Infection with Devriesea agamarum and Chrysosporium guarroi in an inland bearded dragon (Pogona vitticeps)
Abstract
enObjective
Description of clinical, microbiological and histopathological findings in a case of deep dermatitis in an inland bearded dragon (Pogona vitticeps) caused by Devriesea agamarum and Chrysosporium guarroi.
Case report
A 4-year-old male inland bearded dragon, weighing 497 g, was presented at the clinic because the animal was suffering from dysecdysis and chronic skin lesions. Large numbers of bacilli, cocci and hyphal elements were diagnosed during the microscopic examination of the wound exudate. Microbiological analysis of a skin specimen revealed a moderate growth of Enterococcus sp. and D. agamarum. The condition of the bearded dragon improved with combined therapy consisting of ceftiofur hydrochloride, voriconazole and meloxicam. However, 3 months later recrudescence was observed. This time, Clostridium sp. and Chrysosporium sp. were isolated in large numbers. The bearded dragon was euthanized. Histopathology confirmed a severe granulomatous dermatitis with associated fungal hyphae and a severe granulomatous hepatitis with intralesional hyphae. Chrysosporium guarroi was identified by PCR and sequencing in two organs (skin and liver).
Conclusions and clinical importance
This is the first case of an infection with D. agamarum and C. guarroi in an inland bearded dragon (P. vitticeps). It emphasizes the importance of mycological cultures and specific treatment. Samples of suspected Chrysosporium sp. should be cultured at 30°C for 10–14 days. Early antifungal treatment is necessary to prevent systemic and potentially fatal infection with C. guarroi.
Résumé
frObjectifs
Décrire les données cliniques, microbiologiques et histopathologiques d'un cas de dermatite profonde d'un dragon barbu (Pogona vitticeps) liée à Devriesea agamarum et Chrysosporium guarroi.
Cas clinique
Un dragon barbu mâle de 4 ans, pesant 497 g, a été présenté en consultation pour des lésions cutanées chroniques et une dysecdysie. Un grand nombre de bacilles, cocci et hyphes ont été mis en évidence par examen microscopique de l'exsudat cutané. Les analyses microbiologiques de la peau ont permis une croissance modérée d' Enterococcus sp. et D. agamarum. L'état de l'animal s'est amélioré avec un traitement associant du ceftiofur hydrochloride, du voriconazole et du méloxicam. Cependant, 3 mois plus tard, une aggravation a été observée. Cette fois, Clostridium sp. et Chrysosporium sp. ont été isolés en grand nombre. L'animal a été euthanasié. L'histopathologie a confirmé une dermatite granulomateuse sévère associée à des hyphes fongiques et une sévère hépatite granulomateuse avec des hyphes intralésionnels. Chrysosporium guarroi a été identifié par PCR et séquençage dans deux organes (peau et foie).
Conclusions et importance clinique
Ceci est le premier cas d'infection à D. agamarum et C. guarroi chez un dragon barbu (P. vitticeps). Il met en avant l'importance des cultures fongiques et d'un traitement spécifique. Les échantillons suspectés d'etre Chrysosporium sp. doivent être mis en culture à 30°C pendant 10–14 jours. Un traitement antifongique précoce est nécessaire pour prévenir une infection systémique et potentiellement fatale avec C. guarroi.
Resumen
esIntroducción
Descripción de los hallazgos clínicos, microgiológicos e histopatológicos en un caso dermatitis profunda en un dragón barbudo (Pogona vitticeps) calzado por Devriesa agamarum y Chrysosporium guarroi.
Descripción del caso
Un macho de cuatro años de edad dragon barbudo que pesaba 497 g, se presentó en la clínica porque el animal estaba sufriendo disecdisis y lesiones crónicas de la piel. Un gran número de bacilos, cocos e hifas se diagnosticaron durante el examen microscópico del exudado de la herida. El análisis microbiológico de la muestra de piel reveló un crecimiento moderado de Enterococcus sp. y de D. agamarum. La condición del dragón barbudo mejoró con terapia combinada que consistía en este y hidrocloruro de ceftiofuro, voriconazol y meloxicam. Sin embargo a los tres meses se observó exacerbación de las lesiones. Esta vez se aislaron Clostridium sp. y Chrysosporium sp. en alto número. El dragón barbudo fue eutanasiado. La histopatología confirmó una dermatitis granulomatosa severa con presencia de hifas asociadas y una hepatitis severa granulomatosa con hifas intralesionales. Se identificó Chrysosporium guarroi mediante PCR y secuenciación en los dos órganos (piel e hígado).
