RADIOGRAPHIC AND ECHOCARDIOGRAPHIC ASSESSMENT OF LEFT ATRIAL SIZE IN 100 CATS WITH ACUTE LEFT-SIDED CONGESTIVE HEART FAILURE
Presented at the Annual Forum of the American College of Veterinary Internal Medicine, Seattle/WA, June 12–15, 2013.
Abstract
The aims of this study were to evaluate left atrial size in cats with acute left-sided congestive heart failure. We hypothesized that left atrial size as determined by thoracic radiography can be normal in cats with acute left-sided congestive heart failure. One hundred cats with acute left-sided congestive heart failure in which thoracic radiography and echocardiography were performed within 12 h were identified. Left atrial size was evaluated using right lateral and ventrodorsal radiographs. Measurements were compared to two-dimensional echocardiographic variables of left atrial size and left ventricular size. On echocardiography, left atrial enlargement was observed in 96% cats (subjective assessment) whereas maximum left atrial dimension was increased (>15.7 mm) in 93% cats. On radiographs left atrial enlargement (subjective assessment) was found in 48% (lateral view), 53% (ventrodorsal view), and 64% (any view) of cats whereas left atrial enlargement was absent in 36% of cats in both views. Agreement between both methods of left atrial size estimation was poor (Cohen's kappa 0.17). Receiver operating characteristic curve analysis identified a maximum echocardiographic left atrial dimension of approximately 20 mm as the best compromise (Youden index) between sensitivity and specificity in the prediction of radiographic left atrial enlargement.
Left atrial enlargement as assessed by thoracic radiography may be absent in a clinically relevant number of cats with congestive heart failure. Therefore, normal left atrial size on thoracic radiographs does not rule out presence of left-sided congestive heart failure in cats with clinical signs of respiratory distress.
Introduction
Left-sided congestive heart failure is a common clinical syndrome and most often secondary to cardiomyopathy in cats.1-4 Due to its high mortality,3 early diagnosis and immediate effective treatment are of crucial importance for survival. The diagnosis of congestive heart failure is primarily based on history and physical examination findings but may be confounded by conditions causing similar clinical signs.3, 4 Thoracic radiography is the standard diagnostic method in the confirmation of suspected congestive heart failure.2, 3 However, concurrent respiratory disease, heart worm disease, presence of noncardiogenic pleural effusion, prior treatment with diuretics, technical factors related to the difficulty of generating high-quality images in distressed cats, or pathophysiologic phenomena seen relatively often in cats including pronounced venous constriction with heart failure leading to disappearance of pulmonary venous engorgement all may make interpretation of radiographs with regard to the diagnosis of cardiogenic pulmonary infiltrates challenging.2, 4 Moreover, there are differences in appearance and location of cardiogenic pulmonary edema between dogs and cats2, 3 contributing to possible difficulties unequivocally diagnosing left-sided congestive heart failure in cats. Valued as incremental evidence of left-sided congestive heart failure under such circumstances is assessment of left atrial size. If enlarged and respiratory distress present, congestive heart failure is very likely,1, 4 and some authors even conclude that in cats with respiratory distress and absence of left atrial enlargement, left-sided congestive heart failure is definitively ruled out.5 However, to the author's knowledge the latter view is not substantiated by any published evidence. In addition, if left-sided heart failure is missed due to the absence of left atrial enlargement, successful therapies may be delayed or not instituted at all possibly leading to increased mortality.7 Therefore, the objective of this study was to assess left atrial size in cats with left-sided congestive heart failure. We hypothesized that left atrial size as assessed by thoracic radiography can be normal in cats with acute left-sided congestive heart failure.
