Outcome of dogs treated with chemotherapy for mesothelioma: A retrospective clinical study on 40 cases and a literature review
Franck Floch currently works at AniCura TRIOVet, Rennes and Didier Lanore currently works at Hopia, Guyancourt, France.
Abstract
Mesothelioma is an uncommon cancer in dogs for which there is no established standard of care. Chemotherapy is often suggested despite no definitive proof of efficacy. The aim of this study was to evaluate the impact of chemotherapy on survival of dogs with mesothelioma. A retrospective multicentric study was carried out. To be included, dogs needed to present an evocative clinical evolution and a morphological diagnosis of mesothelioma. Exclusion of other cause of effusion and complete clinical follow-up were also required. Fourty dogs were included, 27 received chemotherapy (group 1) and 13 did not (group 2). Groups were heterogeneous regarding the proportion of animals undergoing surgery as part of their treatment (16 in group 1, 2 in group 2; p = .016) and homogeneous otherwise. Univariate analysis showed that dogs from group 1 survived significantly longer than dogs from group 2 (MST: 366 vs. 74 days; p < .001). Complete resolution of effusion after the first chemotherapy administration positively correlated with survival in group 1 (MST: 415 vs. 160 days; p < .01). All other variable tested had no significant impact on survival in univariate analysis, but dogs undergoing surgery and dogs having serous membranes' modification at medical imaging tended to survive longer. Multivariate analysis confirmed that chemotherapy was the sole variable independently associated with survival in our study (odds ratio 5.57–6.12; p < .01).
1 INTRODUCTION
Mesothelioma is a rare neoplasm in dogs originating from mesothelial cells. Its main clinical manifestation is effusions of the affected coelomic cavities. Its diagnosis is often challenging. Indeed, neoplastic and reactive hyperplastic mesothelial cells can appear very similar, and it is difficult to distinguish one from another at cytopathological examination in most cases.1, 2 Histopathological analysis can help in making the difference in some cases: invasion of the underlying tissues and presence of distant or lymph node metastasis are suggested criteria to differentiate mesothelioma from reactive mesothelium.3 However, presence of embolized mesothelial cells in lymph node has been reported in benign conditions and invasion into deeper structure cannot always be evaluated depending on the biopsy technique.4, 5 Furthermore, absence of tissue invasion does not preclude the diagnosis of mesothelioma.3, 6 Also, immunochemistry can help to comfort the mesothelial origin but it cannot demonstrate the neoplastic nature of the proliferation.6-8 Furthermore there is no validated marker or combination of markers that is very specific for mesothelioma.7-9 Consequently, morphological assessment alone, even with histopathology or immunochemistry, appears insufficient to diagnose mesothelioma; and, the final diagnosis is often the result of an integration of clinical, imaging and pathological data.
The absence of consensus on diagnostic procedures and the rarity of the disease may be partly responsible for the paucity of information regarding the therapeutic approach of canine mesothelioma. In people, mesothelioma is mainly pleural. It is also a rare and relatively poorly documented disease. Current therapeutic recommendations are based on surgical resection, when feasible, and platinum-based chemotherapy.10-12 In dogs, information on treatment is limited. Surgical procedures are often proposed in order to decrease the effusion's consequences, and sometimes in a cytoreductive intent. For instance, pericardiectomy is commonly performed for management of pericardial mesothelioma, and pleural port device are increasingly used for the management of pleural mesothelioma. Though, outcome associated with these surgical procedures is poorly documented.13-16 Regarding systemic treatments, for years the rationale for use of chemotherapy was based on a tendancy of better survival of treated dogs in very small cohorts of dogs or isolated reports compared to historical data.1, 17, 18 Recently, a larger cohort of 34 dogs, including a control group, was published by Moberg et al. and also reported a better outcome in dogs with mesothelioma treated with chemotherapy.16 In this study, most dogs had pleural mesothelioma and the most used chemotherapeutic agent was 5-fluorouracil, administered intracavitarily. No survival prognostic factors were identified.
The primary objective of this study was to evaluate the impact of chemotherapy on survival of dogs with mesothelioma. The secondary objective was to determine prognostic factors associated with survival among treated dogs.
2 METHODS
2.1 Cell line validation statement
No cell line was used.
