accelerated junctional escape rhythm with complete atrioventricular block (Figure 1). Blood and urine cultures were obtained, and patient was initiated on empiric coverage for endocarditis with vancomycin, gentamicin, and micafungin.
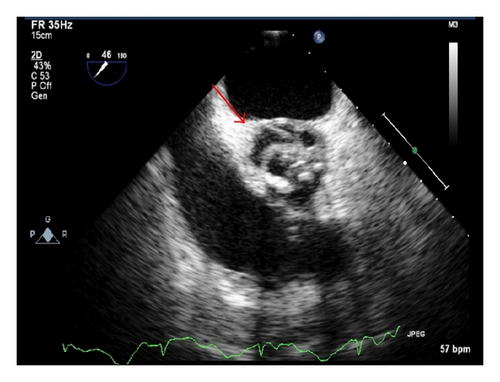
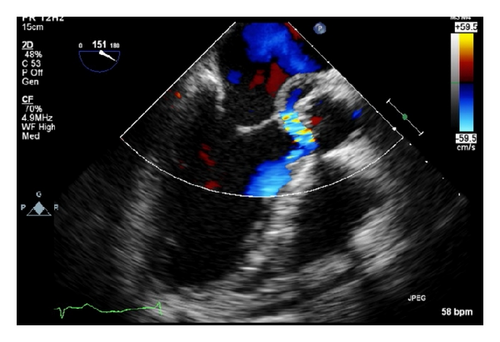
Given CT evidence of septic emboli, fevers, and ECG findings of complete AV block, an initial transthoracic echocardiogram (TTE) was performed on day two of admission, followed by a transesophageal echocardiogram (TEE) on day three of admission. TEE confirmed initial TTE findings of aortic valve thickening on the left coronary cusp highly suggestive of vegetation (Figure 2) and associated severe aortic regurgitation. Furthermore, an echo density was noted at the aortic root with color flow transmission highly suggestive of an aortic root abscess with fistula (Figure 3). There was moderate mitral valve regurgitation with normal left ventricular systolic function. A bicuspid aortic valve was also noted on the TEE. Gram-positive cocci were seen on Gram stain from blood cultures drawn on admission; therefore she was continued on vancomycin and gentamicin. The patient was referred for emergent cardiothoracic surgery with replacement of the aortic valve with a 19 mm freestyle tissue valve, incision and drainage and debridement of the subannular abscess, and reconstruction of the proximal anterior leaflet of the mitral valve and aortic annulus with pericardial patch placement which was performed at an outside hospital on day six of hospitalization. No pacemaker was placed at this time of surgery as the cardiothoracic surgeons felt that it would best be placed once her blood cultures were sterile. At the time of valve replacement a transfemoral pacer was placed.
Within 24 hours of hospitalization, blood cultures drawn on admission began growing what was initially identified as Gram-positive cocci. However, on day three of admission the Gram stain was reassessed and changed to Gram-negative rods identified as Ralstonia species. Repeat blood cultures on consecutive days up until the day of surgery grew persistent Ralstonia species, which was ultimately identified as Ralstonia pickettii. Surgical specimens from the aortic valve and annular abscess all had heavy growth of R. pickettii (surgical intervention on day 6). All postsurgical blood cultures remained negative (Table 1). She was initially on aggressive Gram-positive coverage initially with vancomycin and gentamicin; however this was quickly changed to levofloxacin once sensitivities returned. The Ralstonia species, later identified as pickettii, was sensitive to quinolones and trimethoprim-sulfamethoxazole only with intermediate sensitivity to piperacillin/tazobactam, imipenem, and cefepime and complete resistance to tobramycin amikacin and gentamycin. Her postoperative course was uneventful except for dental extractions done for extensive necrosis and caries. She was initiated on levofloxacin on day four of admission and completed a total of eight weeks of therapy postoperatively. Upon sterilization of blood cultures approximately one week after surgery, a dual-chamber pacemaker was implanted.
| DPA | Culture source | Culture result | TTP hours |
|---|---|---|---|
| 1 | Blood | + | <24 |
| 2 | Blood | + | <24 |
| 3 | Blood | + | <24 |
| 4 | Blood | + | <24 |
| 6 | Aorta | + | <24 |
| 7 | Blood | − | NA |
| 8 | Blood | − | NA |
| 9 | Blood | − | NA |
- DPA: days postadmission; TTP: time to positivity in hours.
Unfortunately, shortly after completion of the initial eight weeks of antibiotic therapy, the patient developed recurrent bacteremia with Ralstonia pickettii complicated by a periannular abscess around the new aortic valve prosthesis and a pseudoaneurysm of the ascending aorta. She was again emergently taken for repeat aortic root replacement with a 24 mm homograft and treated with aggressive antibiotic therapy with trimethoprim-sulfamethoxazole and levofloxacin (after repeat sensitivity testing). Unfortunately the patient rapidly succumbed to infection and died due to complications of persistent bacteremia.