Materials and Methods
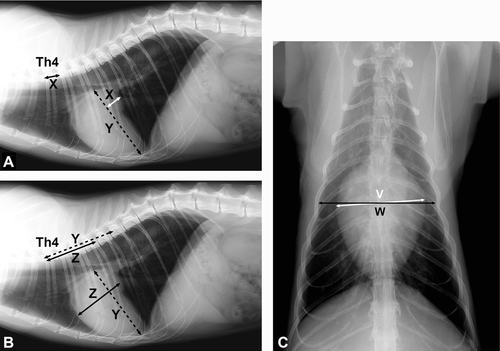
Consecutive cats with acute left-sided congestive heart failure were identified by searching the medical record data base of the Veterinary Medical Center at The Ohio State University from 2003 to 2012 in this retrospective case series. Inclusion criteria were unequivocal diagnosis of left-sided congestive heart failure with acute onset based on historical and clinical findings (e.g., tachypnea, labored breathing, and respiratory distress), thoracic radiography (e.g., interstitial and alveolar infiltrates suggestive of cardiogenic pulmonary edema and/or pleural effusion; Fig. 1),2, 3 and response to diuretic treatment leading to alleviation of clinical signs. Radiographs were identified by one investigator (E.W.), and presence of findings suggestive of left-sided congestive heart failure2, 3 on radiographs was verified collectively by a board-certified radiologist (W.T.D.) and board-certified cardiologist (K.E.S.) each with more than 15 years of experience in their respective field and blinded to other quantitative diagnostic data. Radiographic images had to be made within 12 h of onset of clinical signs, be of sufficient quality (e.g., positioning, exposure, and phase of respiration) to allow for assessment of target variables, and had to be accompanied by an echocardiographic study consistently done within 12 h after thoracic radiography. Prior administration of diuretics was not an exclusion criterion. However, if treated orally only a low dose of furosemide (once a day to once every other day dosing) was permitted. If furosemide was administered parenterally, such treatment was only permitted if performed within 12 h of imaging. After assurance of high-quality digital radiographs (Sedecal™, Sedecal USA, Arlington Heights, IL or Prestige II, GE Medical Systems, Milwaukee, WI; digital radiography system EDR-6, Sound-Eklin, Carlsbad, CA; viewing software E-film, Merge Healthcare, Milwaukee, WI), presence of congestive heart failure (subjective assessment based on the presence of pulmonary vessel engorgement and/or pleural effusion and pulmonary infiltrates suggestive of cardiogenic cause; yes/no), cardiomegaly (subjective assessment; yes/no), left atrial enlargement (subjective assessment; yes/no), pulmonary vein enlargement (subjective assessment; yes/no), pulmonary artery enlargement (subjective assessment; yes/no), vertebral heart scale6 from right lateral images, and cardiothoracic ratio7, 8 from ventrodorsal images were determined. Decisions about the qualitative variables were made by the two board-certified observers in one continuous session and with the studies in random order whereas quantitative variables were measured by a different observer (E.W) blinded to prior assessments. The use of the diagnostic term “equivocal” was not permitted for qualitative assessment; both observers had to come to a collective conclusion about the presence (yes) or absence (no) of a certain qualitative characteristic. The vertebral heart scale6 and cardiothoracic ratio8 were measured (Fig. 2) and reference values published were used in the diagnosis of cardiomegaly (>8.16 for vertebral heart scale and >0.778 for cardiothoracic ratio) corresponding to values beyond the mean plus two standard deviations as found in normal cats. Increased left atrial size was diagnosed from right lateral images as unequivocal bulging of the dilated left atrium extending caudo-dorsally. Pure dorsal ventral elongation of the cardiac silhouette without caudal dorsal bulging was not considered specific of left atrial enlargement.9 On ventrodorsal radiographs, increased size of the left atrium and the left auricular appendage was diagnosed as bulging of the left heart border visible at the 1:30 o'clock to 3 o'clock position, using the clock-face analogy.9 Left atrial size was further quantified by applying a recently introduced vertebral heart scale system for left atrial measurements in cats (Fig. 2).10 Cats were deemed to have left atrial enlargement if left atrial vertebral heart scale was >1.30.10

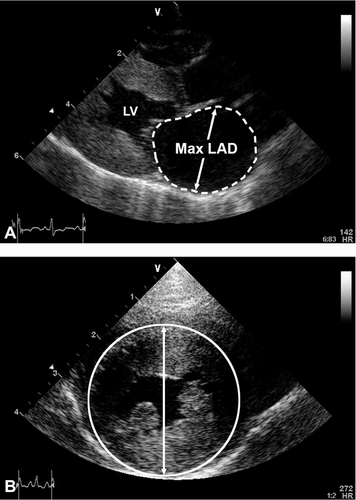
Comprehensive transthoracic two-dimensional (2-D), time motion mode, and Doppler echocardiographic studies were performed in all cats (Vivid 7 Vantage™ with EchoPac software package version BT06, GE Medical Systems, Milwaukee, WI) with the animals in lateral recumbency using imaging views and measurement methods as previously described.10, 11 All quantitative echocardiographic variables were remeasured from previously recorded examinations by one investigator (E.W.) whereas subjective assessment of left atrial size was done by a board-certified cardiologist (K.E.S.) blinded to the results of thoracic radiography. The target variable, left atrial size, was assessed from a right parasternal long-axis imaging view (Fig. 3A) and included subjective data (left atrial enlargement; yes/no) and objective data (maximum left atrial antero-posterior dimension and maximum left atrial area acquired from the same image)10 measured at end-systole. These data were used as gold standard for comparison to radiographic variables of left atrial size. Left atrial enlargement was echocardiographically defined as a maximum left atrial dimension >15.7 mm10 or 16.5 mm1 and a maximum left atrial area >2.76 cm2.10 Left ventricular size was quantified from standard right parasternal short-axis images using left ventricular total dimension (epicardium to epicardium) and area (Fig. 3B) measured at end-diastole.11 Intra- and interobserver measurement variability of selected quantitative radiographic and echocardiographic variables was assessed using 20 randomly selected studies and performing five repeated analyses of the same variables from the same images by two observers in a blinded fashion.