2.2 Case selection
Dogs diagnosed with mesothelioma between January 2004 and April 2020 were included from six veterinary institutions. To be included in the study, dogs needed to fulfil four inclusion criteria. First, a morphological diagnosis of mesothelioma by a board-certified pathologist or clinical pathologist was necessary. However, this was not considered sufficient in the absence of consensus on morphological diagnosis of mesothelioma. Second criteria was a clinical course evocative of mesothelioma, with recurrent effusions of no other possible cause identified. Third, medical imaging of the cavity involved needed to be performed at diagnosis. Fourth, a complete medical record and follow-up needed to be available for review.
2.3 Data collection
For all animals, information collected regarding diagnostic procedures included review of cytopathological or histopathological report, neoplastic cavities' imaging reports, and staging procedures. Result of immunostaining were also collected when available. Double positivity for antibody-staining against cytokeratin AE1/AE3 and vimentin or smooth actin was considered suggestive of a mesothelial origin. Staging procedures included thoracic, cardiac and/or abdominal imaging associated with morphological analysis of any suspicious lesion identified. Imaging procedures included radiographs or CT scan for thorax, echocardiography for cardiac evaluation and, ultrasonography or CT scan for abdomen.
Regarding treatments, data collected included every therapeutic procedure performed or medication administered, including dose and frequency. Regarding chemotherapy, data collected included molecule, dose, frequency, route of administration (intravenous, intracavitary, or both), adverse events, response to treatment, and date of relapse when applicable. Adverse events were retrospectively classified according to VCOG-CTCAE.19 Response to treatment was evaluated based on persistence of effusion at sonography. When possible, evolution of measurable nodule or mass were evaluated according to the RECIST criteria.20, 21 Regarding therapeutic surgery, it included any decompressive or cytoreductive surgical procedures, such as pericardiectomy or pleural port placement. On the contrary, diagnostic surgical procedures (i.e., biopsy collection) were not considered a therapeutic procedure.
In addition, signalment (age, breed, gender and reproductive status), duration of clinical signs prior to diagnosis, number and location of neoplastic effusions at diagnosis, and survival time were also retrieved from medical files.
2.4 Statistical analysis
Dogs were divided into two groups depending on the treatment they received. Dogs receiving chemotherapy constituted group 1 and other dogs constituted group 2.
First, homogeneity between groups was verified. Categorical data tested were gender, reproductive status, number and location of effusions, initial clinical signs duration (categorized as more or less than 30 days), presence of abnormalities of serous membranes at medical imaging and performance of surgery. For those, Pearson's Chi-squared test was performed when there were more than five individuals in each set of data; if not, Fisher's exact test was performed. Continuous data included age and clinical signs duration. Shapiro–Wilk test was performed to assess their distribution type. Both were not normally distributed; therefore Mann–Whitney U test was used to assess the homogeneity between groups. Statistical significance threshold was set at p < .05 for all analyses.
The endpoint of the study was survival. It was defined as the duration from the first morphological diagnosis to death from progression of the disease or censor. Dogs were censored if they were still alive at time of data collection, lost to follow-up or if they died from another cause. For survival analyses, duration of clinical signs was split into two groups of <30 days or ≥30 days and considered as a categorical data. Categorical data evaluated for their impact on survival included those previously mentioned and group. Age was the only continuous data evaluated. Comparison of survivals was performed using Kaplan–Meier method followed by log-rank tests for categorical data, and Pearson's correlation product for continuous data. Significance was set at p < .05 for univariate analysis but all data with p < .20 were then included in a Cox proportional hazards model multivariate analysis.
Another analysis was performed among group 1 to detect any relevant prognostic factor. Tested parameters included response to treatment, route of chemotherapy administration and all categorical data previously mentioned. Response to treatment was retrospectively classified into complete and uncomplete, based on ultrasonography performed 3 weeks after the first chemotherapy session. Complete response (CR) was defined as disappearance of any neoplastic effusion previously diagnosed, absence of newly diagnosed effusion. Progression-free interval (PFI) was evaluated only for complete responders and was define as the duration between the first documented CR to effusion relapse.