Ralstonia species are aerobic Gram-negative, oxidase-positive, nonfermenting bacilli that have in recent years been identified as emerging opportunistic pathogens in immunocompromised hosts. Both environmental and hospital sources have been identified in human infection. Of the Ralstonia genus, Ralstonia pickettii formerly known as Burkholderia pickettii is regarded as the one with clinical importance [1]. It was first identified as Pseudomonas pickettii in 1973 [2] and then reclassified in 1992 to the Burkholderia [3] genus and finally in 1995 to a new genus Ralstonia [4–6], based upon cellular lipid and fatty acid composition, phenotypic analysis, and both DNA and 16s rRNA sequencing and hybridization. Disease associated with Ralstonia pickettii ranges from asymptomatic to septicemia and death.
2. Discussion
Historically, the first documented case of Ralstonia bacteremia and death was reported in 1968 [7]. At that time, the pathogen was reported as an unclassified, Gram-negative bacterium (Group IV d) which was only later identified as Ralstonia pickettii [8]. The case was a 33-year-old African American male who had persistent positive blood cultures with a Group IV d Gram-negative bacillus resistant to all attempted antibiotics (ampicillin, penicillin G, and chloramphenicol). Autopsy was refused; however the patient was noted to have persistent positive blood cultures, a IV/VI harsh systolic murmur at the apex transmitting to the axilla, and fevers, suggesting endocarditis due to persistent bacteremia as cause of death [7].
More recent outbreaks of Ralstonia pickettii infections are documented as nosocomial outbreaks related to the use of contaminated medical solutions (saline, sterile water, disinfectants, intravenous ranitidine, and narcotics) used in patient care [9–17]. In Table 2 we provide a comprehensive review of literature to date from 2005 onward that reflects possible contamination sources as well as outcomes. Prior to 2006 Ryan et al. provide an excellent comprehensive review [1]. The presumptive ability of Ralstonia to persist in these sterile solutions is thought to be associated with its ability to survive within a wide range of temperatures (15°C–42°C) and pass through both 0.2 and 0.45 μm filters, which are used to filter-sterilize medical solutions [18]. In a review of the literature there have been 55 cases of Ralstonia species infections, ranging from bacteremia to meningitis. The majority of infections reported have been treated with piperacillin, imipenem plus amikacin, and a combination of unnamed cephalosporins and aminoglycoside, as well as meropenem. There is no standardized recommendation for the treatment of Ralstonia infection because of the differences in sensitivities in particular to the carbapenems and aminoglycosides as well as the range of disease which includes asymptomatic to frank sepsis as in our patient. Only eight documented cases have resulted in death. The first case was the index case in 1968 as described above [7]. Two cases were elderly diabetic patients who died from complications of R. pickettii septicemia as a result of contaminated ion-exchange resins used to purify water for hospital use [19]. The ion-exchange resins used for deionization of city water allowed the survival of bacteria normally found in the city water supply while the bacteriological filters downstream only lowered the contamination level. Four premature infants have died from complications of R. pickettii-related infections. Of the four cases, one was pneumonia [20] and the other three were associated with bacteremia and sepsis [21, 22]. Finally, the eighth documented case resulting in death is our 51-year-old female who developed endocarditis due to complications of Ralstonia pickettii bacteremia with perivalvular abscess.