Statistical Analysis
Analyses were done with commercially available software (Prism 4, Graph Pad Software, Inc., San Diego, CA and Sigma Stat for Windows Version 3.5, Systat Software, Inc., San Jose, CA). Data were tabulated and graphically inspected for plausibility. Observer variation was calculated using the formula: Coefficient of variation = mean difference/average × 100 and expressed in percent.12 Normality of data was evaluated by the Kolmogorov–Smirnov test. Accuracy of data in the prediction of left-sided congestive heart failure was reported as frequency data and validated by echocardiographic measures of left atrial size. Chi-square tests or Fisher's exact tests were performed for comparison of qualitative variables, and nonpaired t-tests were used for quantitative data comparison. Receiver operating characteristic curve analysis was used to identify the optimal diagnostic cutoff of echocardiographic maximum left atrial dimension in the prediction of left atrial enlargement on thoracic radiographs, and values leading to 100% diagnostic sensitivity, 100% diagnostic specificity, and the optimal combination of such variables (Youden Index J = [Sensitivity + Specificity] − 100) with +100 being the best and −100 being the worst were determined.13 Likewise, the area under the receiver operating characteristic curve was used as a summary measure for diagnostic accuracy to predict radiographic left atrial enlargement14 from maximum left atrial dimension. Cohen's kappa analysis was performed to estimate agreement between echocardiographic (maximum left atrial dimension) and radiographic (subjective left atrial enlargement) methods.15 Linear regression analysis was done to identify associations between echocardiographic and radiographic variables of cardiac chamber size. A P-value < 0.05 was considered significant.
Results
One hundred consecutive cats with unequivocal acute left-sided congestive heart failure that fulfilled the inclusion criteria were entered into the study. Mean (standard deviation) age was 8.1 (4.8) years (minimum to maximum, 0.3–19) and mean body weight was 5.14 (1.51) kg (1.6–9.45). Twenty-eight cats were female (27 spayed and one intact) and 72 cats were male (70 neutered and two intact). Cats were from 13 different breeds with domestic shorthair cats (n = 72) and domestic longhair cats (n = 9) being most frequent. Three each were Himalayan, Maine Coon, and Siamese; two each were Ragdoll and Russian Blue; and there were three additional breeds with one cat each. Primary diagnoses included hypertrophic cardiomyopathy (n = 62), unclassified cardiomyopathy (n = 7), congenital heart disease expected to cause left-sided volume overload and leading to congestive heart failure (n = 7), restrictive cardiomyopathy (n = 6), dilated cardiomyopathy (n = 6), chronic renal failure with systemic hypertension (n = 4), hyperthyroidism (n = 3), chronic anemia (n = 2), bacterial endocarditis (n = 1), and diabetes mellitus with complete atrioventricular block (n = 1). In one cat, no underlying or concurrent disease was identified. In 36 cats that were previously stable different potential triggers for decompensation were identified including parenteral fluid administration (n = 14) or blood transfusion (n = 1), acute arterial thromboembolism (n = 12), parenteral depot corticosteroid administration (n = 7), anesthesia (n = 1), and a possible myocardial infarct (n = 1) as suspected based on the echocardiographic finding of regional left ventricular wall motion abnormality and a serum cardiac troponin I concentration of 48.77 ng/mL (laboratory reference, <0.20) in a cat with hypertrophic cardiomyopathy. A total of 43 cats had received prior treatment with furosemide whereas 57 cats had not. Of those treated, 31 had received parenteral furosemide within 12 h of imaging whereas 12 had received oral furosemide (once a day to every other day dosing at 0.5–1 mg/kg) for at least one week prior to the onset of acute left-sided congestive heart failure. Thirty-two cats received a single IV or IM injection of furosemide during the first 12 h of admission at doses between 0.5 mg/kg (n = 3), 1 mg/kg (n = 14), 1.5 mg/kg (n = 4), and 2 mg/kg (n = 11); two cats a bolus of 1 mg/kg IV followed by constant rate infusion (0.5 mg/h), three cats two bolus injections at 0.5–2.0 mg/kg IV, and another three cats three bolus injections of furosemide at 1–1.5 mg/kg IV. Respiratory rate at initial physical exam was 66 (31) breaths per minute (minimum to maximum, 20–180) in 94 cats. In 21 cats, respiratory rate was ≤40 breaths per minute. Nine cats had open mouth breathing at initial exam. Respiratory rate could not be determined in six cats due to either purring (n = 3) or absence of data entry into the medical record (n = 3).