3 RESULTS
3.1 Population and clinical presentation
Forty dogs met the inclusion criteria which are fully displayed Table S1. The median age was 10.2 years (range: 3–13 years). There were 23 males including 18 intact, 4 neutered, and 1 for whom the reproductive status was unknown. There were 17 females including 5 intact, and 12 spayed. Most dogs were purebred (36/40). Golden Retriever was the most represented breed (11/40). Other breeds represented by more than one dog included German Shepherd (4/40), Yorkshire Terrier (4/40), Bernese Mountain Dog (3/40) and American Staffordshire Terrier (2/40).
The median duration of clinical signs before the first morphological diagnosis was 14 days (range 1–395 days, n = 31). Mesothelioma was pleural in 15 dogs, pericardial in 12, peritoneal in 2, pericardial and pleural in 6, peritoneal and pleural in 2, peritoneal and pericardial in 1 and pericardial, pleural, and peritoneal in 2. At presentation, effusions concerned several body cavities in 26 dogs (65%). Among them, 10 presented confirmed multiple neoplastic effusions, 4 presented only one tumoral effusion, and 12 presented one confirmed neoplastic effusion and other effusions of unknown nature. Fourteen dogs presented a unique tumoral effusion at presentation; among them, 2 had a history of other effusions. For statistical analyses, effusions of unknown nature suspected of being mesothelioma-related were noted as suspectedly neoplastic.
3.2 Imaging procedures
Pleural cavity imaging was performed in 37 dogs (92.5%) with computed tomography (CT) scan (19), radiographs (27) or, ultrasonography (11). Pericardial cavity imaging was performed in 35 dogs (87.5%) with CT scan (19) or, echocardiography (30). Abdominal imaging was performed in 29 dogs (72.5%) with CT scan (19) or, ultrasonography (16) (Table 1).
| Thoracic | Abdominal | Pericardial | |
|---|---|---|---|
| CT scan | 8 | 13 | 5 |
| Radiographs | 9 | ||
| Ultrasonography | 1 | 10 | 16 |
| CT scan and ultrasonography | 1 | 6 | 14 |
| CT scan and radiographs | 9 | ||
| Radiographs and ultrasonography | 8 | ||
| CT scan, radiographs, and ultrasonography | 1 | ||
| Total | 37 | 29 | 35 |
Imaging reports were retrospectively reviewed in 38 dogs; serous membranes were within normal limits (21/38, 55.3%), thickened (11/38, 28.9%), presented nodules (4/38, 10.5%), presented a mass (2/38, 5.3%), or were focally enhanced without hypertrophy at CT scan (2/38, 5.3%). Two dogs had both nodules and thickening of serous membranes. Both dogs presenting a mass had a histopathological diagnosis confirming mesothelial proliferation; one mass was heart-based, multilobulated and heterogeneous and the other was located at the right atrium, irregularly shaped, heterogenous, and poorly defined. Four dogs presented very mild intracavitary lymphadenopathies and two dogs presented moderate sus-sternal lymphadenopathy, though the lesions could not be aspirated due to their small size. One dog presented a lung-lobe torsion along with pleural and pericardial effusion; mesothelioma was histologically diagnosed on the parietal aspect of the torn lobe after the dog underwent lobectomy and pericardiectomy.
3.3 Morphological assessment
All dogs had a cytopathological evaluation of their effusions and it was suggestive of mesothelioma in 36/40 (90%). Three cytopathological examinations were unconclusive due to poor cellularity. For those three cases, subsequent histopathological examination was suggestive of mesothelioma. In the remaining case, cytopathological examination revealed a proliferation of well-differentiated mesothelial cells without any criteria of malignancy; diagnosis of mesothelioma was supported by histopathology and immunohistochemistry.
Histopathology was performed in 19 dogs and was evocative of mesothelioma in 16/19 (84.2%). In two dogs, histopathology suggested a mesothelial hyperplasia of unknown origin and for one dog, biopsies were of poor quality. All three had pericardial effusion for which the cytopathological evaluation was consistent with mesothelioma. All underwent pericardiectomy and the diagnosis was supported after recollection of the effusion in the pleural space and confirmed by a second cytopathological examination. On the 16 specimens with a tumoral diagnosis at histopathology, six presented emboli (37.5%); they were lymphatic in four, lymphatic and vascular in one, and not otherwise specified in one.
Immunohistostaining was performed in 10 dogs with: AE1/AE3 and vimentin (6/10), AE1/AE3 and smooth actin (1/10), AE1/AE3 alone (2/10) and vimentin alone (1/10). One dog presented positivity for AE3 and smooth actin, and negativity for AE1; results were all positive for every other cases. Immunocytostaining was performed in 3 dogs with AE1/AE3 and vimentin, and all were double positive.
