Recent advances in artificial intelligent strategies for tissue engineering and regenerative medicine
Abstract
Background
Tissue engineering and regenerative medicine (TERM) aim to repair or replace damaged or lost tissues or organs due to accidents, diseases, or aging, by applying different sciences. For this purpose, an essential part of TERM is the designing, manufacturing, and evaluating of scaffolds, cells, tissues, and organs. Artificial intelligence (AI) or the intelligence of machines or software can be effective in all areas where computers play a role.
Methods
The “artificial intelligence,” “machine learning,” “tissue engineering,” “clinical evaluation,” and “scaffold” keywords used for searching in various databases and articles published from 2000 to 2024 were evaluated.
Results
The combination of tissue engineering and AI has created a new generation of technological advancement in the biomedical industry. Experience in TERM has been refined using advanced design and manufacturing techniques. Advances in AI, particularly deep learning, offer an opportunity to improve scientific understanding and clinical outcomes in TERM.
Conclusion
The findings of this research show the high potential of AI, machine learning, and robots in the selection, design, and fabrication of scaffolds, cells, tissues, or organs, and their analysis, characterization, and evaluation after their implantation. AI can be a tool to accelerate the introduction of tissue engineering products to the bedside.
Highlights
- The capabilities of artificial intelligence (AI) can be used in different ways in all the different stages of TERM and not only solve the existing limitations, but also accelerate the processes, increase efficiency and precision, reduce costs, and complications after transplantation.
- ML predicts which technologies have the most efficient and easiest path to enter the market and clinic.
- The use of AI along with these imaging techniques can lead to the improvement of diagnostic information, the reduction of operator errors when reading images, and the improvement of image analysis (such as classification, localization, regression, and segmentation).
1 INTRODUCTION
The combination of tissue engineering and regenerative medicine (TERM) and artificial intelligence (AI) has created a new era of technological progress in the biomedical industry.1 Machine learning (ML) and deep learning (DL) allow us to optimize cell culture and facilitate organ and tissue engineering.2 By integrating AI into TE, we can also increase throughput, develop customized medical devices, and produce more functional tissues.3 TE also faces significant challenges, such as limited cell sources, vascular problems, immune system rejection, and poor integration with host tissues.4 Indeed, researchers are constantly exploring new techniques and tools to overcome these challenges and improve the clinical outcomes of TE that can be facilitated using AI.5
Designing and finding solutions for TE challenges due to the complexity of tissues and organs is not only difficult, but also time-consuming and resource-intensive. ML and TE use algorithms designed to learn about the environment, recognize patterns, and suggest solutions.6 Using these algorithms, it is possible to identify specific features in the data set that help to understand cellular or molecular processes.7 In addition, ML helps to train and identify patterns in complex biological structures and to solve 3D structures of protein complexes. DL in cell culture uses neural networks (NNs) to refine the design of scaffolds for desired tissues.8 This is also achieved by identifying patterns in large data sets, which can simplify feature detection and reduce the number of experiments needed to generate a structure. AI-based predictions in this field allow scientists to explore and analyze large data sets to identify molecules or biological structures that are difficult to identify using conventional methods.9
This combination makes it possible to find possible solutions to existing problems, speed up the TE process, and ultimately help create personalized medicine (PM) for patients,10 reducing costs, automating procedures and, most importantly, improving health outcomes. Some examples of important ways in which AI enables a specific combination with TERM are reviewed here.
2 AI APPLICATIONS IN TERM
The basis of TE is the selection of an optimal combination of biomaterials, cells, and signaling factors according to the specific conditions of the patient.3, 11-13 The TE structures development in the market is time-consuming, demanding, and expensive.11 More than half a trillion dollars are allocated annually in the United States to patients with disabilities.14 Currently, there is a large TE data collection that does not have a clear arrangement for quick reviewing and optimization of clinical solutions. The lack of guidelines for tissue designs and simple fabrication processes is one of the main limitations of TE.15, 16
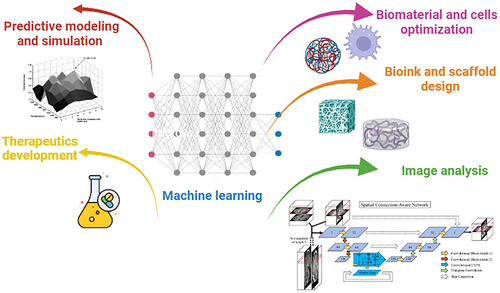
In recent years, several engineering principles have contributed to the faster development of TE.17 By combining computer science and mathematics, AI has been able to develop algorithms that can achieve human intelligence by machines.18 ML algorithms are a sub-branch of AI.19 They can help synchronize TE with other sciences, reduce costs, and accelerate bench-to-bedside translation by evaluating extensive TE data, relationships between them, and suitable strategies selection.15, 20 ML can help discover new drugs, materials, and enzymes, optimize manufacturing processes (such as electrospinning, freeze-drying, 3D printing, etc.) and new compounds, analyze images, and predict the success and performance of robotics in TE (Figure 1).21-24 AI leads to the entry of innovative and cost-effective TE products into the market in the shortest possible time and is known as the next step in the evolution of TE success.25
In addition, AI shortens the regulatory paths related to TE products. The entry of TE products into the market requires the approval of regulatory bodies such as the Food and Drug Administration (FDA) and European Medicines Agency (EMA), which takes a minimum of 3–6 months [510(k) pathway, for devices similar to existing devices] to 3–7 years (for new devices that require further investigation).11 In addition, the presence of cells, growth factors, and active agents in TE products has increased the cost of their development and evaluation in regulatory ways.26 ML helps facilitate this path. ML predicts which technologies have the most efficient and easiest path to enter the market and clinic. The FDA has also created new guidelines and pathways to expedite the evaluation of medical devices with AI.27 This section discusses the AI application in various aspects of TE.