Conclusiones e importancia clínica
Éste es el primer caso de una infección con D. agamarum y C. guarroi en un dragón barbudo (P. vitticeps). Este hallazgo ensalza la importancia de los cultivos micológicos y un tratamiento específico. Las muestras de casos sospechosos de Chrysosporium sp. deben ser cultivadas a 30°C durante 10 a 14 días. El tratamiento antifúngico temprano es necesario para prevenir la diseminación sistémica y la infección potencialmente fatal con C. guarroi.
Zusammenfassung
deZiel
Eine Beschreibung klinischer, mikrobiologischer und histopathologischer Befunde im Fall einer tiefen Dermatitis bei einer Bertagame (Pogona vitticeps), die verursacht war durch Devriesea agamarum und Chrysosporium guarroi.
Fallbericht
Eine 4 Jahre alte männliche inländische Bartagame mit 497 g Gewicht wurde der Klinik vorgestellt, weil das Tier an Dysecdysis und chronischen Hautveränderungen litt. Eine große Anzahl an Bazillen, Kokken und Hyphen wurde bei der mikroskopischen Untersuchung der Wundexsudate festgestellt. Die mikrobiologische Analyse der Hautproben zeigte ein moderates Wachstum von Enterococcus sp. und D. agamarum. Der Zustand der Bartagame verbesserte sich mit einer kombinierten Therapie bestehend aus Ceftiofur hydrochloride, Voriconazole and Meloxicam. Trotzdem wurde 3 Monate später ein Rezidiv beobachtet. Zu diesem Zeitpunkt wurde Clostridium sp. und Chrysosporium sp. in großer Anzahl isoliert. Die Bartagame wurde euthanasiert. Histopathologisch wurde eine schwere granulomatöse Dermatitis mit Pilzhyphen und eine schwere granulomatöse Hepatitis mit intraläsionalen Hyphen bestätigt. Chrysosporium guarroi wurde mittels PCR identifiziert und aus zwei Organen sequenziert (Haut und Leber).
Schlussfolgerungen und klinische Bedeutung
Es handelt sich hierbei um den ersten Fall einer Infektion mit D. agamarum and C. guarroi bei einer inländischen Bartagame (P. vitticeps). Das unterstreicht die Wichtigkeit einer Pilzkultur und einer speziellen Behandlung. Proben mit Verdacht auf Chrysosporium sp. sollten bei 30°C 10-14 Tage lang kultiviert werden. Eine frühzeitige Pilzbehandlung ist nötig, um eine systemische und möglicherweise fatale Infektion mit C. guarroi zu verhindern.
Abstract
chAbstract
jaIntroduction
Devriesea agamarum is part of the oral microbiota of clinically healthy bearded dragons and can also cause dermatitis.1 Chrysosporium guarroi has been isolated in cases of dermatomycosis in green iguanas and bearded dragons.2, 3 This case report describes clinical signs, diagnostic steps and treatment of a case of deep dermatitis associated with D. agamarum and C. guarroi.
Case report
A 4-year-old male inland bearded dragon (Pogona vitticeps), weighing 497 g, was presented with dysecdysis and chronic skin lesions. It had previously been treated orally (p.o.) with 10 mg/kg enrofloxacin (Baytril®; Bayer Austria GmbH, Vienna, Austria) given once a day for 6 days, then with miconazole nitrate, polymyxin B sulfate, prednisolone acetate (Surolan®; Janssen Pharmaceutica NV, Beerse, Belgium) and topical miconazole (Daktarin® 2% – Oral Gel; Janssen-Cilag Pharma, Vienna, Austria) for 10 days; however, the clinical signs deteriorated during this therapy. The dragon lived alone in a 190 cm × 70 cm × 90 cm enclosure (photoperiod 12.5 h, temperature 26–50°C, humidity 40–70%, cage substrate sand) and was fed a mixed diet of crickets and salad. Physical examination revealed weight loss (from a guide weight of 680 g compared with 497 g) and retained slough on the beard. Skin lesions were brown to black, erosive to ulcerative, 0.5–2 mm in diameter, in confluent areas up to 1 cm in diameter, and multifocally distributed all over the body (Figure 1). Differential diagnoses included bacterial, fungal or viral dermatitis.

Exudative material from a skin wound on the right mandible was examined microscopically using Ziehl Neelsen staining. No acid-fast organisms were observed; bacilli, cocci and hyphal elements were found during microscopic examination. A swab was taken from the skin lesions. Blood was collected from the tail vein for haematological and plasma chemical analysis (see Table S1 in Supporting information).