3.4 Treatment
Twenty seven dogs received chemotherapy (group 1) and 13 did not (group 2). Chemotherapy was administered intracavitary in 12 dogs (44.4%), intravenously in 2 (7.4%) and both intracavitary and intravenously in 13 (48.1%). Agents used for intracavitary chemotherapy included cisplatin (13/25, 52%) and carboplatin (12/25, 48%). Agents used for intravenous chemotherapy included carboplatin (5/15, 33.3%), doxorubicin (4/15, 26.7%), alternance of carboplatin and doxorubicin (4/15, 26.7%), alternance of carboplatine and mitoxantrone (1/15, 6.6%) and a combination of cisplatin, carboplatin, mitomycin C and mitoxantrone (1/15, 6.6%). Eleven dogs received several molecules as part of their initial chemotherapy protocol (41%). One dog received metronomic therapy with chlorambucil at the end of his protocol. Response to chemotherapy was reported in 26 dogs and was complete 3 weeks after the first administration in 13 (50%). Follow-up of nodules was available in 2 dogs; one was reassessed after 1 month and presented disappearance of all nodules and the other one was reassessed after 5 months and presented nodules size's reduction. Dogs with uncomplete response after 3 weeks of treatment did not experience CR afterwards. Number of administrations varied from 1 to 10 (median = 4; n = 23). Four adverse events were recorded: grade 3 and grade 4 neutropenia, grade 2 thrombocytopenia, and grade 2 vomiting. No renal toxicity was reported.
Ten complete responders experienced a relapse after a median PFI of 242.5 days. Among all dogs undergoing chemotherapy, nine dogs received a second protocol after relapse (4/27, 14.8%) or following absence of response to the first-line treatment (5/27, 18.5%). These included repeating previous chemotherapy protocol (2/27, 7.4%), initiation of another maximum tolerated dose protocol (5/27, 18.5%), administration of toceranib (2/27, 7.4%), and pleurodesis (2/27, 7.4%). Three out of 4 dogs who had a CR to their first protocol experienced a CR to the second protocol; one was treated with toceranib, and two received a repeatition of their first platinum-based intracavitary protocol. Dogs not achieving a CR with their first protocol did not achieve a better response after the rescue protocol.
Eighteen dogs (45%) underwent therapeutic surgical procedures consisting of pericardiectomy (13/18, 72.2%), lobectomy and pericardiectomy (1/18, 5.6%), pleural port placement (3/18, 16.7%), and pleural port placement and pericardiectomy (1/18, 5.6%). Among them, only two dogs were from group 2; both underwent pericardiectomy.
Other treatments administered included prednisolone (27/40, 67.5%), non-steroidal anti-inflammatory drugs (6/40, 15%), furosemide (8/40, 20%) and sotalol (1/40, 2.5%). Seven dogs did not receive complementary treatments—4 from group 1 and 3 from group 2.
3.5 Survival analysis and prognostic factors
Twenty-six dogs died of tumour-related cause and 14 dogs were censored. Six died of other causes (cardiac arrest during surgery after relapse, piroplasmosis, leishmaniasis, histiocytic sarcoma and hit by car) and one died in unknown circumstances while his mesothelioma was still in remission. Six dogs were lost to follow-up after a median follow-up time of 273 days (range 41–779 days), and one was still alive at the time of data collection (after 274 days of follow-up).
