Single-unit transfusions and hemoglobin trigger: relative impact on red cell utilization
Abstract
BACKGROUND
Patient blood management (PBM) programs can reduce unnecessary transfusions, but the optimal methods used to achieve this effect are unclear. We tested the hypothesis that encouraging single-unit red blood cell (RBC) transfusions in stable patients would have a greater impact on blood use than compliance with a specific hemoglobin (Hb) transfusion trigger alone.
STUDY DESIGN AND METHODS
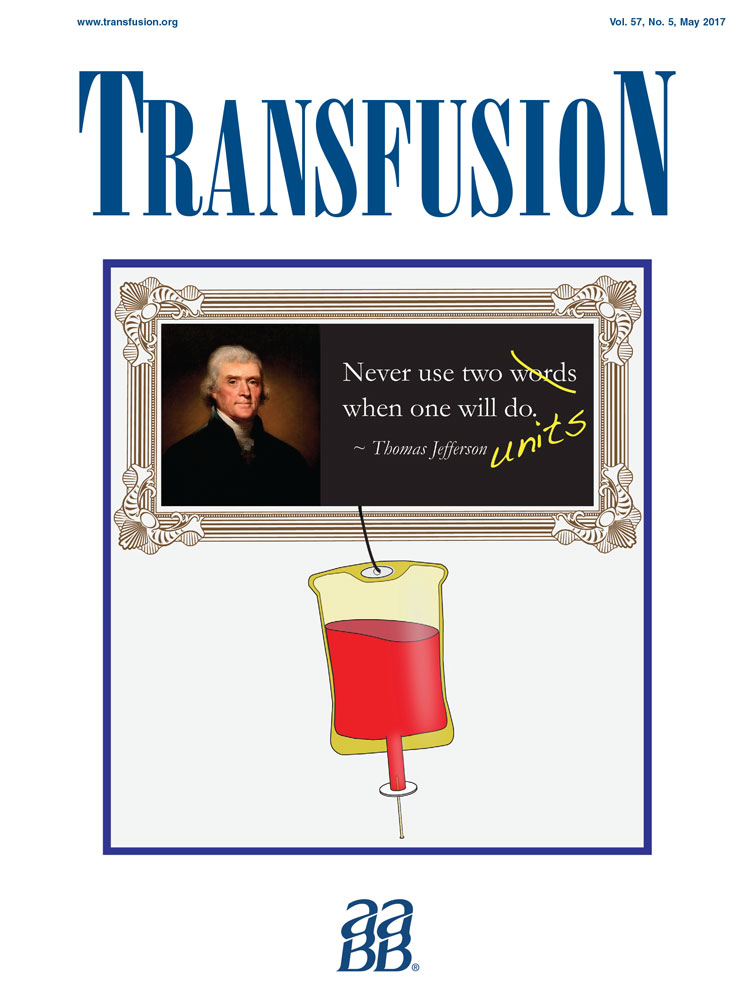
We analyzed blood utilization data at three community hospitals without previous PBM efforts before and after implementing a PBM program. Data were analyzed at monthly intervals to determine the relative impact of a “Why give 2 when 1 will do?” campaign promoting single-unit RBC transfusions and simultaneous efforts to promote evidence-based Hb triggers of 7 or 8 g/dL. Univariate and multivariate analyses were used to identify independent effects of these two interventions on overall RBC utilization.
RESULTS
Univariate analysis revealed that both the increase in single-unit transfusions (from 38.0% to 70.9%; p < 0.0001) and the decrease in RBC orders with an Hb trigger of at least 8 g/dL (from 45.7% to 25.0%; p < 0.0001) were associated with decreasing RBC utilization. Multivariate analysis showed that the increase in single-unit transfusions was an independent predictor of decreased RBC utilization, but the Hb triggers of both 7 and 8 g/dL were not. Overall, our PBM efforts decreased RBC utilization from 0.254 to 0.185 units/patient (27.2%) across all three hospitals (p = 0.0009).
CONCLUSIONS
A campaign promoting single-unit RBC transfusions had a greater impact on RBC utilization than did encouraging a restrictive transfusion trigger.