Results of thoracic radiography and 2-D echocardiography are summarized in Table 1. Radiographic findings suggestive of cardiogenic pulmonary edema were present in 95 cats while five cats had pleural effusion only in the absence of pulmonary infiltrates suggestive of cardiogenic pulmonary edema. Pleural effusion was present in another 46 cats. Of 96 sets of radiographic images available for subjective assessment of pulmonary vessels, 49 showed pulmonary venous enlargement (lobar pulmonary vein dimension wider than that of accompanying pulmonary artery and/or lobar pulmonary vein dimension wider than the smallest dimension of the third rib) whereas 47 did not. In the same sets of radiographs, pulmonary artery enlargement (lobar pulmonary artery dimension wider than that of the accompanying pulmonary vein) was identified in 65 whereas it was not in 31.
| Imaging mode | Variable | N | Diagnostic cutoff | Yes | No |
|---|---|---|---|---|---|
| Radiography | Pulmonary vein enlargement | 96 | Subjective | 49 | 47 |
| Pulmonary artery enlargement | 96 | Subjective | 65 | 31 | |
| Pulmonary edema | 100 | Subjective | 95 | 5 | |
| Pleural effusion | 100 | Subjective | 51 | 49 | |
| Cardiomegaly | 100 | Subjective | 96 | 4 | |
| Vertebral heart scale (v) | 97 | ≥8.16 | 87 | 10 | |
| Cardiothoracic ratio | 96 | 0.778 | 43 | 53 | |
| Left atrial enlargement (lat) | 100 | Subjective | 48 | 52 | |
| Left atrial enlargement (v/d) | 100 | Subjective | 53 | 47 | |
| Left atrial enlargement (both lat and v/d) | 100 | Subjective | 36 | 64 | |
| Left atrial enlargement (either lat or v/d) | 100 | Subjective | 28 | 72 | |
| Absence of left atrial enlargement (both lat and v/d) | 100 | Subjective | 36 | 64 | |
| Left atrial VHS (v) | 97 | 1.3010 | 7 | 90 | |
| Echocardiography | Left atrial enlargement | 100 | Subjective | 96 | 4 |
| Maximum left atrial dimension (mm) | 100 | 15.710 | 93 | 7 | |
| Maximum left atrial dimension (mm) | 100 | 16.51 | 81 | 19 | |
| Maximum left atrial area (cm2) | 100 | 2.7610 | 80 | 20 | |
| Maximum left ventricular outer area (cm2) | 100 | 6.6510 | 74 | 26 |
- v, vertebral bodies; lat, lateral projection; v/d, ventrodorsal projection. Maximum left ventricular outer area, maximum left ventricular area including the myocardium (area under entire epicardial circumference). Superscript letters refer to references from which diagnostic cutoffs were acquired.