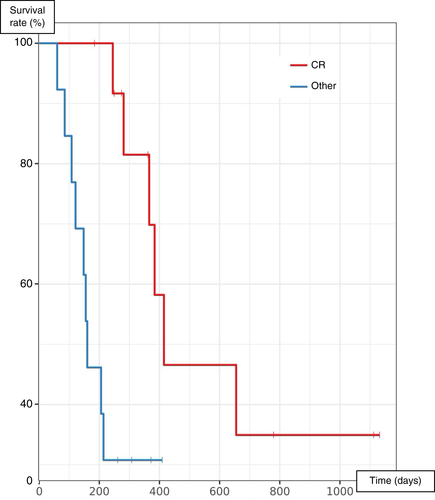
Group 1 and 2 were homogeneous except for performance of therapeutic-intent surgery: there was a significantly higher percentage of dogs undergoing surgery in group 1 than group 2 (p = .016). Among all factors tested for their impact on survival on univariate analysis, only chemotherapy was significantly associated with outcome, with a median survival time (MST) of 366 days for dogs from group 1 and 74 days for dogs from group 2 (p < .001) (Table 2, Figure 1). Dogs undergoing surgery as part of their treatment protocol tended to live longer than others, but this was not statistically significant (MST 366 vs. 151 days, p = .18). Dogs with serous membranes' abnormalities at imaging also tended to live longer (MST 288 vs. 155 days, p = .17). A multivariate analysis including all three parameters could not be conducted due to the low number of cases; therefore, two distinct multivariate analyses were conducted using chemotherapy performance as the first variable, and imaging results or surgery performance as the second. In both analyses, only chemotherapy remained significantly associated with survival (hazard ratio 5.37–6.12; p < .01, Table 3).
| Categorical data | Median (95% CI) | n | n events | p | |
|---|---|---|---|---|---|
| Gender | Male | 214 (151; 655) | 23 | 17 | .78 |
| Female | 245 (121; –) | 17 | 9 | – | |
| Reproductive status | Intact | 281 (160; –) | 23 | 16 | .5 |
| Neutered | 155 (60.0; –) | 16 | 9 | – | |
| Clinical signs' duration | < 30 days | 366 (147; –) | 19 | 12 | .49 |
| ≥ 30 days | 148 (121; –) | 12 | 9 | – | |
| Location of effusion | Pleural | 160 (141; –) | 15 | 10 | .73 |
| Pericardial | 306 (147; –) | 12 | 7 | – | |
| Peritoneal | 415 (415; –) | 2 | 1 | – | |
| Pericardial and pleural | 74 (60; –) | 6 | 5 | – | |
| Peritoneal and pleural | 273 (162; –) | 2 | 2 | – | |
| Peritoneal and peritoneal | – (–; –) | 1 | 0 | – | |
| Pericardial, pleural and peritoneal | 121 (121; −) | 2 | 1 | – | |
| Number of neoplastic effusions | One | 245 (155; –) | 29 | 18 | 0.28 |
| Multiple | 151 (74; –) | 11 | 8 | – | |
| Number of possibly neoplastic effusions | One | 214 (141; –) | 16 | 9 | 0.6 |
| Multiple | 206 (147; 655) | 24 | 17 | – | |
| Location | Pericardial | 306 (147; –) | 12 | 7 | 0.84 |
| Other | 162 (148; 655) | 28 | 19 | – | |
| Location | Pleural | 160 (141; –) | 15 | 10 | 0.98 |
| Other | 245 (147; –) | 25 | 16 | – | |
| Serous membranes' abnormalities at | No | 151 (74.0; –) | 19 | 14 | 0.17 |
| imaging | Yes | 384 (162; –) | 11 | 6 | – |
| Presence of nodules or mass | No | 214 (147; 655) | 32 | 21 | 0.62 |
| Yes | 384 (60; –) | 6 | 3 | – | |
| Presence of adenopathy | No | 206 (121; –) | 32 | 22 | 0.068 |
| Yes | – (415; –) | 6 | 2 | – | |
| Chemotherapy | Yes | 366 (214; –) | 27 | 16 | <0.001 |
| No | 74.0 (42.0; –) | 13 | 10 | – | |
| Surgery | Yes | 366 (206; –) | 18 | 10 | 0.18 |
| No | 151 (108; –) | 22 | 16 | – |
- Note: Significant p-values are in bold characters.

| Variable tested | Hazard ratio | p-value | |
|---|---|---|---|
| Group | Group 2 versus Group 1 | 5.57 [1.96; 15.8] | <.01 |
| Therapeutic-intent surgery | Performed vs not performed | 1.06 [0.416; 2.71] | .9 |
| Group | Group 2 versus Group 1 | 6.12 [2.31; 16.2] | <.001 |
| Serous membranes' abnormalities at imaging | Presence versus Absence | 0.585 [0.249; 1.37] | .22 |
- Note: Significant p-values are in bold characters.