The dragon was hospitalized and treated with sodium chloride and glucose infusion (Fresenius Kabi, Graz, Austria), 20 mL/kg subcutaneously (s.c.), once a day for 20 days, and wound bathing with chamomile (Kamillosan®-Drops; Meda Pharma, Vienna, Austria) and povidone-iodine solution (Betaisodona® Standardized Solution; Mundipharma GmbH, Vienna, Austria) for 20 days. Ceftiofur hydrochloride (Eficur® 50 mg/mL; Laboratories Hipra SA, Amer, Spain) 5 mg/kg s.c. was given for 12 days, meloxicam (Metacam® 1.5 mg/mL; Boehringer Ingelheim Vetmedica, Ingelheim/Rhein, Germany) 0.1–0.5 mg/kg was given p.o. once a day for 5 days, and voriconazole (Vfend®; Pfizer Ltd, Vienna, Austria) 10 mg/kg was administered p.o. once a day for 14 days. The dragon was force fed with a herbal-based critical care diet for the first 3 days. The skin lesions were dry, clean and healing on re-evaluation on days 28, 42, 58 and 77.
On day 106, the owner represented the lizard with newly formed skin lesions. A swab for culture was taken from the new lesions. At the next visit (day 132), the lizard's condition had worsened. Therapy was based on s.c. fluid infusions, metronidazole (25 mg/mL suspension, magistral preparation) 25 mg/kg given p.o. once a day, voriconazole, topical iodine ointment (Betaisodona® Wound Gel; Mundipharma GmbH, Limburg/Lahn, Germany) and force feeding. On day 135, a blood sample was taken for haematological and plasma chemical analysis (see Table S1 in Supporting information). Despite treatment, the animal's physical condition deteriorated and it had to be euthanized.
Microbiology and histopathology
For bacteriological analysis, the skin sample was incubated on blood agar BD Columbia Agar with 5% sheep blood (BA; Becton Dickinson, Heidelberg, Germany) in aerobic/microaerophilic (5% CO2)/anaerobic conditions, and BD MacConkey II (Becton Dickinson) at 37°C for 24–48 h. After 24 h of incubation, the predominant colonies (bacterial isolate 2886/12) on BA were small, showing round, mucoid, semi-transparent colony morphology. After 48 h, colonies were surrounded by a narrow zone of haemolysis. Further characterization included Gram reaction, oxidase and catalase activity as described by Loncaric et al.4 For species characterization of the 2886/12 isolate, 16S rRNA gene sequence analysis was performed as described previously.5 The isolate was identified using the EzTaxon-e server (http://eztaxon-e.ezbiocloud.net/).6 The 16S rRNA gene sequence was submitted to Genbank (accession number KF647330) and was >99.9% similar to the type strain of D. agamarum IMP2T (EU009865). The high 16S rRNA gene sequence similarity between 2886/12 and the type strain of D. agamarum suggested species affiliation.
Apart from D. agamarum, a moderate amount of Enterococcus sp. was isolated; these organisms were Gram positive, catalase negative, had typical colonial appearance on BA and grew well on BD Enterococcosel Agar (Becton Dickinson). For the second bacterial examination (day 106), there were large numbers of Clostridium sp. (they were Gram positive; some cells appeared Gram variable, spore forming and grew in strictly anaerobic conditions, but without the double zone of haemolysis typical for Clostridium perfringens). For mycological analysis, samples were cultivated on BD Sabouraud Agar with gentamicin and chloramphenicol (Becton Dickinson Austria GmbH, Schwechat, Austria) at 30°C for 10 days. Fungal colony characteristics and microscopic features resembled Chrysosporium sp.