On echocardiography, mean (standard deviation) maximum left atria dimension was 19.8 mm (3.6; minimum to maximum, 11–31.8). Using 15.7 mm as the diagnostic cutoff,10 left atrial enlargement was found in 93 cats. Using 16.5 mm as the diagnostic cutoff,1 81 cats had left atrial enlargement. Mean maximum left atrial area was 3.89 cm2 (1.29; minimum to maximum, 1.38–8.02). Using 2.76 cm2 as the diagnostic cutoff,10 80 cats had left atrial enlargement. Five of six cats with a maximum left atrial dimension <15.7 mm had also a maximum left atrial area <2.76 cm2. In 23 cats mild pericardial effusion was found. The vertebral heart scale and left atrial vertebral heart scale could only be quantified in 97 cats. In two sets of radiographs provided by the referring veterinarian, vertebral heart scale was not measured due to improper position of the cats. In one cat, vertebral heart scale was not measured due to severe pleural effusion. Mean vertebral heart scale was 8.9 vertebral bodies (v; 0.8; minimum to maximum, 6.6–10.8). Using 8.1 v as the diagnostic cutoff,6 90% of cats had cardiac enlargement. In 23 cats, vertebral heart scale was >9.3 v. Radiographic left atrial enlargement was observed in 48 cats using subjective assessment and lateral projections, whereas left atrial enlargement was found in 53 cats using ventrodorsal projections. In 36 cats, both lateral and ventrodorsal projections indicated presence of left atrial enlargement. In another 36 cats, left atrial enlargement was absent in either view. In 28 cats, left atrial enlargement was either detected in the lateral projection (n = 11) or the ventrodorsal projection (n = 17). Cohen's kappa coefficient used to quantify agreement between both echocardiographic and radiographic methods of left atrial size estimation was 0.17. Cats with absent left atrial enlargement on orthogonal sets of thoracic radiographs had smaller echocardiographic left atrial size compared to cats in which left atrial enlargement was observed in either one or both radiographic views (maximum left atrial dimension 17.87 ± 3.11 mm vs. 20.84 ± 3.37 mm and maximum left atrial area 3.23 ± 1.01 cm2 vs. 4.26 ± 1.29 cm2). Cats with absent left atrial enlargement had similar proportions of underlying diseases as compared to cats with evidence of left atrial enlargement (all P > 0.05), and there was no difference between both groups regarding frequency of trigger events of acute left-sided congestive heart failure (37% vs. 35%, P = 0.921). Sixteen (44%) of the 36 cats without demonstrable left atrial enlargement on thoracic radiographs were pretreated with furosemide whereas 20 (56%) were not. The cardiothoracic ratio was not measured in four cats due to either improper position or pleural effusion making clear identification of the cardiac silhouette impossible. Using a diagnostic cutoff for he cardiothoracic ratio of 0.77,8 43 cats had cardiomegaly.
Results of the receiver operating characteristic curve analysis in the radiographic prediction of left atrial size are summarized in Table 2. Using single or multiple radiographic imaging views lead to identification of an echocardiographic maximum left atrial dimension of approximately 20 mm at or beyond which left atrial enlargement can be observed on thoracic radiography with an optimal combined sensitivity and specificity of approximately 60–70%. An echocardiographic maximum left atrial dimension around 25 mm was visible on thoracic radiographs as left atrial enlargement with 100% specificity but low sensitivity (<20%). Using these thresholds, a maximum left atrial dimension ≥20 mm (n = 49) was seen as left atrial enlargement on lateral or ventrodorsal radiographs in 59% and 65% cats and a maximum left atrial dimension ≥25 mm (n = 10) in 92% and 88% cats, with no difference in proportions between radiographic views (P = 0.582 and 0.651), respectively. Univariate linear regression analysis identified associations between maximum left atrial dimension and maximum left atrial area (r = 0.89; P < 0.001), maximum left atrial dimension and left atrial vertebral heat scale (r = 0.41; P < 0.001), vertebral heart scale and cardiothoracic ratio (r = 0.39; P < 0.001), maximum left ventricular dimension and vertebral heart scale (r = 0.21; P = 0.038), maximum left ventricular area and vertebral heart scale (r = 0.22; P = 0.032), vertebral heart scale and left atrial vertebral heart scale (r = 0.51; P < 0.001), maximum left ventricular dimension and maximum left ventricular area (r = 0.86; P < 0.001), and vertebral heart scale and maximum left atrial dimension (r = 0.382; P < 0.001). Coefficients of variation for intra- and interobserver variability of measurements (Table 3) ranged between 2.9% (maximum left atrial dimension) and 17.6% (left atrial vertebral heart scale).