Among group 1, response to treatment was the sole prognostic factor found in univariate analysis; complete responders after the first administration of chemotherapy had a MST of 415 days compared to 160 days for uncomplete responders (p < .01) (Table 4, Figure 2). Multivariate analysis could not be performed due to the limited number of cases.
| Categorical data | Median (95% CI) | n | n events | p | |
|---|---|---|---|---|---|
| Gender | Male | 366 (206; –) | 15 | 11 | .55 |
| Female | – (155; –) | 12 | 5 | – | |
| Reproductive status | Intact | 366 (206; –) | 18 | 12 | .77 |
| Neutered | – (155; –) | 9 | 4 | – | |
| Clinical signs' duration | <30 days | 384 (366; –) | 11 | 6 | .39 |
| ≥30 days | 248 (148; –) | 8 | 6 | – | |
| Location | Pleural | 214 (155; –) | 12 | 7 | .93 |
| Pericardial | 366 (245; –) | 8 | 4 | – | |
| Peritoneal | 415 (415; –) | 2 | 1 | – | |
| Pericardial and pleural | 358 60 (–; –) | 2 | 2 | – | |
| Peritoneal and pleural | 384 (–; –) | 1 | 1 | – | |
| Pericardial, pleural and peritoneal | 121 (121; –) | 2 | 1 | – | |
| Number of neoplastic effusions | One | 366 (214; –) | 22 | 12 | .46 |
| Multiple | 384 (121; –) | 5 | 4 | – | |
| Number of possibly neoplastic effusions | One | 245 (160; –) | 12 | 6 | .88 |
| Multiple | 366 (206; –) | 15 | 10 | – | |
| Location | Pericardial | 366 (245; –) | 8 | 4 | .98 |
| Other | 384 (160; –) | 19 | 12 | – | |
| Location | Pleural | 214 (155; –) | 12 | 7 | .92 |
| Other | 384 (245; –) | 15 | 9 | – | |
| Serous membranes' abnormalities at | No | 366 (214; –) | 11 | 7 | .84 |
| imaging | Yes | 384 (206; –) | 14 | 7 | – |
| Presence of nodules or mass | No | 366 (214; –) | 20 | 12 | .72 |
| Yes | 384 (384; –) | 5 | 2 | – | |
| Presence of adenopathy | No | 366 (206; –) | 21 | 13 | .083 |
| Yes | – (415; –) | 4 | 1 | – | |
| Intravenous chemotherapy | Yes | 384 (245; –) | 15 | 8 | .49 |
| No | 244 (155; –) | 12 | 8 | – | |
| Both intracavitary and intravenous | Yes | 384 (214; –) | 13 | 7 | .53 |
| chemotherapy | No | 263 (160; –) | 14 | 9 | – |
| Use of cisplatin | Yes | 384 (206; –) | 13 | 6 | .5 |
| No | 263 (155; –) | 14 | 10 | – | |
| Polychemotherapy | Yes | 384 (366; –) | 11 | 4 | .097 |
| No | 230 (155; –) | 16 | 12 | – | |
| Response to treatment | Complete | 415 (366; –) | 13 | 6 | <.01 |
| Other | 160 (121; –) | 13 | 9 | – | |
| Surgery | Yes | 366 (206; –) | 16 | 9 | .95 |
| No | 384 (160; –) | 11 | 7 | – |
- Note: Significant p-values are in bold characters.
3.6 Survival analysis among subpopulations
Considering only pleural mesothelioma, chemotherapy was the only treatment significantly associated with outcome (MST 214 vs. 40 days, p < .001). Surgery was not significantly associated with survival for pleural mesothelioma (MST 281 vs. 150 days, p = .38). Considering only pericardial mesothelioma, dogs treated with chemotherapy (MST 366 vs. 102 days, p = .086) and/or surgery (MST 366 vs. 147 days, p = .42) tended to live longer but this was not significant. Regarding dogs with multicavitary effusions, chemotherapy was positively associated with outcome (MST 366 vs. 74 days, p > .001) and surgery was not significantly associated with outcome (MST 366 vs. 147 days, p = .15). Multivariate studies could not be conducted due to the low number of cases. Full results are displayed Table S2.
Among dogs having a tumoral diagnosis at histopathology, all dogs presenting emboli (n = 6) were treated with chemotherapy and 5/6 had surgery. Among them, 3/6 had CR to chemotherapy. Dogs without emboli had a MST of 655 days compared to 310 for those who did, though this was not significant (p = .43) (Table S3).