| Overview of Ralstonia species infections | ||||||||
|---|---|---|---|---|---|---|---|---|
| n | Age (years) | Gender | Potential offending agent | Infection | Antibiotics used | Surgery | Outcome | |
| Our case | 1 | 51 | Female | Iron infusions | Endocarditis |
|
AVR | Died |
| Graber et al. [7] | 1 | 33 | Male | IV drug abuse | Endocarditis∗ | Penicillin + chloramphenicol | None | Died |
| Poty et al. [19] | 4 | Adults | — | Ion-exchange resin | Bacteremia | — | None |
|
| Timm et al. [20] | 10 | Neonates | — | Acetic acid cleaning solution | Pneumonia | — | None |
|
| Moreira et al. [21] | 13 | Adults | — | “Sterile” water for injection | Bacteremia | Ciprofloxacin + gentamicin | None | All survived |
| 3 | Neonates | — |
|
Ampicillin + gentamicin | None |
|
||
| Vitaliti et al. [22] | 1 | 26 weeks gestation | Female | — | Bacteremia | Cephalosporin + meropenem + aminoglycoside | None | Died |
| Stelzmueller et al. [23] | 38 | Adults | — | None identified |
|
— | None | All survived |
| Forgie et al. [26] | 2 | Neonates | — | ECMO circuits | Bacteremia | Tobramycin + piperacillin-tazobactam | None |
|
| Kismet et al. [27] | 2 | Toddlers | Females | Port-A-Cath | Bacteremia | Meropenem + cefepime | Removal of Port-A-Cath | All survived |
| Kimura et al. [28] | 18 | Neonates | — | Heparin flush | Bacteremia | Piperacillin | None | All survived |
| Strateva et al. [29] | 1 | 75 | Female | Hemodialysis system | Bacteremia | Levofloxacin | None | Survived |
| Fernández et al. [11] | 46 | — | — | IV Ranitidine | Bacteremia | — | None | All survived |
| Kahan et al. [30] | 6 | — | — | 0.05% chlorhexidine | Bacteremia | — | — | — |
| Roberts et al. [10] | 19 | — | — | “Sterile” water | Bacteremia | — | — | — |
| Raveh et al. [31] | 4 | — | — | IV catheters | Bacteremia | — | — | — |
| Fujita et al. [32] | 1 | 53 | Male | IV catheter | Bacteremia | Cefazolin | None | Survived |
| Mikulska et al. [33] | 10 | — | — | None identified | Bacteremia | 3rd generation cephalosporins + amikacin or carbapenems | None |
|
| Woo et al. [34] | 1 | 7 | Male | Cord blood transplant | Bacteremia | Cefoperazone/sulbactam + ciprofloxacin | None | Survived |
| Marroni et al. [35] | 9 | Adults | — | Heparin solution | Bacteremia | — | None | All survived |
| Adiloǧlu et al. [36] | 1 | Neonate | — | Distilled incubator water | Bacteremia | — | None | Survived |
| Candoni et al. [37] | 20 | Adults | — | None identified | Bacteremia | — | None | All survived |
| Japp et al. [38] | 1 | — | — | None identified | Bacteremia | — | None | — |
| Hansen et al. [39] | 1 | — | — | IV catheter | Bacteremia | — | None | Survived |
| Chomarat et al. [40] | 1 | — | — | None identified | Bacteremia | — | — | Survived |
| Lazarus et al. [41] | 1 | Adult | — | In vitro handling process | Bacteremia | — | None | Survived |
| Marroni et al. [35] | 6 | — | — | Purified saline | Bacteremia | — | None | All survived |
| Yoneyama et al. [42] | 17 | Adults | — | 0.05% chlorhexidine aqueous solution | Bacteremia | — | None | All survived |
| Lacey and Want [9] | 7 | Children | — | “Sterile” distilled water | Bacteremia | — | None | All survived |
| Chetoui et al. [43] | 6 | Adults | — | “Sterile” saline | Bacteremia | — | None | All survived |
| Maki et al. [12] | 9 | Adults | — | Pre-drawn fentanyl syringes | Bacteremia | — | None | All survived |
| Gardner and Shulman [13] | 9 | Infants | — | Tracheal irrigant solution | Respiratory infection | — | None | All survived |
| Trotter et al. [44] | 1 | 5 | Male | None identified | Pneumonia | TMP-SMX | Decortication | Survived |
| Hagadorn et al. [45] | 1 | Neonate | — | Home water birth | Pneumonia | — | — | — |
| Miñambres et al. [46] | 1 | Adult | — | None identified | Pneumonia | — | None | Survived |
| MMWR [16] | 13 | Children |
|
0.9% sodium chloride solution |
|
— | None | All survived |
| MMWR [14] | 5 | Infants | — | 0.9% sodium chloride solution |
|
— | None | All survived |
| Labarca et al. [17] | 34 | — | — | 0.9% sodium Chloride |
|
— | None |
|
| Pan et al. [47] | 1 | 65 | Male | None identified | Pneumonia | Imipenem-cilastatin | Chest tube | Survived |
| Ahkee et al. [48] | 1 | 41 | Male | Respiratory therapy solution | Pneumonia |
|
Thoracentesis | Survived |
| Kendirli et al. [49] | 2 | 2 months | Female | Ventilator circuit |
|
Piperacillin-tazobactam | None | Survived |
| 14 | Male |
|
None | Died | ||||
| Burns et al. [50] | 2 | Adults | — | Cystic fibrosis | Respiratory infection | — | None | All survived |
| Wertheim and Markovitz [51] | 1 | 71 | Male | None identified | Osteomyelitis | TMP-SMX | Laminectomy | Survived |
| Degeorges et al. [52] | 1 | 29 | Male | None identified | Osteomyelitis | — | Debridement | Survived |
| Elsner et al. [53] | 1 | Adult | — | Hemodialysis machine | Spinal osteitis | — | — | — |
| Sudo et al. [54] | 1 | 48 | Female | None identified | Spondylitis | Cefepime + minocycline | None | Survived |
| Zellweger et al. [55] | 1 | — | Male | IV drug abuse | Septic arthritis | Ceftriaxone | — | Died |