| Left atrial enlargement (thoracic radiography) | AUC | Max LAD (mm) cutoff | Se (%) | Sp (%) | Youden index | P |
|---|---|---|---|---|---|---|
| On lat projection only | 0.71 | 13.0 | 100 | 4 | ||
| 24.3 | 20 | 100 | ||||
| 19.6 | 70 | 60 | 30 | <0.001 | ||
| On vd projection only | 0.68 | 13.0 | 100 | 4 | ||
| 24.5 | 11 | 100 | ||||
| 19.6 | 68 | 65 | 33 | 0.002 | ||
| On either lat OR vd projection | 0.73 | 13.1 | 100 | 6 | ||
| 24.3 | 16 | 100 | ||||
| 19.9 | 64 | 74 | 38 | <0.001 | ||
| On lat AND vd projection | 0.69 | 13.0 | 100 | 3 | ||
| 25.7 | 6 | 100 | ||||
| 19.6 | 72 | 58 | 30 | 0.002 |
- ROC, receiver operating characteristic; AUC, area under the ROC curve; Max LAD, maximum left atrial dimension; Se, sensitivity; Sp, specificity; lat, lateral projection; v/d, ventrodorsal projection. The bold numbers present the ones indicating best diagnostic accuracy of the appropriate test.
| Variable | Intra-OV | Inter-OV |
|---|---|---|
| Maximum left atrial dimension | 2.9 | 7.7 |
| Maximum left atrial area | 4.8 | 12.3 |
| Maximum left ventricular dimension (epicardium-to-epicardium) | 2.6 | 2.9 |
| Maximum left ventricular area (area under entire epicardial circumference) | 4.9 | 10.2 |
| Vertebral heart scale | 2.5 | 5.3 |
| Left atrial vertebral heart scale | 9.7 | 17.6 |
| Cardiothoracic ratio | 4.2 | 3.7 |
- OV, observer measurement variability.
Discussion
The major findings of this study are that (1) left atrial enlargement as assessed by thoracic radiography can be absent in a relevant number of cats with left-sided congestive heart failure independent of the underlying disease etiology and despite the fact that almost all cats with left-sided congestive heart failure have left atrial enlargement on 2-D echocardiography, (2) pulmonary venous enlargement is a poor indicator of left-sided congestive heart failure in cats with pulmonary arteries more often enlarged as compared to pulmonary veins, and (3) cardiomegaly is a consistent finding in cats with left-sided congestive heart failure making radiographic assessment of heart size diagnostically more important than evaluation of left atrial size in cats with respiratory distress.
The presence of congestive heart failure in cats is suspected based upon a pattern of historical and clinical findings including but not limited to restlessness, anorexia, hiding, and respiratory abnormalities such as tachypnea and labored breathing. The combination of such findings with a heart murmur or a gallop sound, a cardiac arrhythmia, pulmonary crackles, and jugular vein distension leads to a considerable increase in pretest probability of congestive heart failure. However, although respiratory distress is highly sensitive of congestive heart failure, it lacks specificity as primary respiratory disease, metabolic abnormalities, or severe pain may cause similar clinical signs. Currently, thoracic radiography is the clinical gold standard in the diagnosis of decompensated heart failure in cats. Findings such as cardiomegaly,4, 9, 16 left atrial enlargement,1, 2, 5 diffuse or focal reticular or granular interstitial infiltrates,2 an alveolar lung pattern with air bronchograms,2, 9 enlargement of pulmonary vessels2, 9, 17 with or without a bronchial pattern,2 and pleural effusion2, 3, 9 have all been reported in cats with congestive heart failure. However, the radiographic appearance of left-sided congestive heart failure in cats is more variable than in dogs,2 and cats with congestive heart failure frequently develop pleural effusion that may complicate radiographic assessment. 2
Whereas decompensated left heart disease in dogs is almost universally associated with increased left atrial size18 and the radiographic characteristics of left atrial enlargement such as a prominent waist or notch in the caudal cardiac border between the atrium and ventricle with dorsal displacement of the trachea and more specifically the left mainstem bronchus are commonly found, the same may not be true in cats.9, 16 Cats with left-sided heart disease often develop left ventricular enlargement seen on radiographs as an elongated cardiac silhouette and increased convexity of the left ventricular border in both orthogonal projections. Although left ventricular enlargement is often associated with left atrial enlargement, signs of left ventricular elongation do not unequivocally differentiate between left atrial and left ventricular enlargement,4, 9 and left ventricular enlargement with normal left atrial size has been reported in cats with advanced heart disease.1, 4, 11 The results of this study confirm that clear evidence of left atrial enlargement, although found on 2-D echocardiography in the vast majority of cats, can be absent on thoracic radiographs in many cats with acute left-sided congestive heart failure. More than one-third of cats did not reveal specific radiographic signs of left atrial enlargement. Similar to our findings, left atrial dimension as determined by 2-D echocardiography was increased in most cats with congestive heart failure using a diagnostic cutoff of 16.5 mm1 in another study leading to high diagnostic accuracy to distinguish cats with congestive heart failure from cats with primary respiratory disease using echocardiographic methods, with only 10% of cats misclassified.1 Unfortunately, in the latter1 only a low number of cats underwent thoracic radiography making comparison of studies with regard to the diagnostic accuracy of thoracic radiography impossible. In a study of 21 cats with cardiogenic pulmonary edema seen in a first opinion veterinary practice,2 all cats had left atrial enlargement on 2-D echocardiography with a mean vertebral heart score and mean maximum left atrial dimension larger as compared to our study (9.6 vertebrae vs. 8.9 vertebrae and 21 mm vs. 19.8 mm, respectively), probably indicating more advanced disease in the former.2 However, only 11 of the 21 cats (52%) had a definitive left atrial bulge indicating left atrial enlargement, a proportion similar to what was found in our study.