4 DISCUSSION
Apart from a recently published retrospective study describing a relatively large series of mesothelioma,16 data on this tumour is rather scattered in the veterinary literature. To discuss our results, a systematic review was conducted. This review does not include the results of the study of Moberg et al. which are discussed separately. A total number of 122 cases of mesothelioma, fulfilling the four inclusion criteria set in our study, were found complicated in 47 isolated case reports and 10 case series.1, 6, 13, 17, 18, 22-73 Morphological evaluation was made by repeated cytopathological examinations in one case and histopathology in every other cases. Forty-four had immunohistochemistry performed. In the study of Moberg et al., 34 cases diagnosed with histopathology (32/34) or cell-block cytopathology (2/34) were described. Seventeen had immunohistochemistry performed.
In our population, pleural (62.5%) and pericardial (50%) cavities were the most commonly affected. Similarly, in Moberg's series, a majority of dogs had involvement of the pleural cavity (91.2%) and pericardial cavity was the second most commonly affected (47%).16 In our literature review, location was known in 120 dogs; it was pleural in 13 (10.8%), pericardial in 77 (64.2%), peritoneal in 15 (12.5%), pericardial and pleural in 6 (5%), pleural and peritoneal in 3 (2.5%), peritoneal and pericardial in 1 (0.8%%), tri-cavitary in 2 (1.7%) and concerned the tunica vaginalis in 3 (2.5%). Thus, pleural cavity was involved in 24% and pericardial cavity in 71.7% of cases. This difference could result from a selection bias; in fact, 61 pericardial mesotheliomas were included from case series on pericardial disease or pericardiectomy.1, 6, 38, 39, 45, 57 In contrast, no mesothelioma was included from cohorts of pleural or peritoneal diseases. Finally, as in humans, canine mesothelioma seems to mainly concern pleural cavity; though, pericardial cavity may be more frequently involved in dogs.11, 74
Medical imaging of the neoplastic cavity is required during the diagnosis of mesothelioma, especially to exclude other cause of effusion. Indeed, little is known about mesothelioma imaging; two studies on thoracic CT images of malignant and benign diseases showed parietal pleura thickening, nodular diaphragmatic thickening and thoracic wall invasion to be associated with thoracic malignancies.75, 76 Though, all intra-thoracic malignancies were treated at the same level and only a limited number of mesothelioma were included. In our cohort, medical imaging was unremarkable in 55.3% of cases; when abnormal, main finding was thickening of serous membrane (28.9%), and less frequently nodules or masses (15.8%). In Moberg's series, 27 description of thoracic and abdominal CT were available. No gross disease was identified in 33% of dogs; nodules were quite common (≥33%) as well as pleural (30%) and/or pericardial (11%) thickening. In previously published mesothelioma cases, imaging procedures' information were available for 56 dogs; thoracic/pericardial cavity was evaluated in 47 and abdominal cavity in 21. No abnormal lesion was found in 30 dogs (53.6%); common findings were serosal nodules/masses (17/56, 30.4%) and serosal thickening (9/56, 16.1%). Results should be compared with caution since they were obtained with several imaging techniques over a long period of time. However, results show that absence of imaging abnormalities is common. When present, serosal thickening, nodules and masses are the most common abnormalities.
In our series, chemotherapy was the only treatment significantly and independently associated with survival. MST was 366 days for dogs receiving chemotherapy compared to 74 days for those who did not. Moberg found similar results in a cohort of 34 dogs, with a MST from diagnosis to death of 234 days for 25 dogs treated with chemotherapy and 29 days for others.16 Twenty-four other cases of dogs receiving chemotherapy for the treatment of mesothelioma were identified in literature.1, 17, 18, 30, 32, 33, 36, 39-41, 46, 47, 49, 53, 56, 61, 69, 70, 73 It was administered intracavitary in 14 (58.3%), intravenously in 7 (29.1%) and both in 3 (12.5%). Intracavitary molecules administered were cisplatin (10), carboplatin (4), mitoxantrone and carboplatin (1), gemcitabine and carboplatin (1), and paclitaxel-loaded adipose tissue (1). Intravenous molecules were doxorubicin (5), mitoxantrone (2), cisplatin (1) and carboplatin (1). In published cases, dogs treated with chemotherapy also tented to survive longer (Table S4), even though there could be a selection bias. In the end, the three cohorts seem to indicate a benefit of chemotherapy.