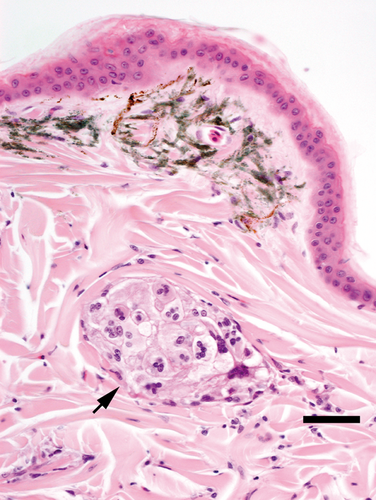
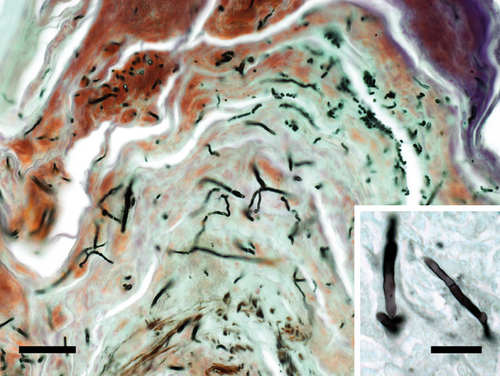
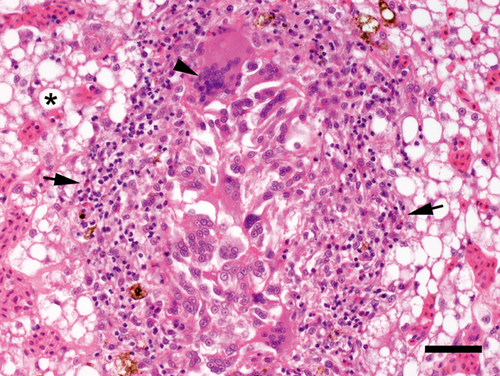
Postmortem histopathological findings in the region of the skin lesions confirmed a severe granulomatous dermatitis (Figure 2) with associated fungal hyphae (Figure 3). The liver showed a severe diffuse fatty degeneration and, in some areas, a severe granulomatous hepatitis (Figure 4) with intralesional hyphae (Figure 3, inset). In these skin and liver lesions, bacteria and acid-fast organisms were not found with special stains including haematoxylin and eosin, Ziehl Neelsen, Gram and Brown & Brenn. For identification of fungal species, DNA was extracted from pure cultures isolated from skin samples as well as from formalin-fixed, paraffin-embedded liver tissues using GenEluteTM Mammalian Genomic DNA Miniprep Kit (Sigma-Aldrich Handels GmbH, Vienna, Austria) or BiOstic FFPE Tissue DNA Isolation Kit (MO BIO Laboratories, Carlsbad, CA, USA) according to the manufacturer's instructions. PCR amplification of ITS1, the 5.8S rRNA gene, and ITS2 was performed as described previously and products were sequenced at LGC Genomics, Berlin.7 BLASTn with default settings (http://www.ncbi.nlm.nih.gov/BLAST) was used to compare both obtained sequences (culture from skin sample and the paraffin-embedded liver sample) with database sequences. The two sequences of ITS1-5.8S-ITS2 obtained (from skin and liver samples) were 527 bp and identical. A search on GenBank database using BLAST revealed that the sequences had 100% similarity to a C. guarroi CCFVB CH11 (EU018452.1) sequence. The sequence was submitted to Genbank (accession number KF647329). According to phylogenetic studies, C. guarroi has recently been placed in the genus Nannizziopsis.3
Biochemistry
Abnormal blood parameters, based on values for healthy bearded dragons,8, 9 included leukocytosis (days 1 and 135), heterophilia (days 1 and 135) and monocytosis (day 1); these could be associated with inflammation and infection. Lymphopenia (days 1 and 135) could be caused by malnutrition and stress.10 Hypercalcaemia (day 1) in a male inland bearded dragon8 could be the result of inadequate supplementation with calcium and vitamin D3; supplementation by the owner was not evaluated. Hypophosphataemia (day 135) could be associated with starvation.10
Discussion
Devriesea agamarum is a facultative pathogenic bacterium that is able to cause dermatitis and skin lesions;1 recommended treatments include ceftiofur hydrochloride at a dose of 5 mg/kg once daily.11 Large numbers of Clostridium sp. were isolated at the second bacterial examination (day 106) and were treated with metronidazole. The Enterococcus sp. isolate was considered to be nonpathogenic.
Fungal hyphae were observed during the microscopic examination of the wound exudate, leading to a tentative diagnosis of Aspergillus sp.; however, no fungi were isolated after culture of a swab sample. Later, Chrysosporium sp. was diagnosed in the same animal. It is possible that Chrysosporium sp. was microscopically misinterpreted as Aspergillus sp. and not found because the sample was only incubated routinely for 3 days. Colonies of C. guarroi are slow growing and reach 15–19 mm on Sabouraud dextrose agar after 14 days at 25°C.2 Clinical signs and histopathological findings in this case resembled those described for C. guarroi in green iguanas.12 Voriconazole, the recommended safe systemic therapy of Chrysosporium anamorph of Nannizziopsis vriesii (CANV) in bearded dragons,13 was chosen to treat suspected Aspergillus sp., and it appeared to be clinically effective. Treatment time would have been longer if C. guarroi had been identified at the first visit. After Chrysosporium sp. was isolated in the skin sample, voriconazole was started again. Unfortunately, the animal was already in a poor condition and suffering from a systemic fungal infection.
Samples of suspected Chrysosporium sp. should be cultured at 30°C for 10–14 days. Immediate antifungal treatment is necessary to avoid systemic and potentially fatal infection with C. guarroi. In a previous study, elimination of CANV by voriconazole was achieved on average after 47 days.13 Primary causes or predisposing factors of co-infection remain questionable. Husbandry seemed to be adequate, and other bearded dragons from the same owner, housed separately, were not affected.