Once moderate to severe left atrial dilatation develops the likelihood of finding specific evidence of left atrial enlargement on radiographs seems to increase. We identified a clinically-useful decision threshold of approximately 20 mm for maximum left atrial dimension, considered by many veterinary cardiologists as moderate left atrial enlargement, to have a 60–70% sensitivity and specificity for correctly identifying left atrial dilatation on thoracic radiographs. Once maximum left atrial dimension is around 25 mm, left atrial enlargement is seen on radiographs with 100% Sp. These numbers seem to have clinical and possibly therapeutic relevance. Although arbitrary, many veterinarians treat cats with heart disease with a platelet inhibitor with the intention to prevent or delay feline arterial thromboembolic disease.19 Increased left atrial size is one key variable that might trigger the initiation of such treatment,19, 20 and the threshold of maximum left atrial dimension that seems to be used often in decision making is centered around 20 mm. That is, if left atrial enlargement is seen on thoracic radiographs, one would expect that echocardiographic maximum left atrial dimension is 20 mm or larger in most of such cats, justifying administration of antiplatelet drugs even without a prior echocardiogram. Although the latter approach has not yet been substantiated by a prospective study the approach appears appealing and deserves further investigation. Moreover, moderate to severe left atrial enlargement is likely associated with moderate to severe dilatation of the left auricle, a cardiac structure not commonly identified on lateral radiographs. On ventrodorsal radiographs, the enlarged left auricular appendage will only be seen if moderately to severely enlarged with its lateral border becoming border-forming at the 1:30 o'clock to 3 o'clock position as found in our study. The majority of cats with moderate and severe left atrial enlargement on echocardiography (65% of cats with a maximum left atrial dimension ≥20 mm and 88% of cats with a maximum left atrial dimension ≥25 mm) had evidence on left atrial enlargement on lateral or ventrodorsal radiographs, respectively.
More quantitative radiographic variables of left atrial size have recently been evaluated in cats with heart disease10, 16 to overcome subjectivity of the assessment of which left atrial vertebral heart scale obtained from lateral radiographic images10 was used in this study. The distance from the center of the seventh vertebral body to the leftward edge of the cardiac silhouette in the dorsoventral projection was used as a potential measure specific to the left atrium in another study of 24 cats.16 However, both variables were of little value in predicting echocardiographic left atrial size with coefficients of determination (r2) between variables below 0.20 rendering both of limited incremental value in the diagnosis of left atrial enlargement.
As in other feline studies,4, 16 the cardiac silhouette was enlarged in almost all cats with acute left-sided congestive heart failure. This finding is not unexpected and likely owing to the fact that volume overload is integral part in the pathophysiology of congestive heart failure and that the cardiac silhouette represents the summation of four cardiac chambers including the myocardium, the great vessels of the heart base, and the pericardial space, structures that are all influenced by increased preload. From the results of this and other studies,4, 16 it seems that the combination clinical signs of congestive heart failure, pulmonary infiltrates, and radiographic cardiomegaly are the best combined predictor of congestive heart failure, whether or not left atrial size is visibly increased.