| Makaritsis et al. [56] | 1 | 83 | Female | None identified | Septic arthritis | Ceftazidime | Arthrocentesis | Survived |
| Heagney [57] | 1 | — | — | None identified | Meningitis | — | — | — |
| T’Sjoen et al. [58] | 1 | 38 | Female | Ventriculoarterial shunt | Meningitis | — | — | — |
| Fass and Barnishan [59] | 1 | — | — | None identified | Meningitis | — | None | — |
| Yuen et al. [60] | 1 | 32 | Male | None identified | Peritonitis | Cefuroxime | Paracentesis | Survived |
| Carrell et al. [61] | 1 | — | Male | — | Seminal infection | — | None | Survived |
| Parent and Mitchell [62] | 8 | Adults | — | Crohn’s disease | Infection | — | None | All survived |
| Minah et al. [63] | — | — | — | Myelosuppressed cancer | Asymptomatic | — | — | Survived |
| McNeil et al. [15] | 5 | Infants | — | Respiratory therapy solution | Asymptomatic | — | None | All survived |
| Costas et al. [64] | 28 | Infants | — | None identified | Pseudooutbreak | — | None | All survived |
| Heard et al. [65] | 15 | Infants | — | Contaminated bottles | Pseudooutbreak | — | None | All survived |
| Dimech et al. [8] | 6 | Adults | — | Detergent disinfectant | Pseudobacteremia | — | None | All survived |
| Lacey and Want [9] | 25 | Adults | — | Blood culture technique | Pseudobacteremia | — | None | All survived |
| Boutros et al. [66] | 14 | — | — | Culture bottles | Pseudobacteremia | None | None | All survived |
| Maroye et al. [67] | 6 | Children | — | Distilled water | Asymptomatic | — | None | All survived |
| Morar et al. [68] | 1 | Child | — | None identified | Asymptomatic | — | None | Survived |
| Yoneyama et al. [42] | 7 | — | — | Water | Asymptomatic | — | None | Survived |
- ECMO: extracorporeal membrane oxygenation; IV: intravenous; AVR: aortic valve replacement; TMP-SMX: trimethoprim-sulfamethoxazole.
- ∗Presumed to have endocarditis but could not confirm diagnosis.
Immunocompromised patients seem to be at the highest risk of infection with pulmonary and blood stream infections being the primary routes [23]. Patients with acquired (i.e., HIV) or pharmaceutical (i.e., steroids, TNF blockers) induced immunosuppression are the most likely to succumb to infection with Ralstonia species. The single most important risk factor for acquiring infection with R. pickettii is cystic fibrosis. Furthermore, while respiratory tract and other nonsystemic infections responded well to parenteral antibiotic therapy, it seems to have little success in cases of R. pickettii bacteremia and sepsis, in particular, if a contaminated central venous line is involved. Removal of any indwelling device such as a central venous catheter is mandatory and critical in source control.
Interestingly, our patient had several predisposing risk factors that placed her at risk for both R. pickettii infection and complications. Approximately two months prior to presentation, our patient had a central venous catheter placed for intravenous iron transfusions. She also underwent tarsal tunnel release three weeks prior to presentation. In each of these settings she was exposed to not only potentially contaminated infusions but also hospital related procedures that may have resulted in infectious complications. Previous outbreaks have implicated hospital water, distilled water, saline, ion exchange resins, IV ranitidine, hemodialysis machines, and intravenous drug use [1]. Fortunately, our patient was an isolated case with no other cases suggesting that this was not a hospital associated outbreak. Finally, she was found to have a bicuspid aortic valve, which, in bacteremia, has been associated with increased incidence of infective endocarditis (IE) when compared to those without bicuspid aortic valves. Cases of IE occurring in patients with bicuspid aortic valves as compared to native valves have increased incidence of complications such as valve perforation, valve destruction, heart failure, and valvular, perivalvular, and/or myocardial abscess [24, 25].
Patients with health care-associated infections or who have had recent hospitalization or medical intervention (as in our case) are a new risk group that requires careful diagnostic attention in the presence of fever and bacteremia to evaluate infective endocarditis. Ralstonia pickettii should be considered an important potential etiology of nosocomial infections among patients who are immunocompromised, have cystic fibrosis, have central venous catheters, or have had recent surgical or medical hospitalizations. It is important to quickly recognize and treat R. pickettii as it has been identified as causing many potentially harmful infections resulting in increased morbidity and mortality. Ralstonia species are thought to be a rare infectious organism; however, our review of the literature suggests that the organism may be a more widespread and invasive pathogen than previously thought.
Conflict of Interests
The authors declare that there is no conflict of interests regarding the publication of this paper.