In our study, response to chemotherapy was the only prognostic factor associated with survival among dogs treated with chemotherapy. After the first chemotherapy session, 50% were in CR. Moberg et al. reported 4% of complete responders and 37% of responders when assessing the response clinically and by quantification of residual effusion drainage, 3 weeks after the initiation of chemotherapy. Response to chemotherapy was assessed in 13 other published cases according to the criteria defined in our study; it was complete in 3/13 dogs. Differences in complete response rates must be interpreted cautiously considering possible evaluation bias and the rather small number of cases per group. Though, it could also be linked to the different protocols performed. For instance, cisplatin was used in 52% of dogs in our study, 46% in our literature review and no dog in Moberg's study. In humans, cisplatin is part of the first-line treatment of mesothelioma.10-12, 77 In dogs, it is not frequently used, mainly because of its associated nephrotoxicity; though, it seems well tolerated when administered intracavitary with adequate saline diuresis.17, 78 No case of nephrotoxicity was reported in our cohort. Moreover, several molecules were administered as the first-line chemotherapy in 41% of dogs in our cohort, 25% in our literature review and 17% in Moberg's cohort. In humans, response rates are higher with multi-agent protocols compared to single-agent protocols.79
In our study, dogs treated with surgery tended to live longer even though it was not significant. In Moberg's series, 20 dogs underwent perciardectomy and 22 dogs had a subcutaneous pleural and/or peritoneal port placed but outcome associated with those procedures was not displayed.16 In literature, surgery was performed in 71/105 (67.6%) dogs. It consisted of pericardiectomy in 61 (85.9%), debulking in 9 (12.6%), and both in 1 (1.4%). Dogs treated with surgery tended to survive longer; but, as in our cohort, most dogs received either surgery and chemotherapy or no treatment. In our cohort, only two dogs received surgery in the non-chemo group, which is not enough to assess effectiveness. When limiting our analysis to dogs receiving chemotherapy, no tendency could be found between surgery and outcome either in literature or in our cohort. Influence of surgery on outcome need to be further assessed; ideally, prospective studies on specific location with comparison of several type of surgical procedures would be necessary.
Main limitations of our study are due to its retrospective nature. Diagnostic, staging, and treatment protocols were not standardized. Multivariate analyses were necessary to conclude in most cases but could not always be performed due to the limited number of cases included. Even though complete staging was not performed in all dogs, imaging of the neoplastic cavity was always performed. Therefore, diagnosis based on cytopathological examinations were authorized, since cases of carcinomatous or sarcomatous effusions without any mass in the affected cavity appears unlikely.80 Furthermore, in human medicine, cytology can be an acceptable mean of diagnostic confirmation when clinical and imaging context are in favour of mesothelioma and biopsies cannot be collected.10, 81 Moreover, histopathological examinations are not always reliable and immunohistochemistry can only confirm the mesothelial origin and not the neoplastic nature of the proliferation.6 This is why morphological examination was always confronted to clinical and imaging results in our study, which decreases the risk of misdiagnosis.
5 CONCLUSION
Conclusively, chemotherapy was associated with an increased survival of dogs with mesothelioma in our cohort; complete response after the first administration was the only identified positive prognostic factor. Impact of surgery on survival remains unknown and might depend of neoplastic location.
ACKNOWLEDGEMENTS
Authors would like to deeply thank Dr Esther Piccirillo and Dr Laurie Boissy for their help in collecting a part of the files. Authors thank the veterinary hospital Advetia (Velizy-Villacoublay, France) and the veterinary school of Toulouse, from where some cases were included. Authors also thank Dr Isabelle Bublot (former practitioner in cardiology at VetAgro Sup) and the intensive care unit of VetAgro Sup for their help in the management of some of the cases and their help in the preliminary work in this study. Finally, authors thank all referring veterinarians, radiologists, cytopathologists and pathologists who have been involved in the diagnosis of the cases.
FUNDING INFORMATION
This work received no funding.
CONFLICT OF INTEREST
The author declares that there is no conflict of interest.
Open Research
DATA AVAILABILITY STATEMENT
The data that support the findings of this study are available from the corresponding author upon reasonable request.