Only approximately one-half of the cats with acute left-sided congestive heart failure had pulmonary vein dilatation and about two-thirds of cats had pulmonary artery enlargement as assessed subjectively or semiquantitatively, proportions that were rather unexpected. In cats as well as in dogs with congestive heart failure, one would anticipate at least pulmonary vein enlargement in the majority of animals owing to the pathophysiology of congestive heart failure where fluid retention leading to increased preload is a central part. However, the presence of pleural effusion as found in 51% cats may have led to partially collapsed lung lobes obscuring of pulmonary vessels and preventing observers from proper identification of such anatomic structures.2 Moreover, prior treatment with furosemide as done in 43% cats may have led to acute changes of central hemodynamics suddenly reducing preload and left ventricular filling pressures and thus the size of the pulmonary veins. In addition, it is well known from studies in people21, 22 that systemic veins contain a large number of α1 and α2 adrenergic receptors making them highly sensitive to stimulation by the sympathetic nervous system. Compared to arteries, veins contain more than five times the density of adrenergic nerve terminals which are distributed throughout the media as opposed to being localized around the adventitial medial border in arteries. Whether or not this is also true in cat is unknown; however, these anatomic findings may translate to physiologic responses such as venous constriction under sympathetic stress as likely found in our cats with acute left-sided congestive heart failure leading to absence of venous engorgement. In addition, owing to the aim of the study no attempt was made to further quantify the size the pulmonary vessels which may have led to underestimation of vessel size. Finally, as observed in dogs,18 many cats with congestive heart failure may have developed postcapillary or mixed pulmonary arterial hypertension increasing the size of the larger pulmonary branch arteries and affecting the ratio between artery and vein dimension as assessed subjectively in this study. Unfortunately, no attempts were made to noninvasively estimate pulmonary arterial pressure in our cats. Therefore, such underlying pathophysiology can only be speculated on.
A number of limitations of this study can be identified. Accuracy of thoracic radiography in the diagnosis of congestive heart failure may be limited due to subjectivity of interpretation, radiographic technique, type of underlying disease, observer variation, and other factors. Only cats with acute left-sided congestive heart failure were included whereas normal cats, cats with preclinical cardiac disease, and cats with primary respiratory disease were not. Therefore, information on the diagnostic accuracy of left atrial size estimation using thoracic radiography in a more diverse population of patients was not obtained. Left atrial size measurements using 2-D echocardiography do not consider the left auricle. However, this chamber may become very large occupying up to 50% of the left atrial volume as demonstrated in dogs23 and people.24 Therefore, left atrial size assessment using 2-D echocardiography may lead to clinically relevant underestimation of true left atrial size and volume. Only two observers evaluated the radiographic images, and observer variation of qualitative variables was not determined. Moreover, based on the inclusion criteria (cats with congestive heart failure only) observers were likely biased with regard to their qualitative assessment. However, observers were blinded to the quantitative echocardiographic measurements, in particular left atrial size variables, which may have off-set some bias. The size of the pulmonary arteries and veins were subjectively evaluated but not uniformly normalized to thoracic cavity or bony structures within the radiographic field of view25 which may have led to under or overestimation of vessel size. Pulmonary edema and pleural effusion may obscure the cardiac borders and pleural fluid may have falsely increased apparent cardiac size. The echocardiographic cutoff defining left atrial enlargement may have been too low overestimating the presence of left atrial enlargement in our study. However, there was excellent agreement between visual (subjective) and quantitative assessment using the decision threshold applied with a similar frequency of left atrial enlargement (93% vs. 96%) observed. A maximum left atrial dimension between 15.7 mm and 16.5 mm has been used in previous studies1, 10, 26 as indicators of increased left atrial size which is relatively similar to what was used in this study. Variables of left atrial size were not corrected for body weight or body surface area. However, although a dimensional variable of left atrial size, it has been shown to be relatively independent of body weight in cats.1 Finally, prior use of diuretic drugs such as furosemide will lead to a reduction of cardiac chamber and vessel size which may have affected the results of our study.
In conclusion, left atrial enlargement as assessed by thoracic radiography may be absent in a clinically relevant number of cats with acute left-sided congestive heart failure. Therefore, normal left atrial size on thoracic radiographs does not rule out presence of left-sided congestive heart failure in cats with clinical signs of respiratory distress.
ACKNOWLEDGEMENT
This study was supported by a Summer Research Student Grant from the College of Veterinary Medicine, The Ohio State University, Columbus, OH.