2.1 Predictive modeling and simulation
In TE, predictive models are used to simulate scaffolds and biological processes,28, 29 predict the behavior of cells,30 and understand how tissues respond to various stimuli in a virtual and controlled environment.8 Predictive models with the help of ML algorithms and AI use the structure-property relationship of the existing data to predict the performance of the scaffolds.3 These models can predict how biomaterials interact with cells, tissues, and the surrounding environment to provide the mechanical and biochemical signals necessary for tissue regeneration. Furthermore, these models are used in the design of bioreactors similar to the body environment,31 simulating the growth of blood vessels,32 predicting the integration of scaffolds with body tissues and the reaction of the immune system to them,17 understanding complex biological processes,15 personalizing treatment approaches for the patient,33 and predicting the performance of new drugs and their effects on tissues.34 Xu et al.32 used different ANNs with more than 30 variables to achieve the best predictive model of vascular TE strategies and were able to accurately predict 94.24% (for a NN with two layers) and 91.45% (for a single-layer NN). Some of the models and algorithms used for this purpose are summarized in Table 1 and Figure 2.
| Model/Algorithm | Description |
|---|---|
| Finite Element Analysis (FEA) | A numerical technique for simulating the deformation and mechanical properties of scaffolds under load |
| Cellular Automata Models | A model for simulating the behavior and migration of cells and how tissue grows |
| Agent-Based Models | A model for predicting the behavior and interaction of different components within the tissue |
| Partial Differential Equations (PDEs) | a model for simulating the distribution and exchange of biochemical factors within the tissue (such as oxygen exchange) |
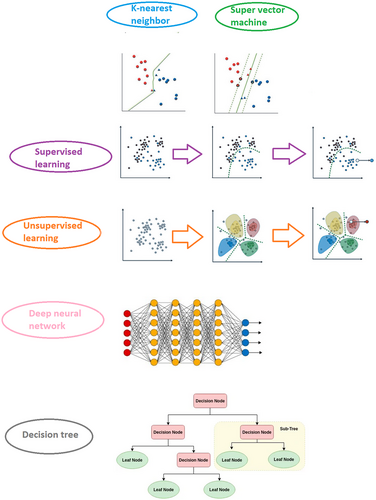
| Supervised Learning | These algorithms are used by receiving a combination of input data and corresponding output data and finding a pattern between them to predict the results of new input data. |
| Unsupervised Learning | These algorithms only include input to identify patterns between input values |
| Reinforcement Learning | This algorithm uses a reward-based system that evaluates the intelligent agent in each time interval and determines the agent's current state and reward from the set of available actions, and the agent is sent to the environment to move to a new state. |
| Deep learning | This algorithm is used for machine learning models with three or more layers, characterized by passing raw input information through each layer, summarizing parameters, extracting features, and complex relationships between data. |
| Regression | This algorithm is used when the outputs have continuous values. |
| Classification | This algorithm is used when the outputs have categories and labels. |
| Neural networks | Learning machines based on artificial neural networks are one of the most widely used fields in tissue engineering. These artificial neural networks encourage an algorithm simulated from the nerve cells of the human brain to simulate the way the brain processes problems. Machine learning consists of three or more-layered neural networks that are used in speech, image, and other fields. |
| Support Vector Machines (SVM) | A classification algorithm to find the best hyperplane of data of different categories |
| Decision Trees | Make decisions by dividing data into smaller parts |
| Random forests | uses a combination of different decision trees to improve accuracy |
| K-Nearest Neighbors (KNN) | Classification of data based on the most dominant class among KNN |
| Naive Bayes | probabilistic algorithm for classification |
The selection of each of these algorithms and models depends on the nature of the data and the desired result. Zhou et al.40 used the MeD-P ML model to predict the interaction between biomaterials and mesenchymal stem cells (MSCs, based on RNA sequence data) and optimize the performance of biomaterials on cell fate. Xu et al.41 developed a design engine using ANNs and decision trees to provide better TE designs in the treatment of laboratory animals.42
2.2 AI-driven optimization of biomaterial properties
Biomaterial design should be optimized according to the necessary physical and biological characteristics43 and includes the step-by-step selection of bioactive ligands based on biological studies and natural tissue structure, requires a lot of primary resources and time.44-46 AI networks (due to their ability to analyze a large set of data and provide predictive algorithms and models) can accelerate this and reduce costs.47, 48
Choosing the optimal algorithm (supervised and unsupervised learning) for biomaterials development is done according to the type and amount of available data.49 These algorithms predict the effect of motifs, functional groups, and their combination on the performance and properties of the resulting composite by evaluating molecular weight, rheological properties, chemical spectrum, synthesis methods, and characteristics of various polymers and biomaterials in databases such as Reaxys, PubChem, and Chem Spider, and lead to facilitating the discovery and design.50-52 There are various database libraries for various biomaterials, some of which are summarized in Table 2.
| Material | Database libraries | |||||
|---|---|---|---|---|---|---|
| Metal | Citrination | Materials Project | tmQM | MatWeb | Total Materia | NIST Inorganic Crystal Structure |
| Cceramic | MatWeb | Nist Ceramics WebBook (WebSCD) | Dielectric Database Online | |||
| Polymer | PoLyInfo | NanoMine | CROW | CAMPUS | Khazana | |
ML can help with the presentation of a set of optimal reproducible biomaterial designs, express the impact of their chemical composition on their biological activity and performance, and accelerate their entry into the market.53 To date, ML has been used in investigating the effect of biomaterials on peptide hydrogel formation,54 cell adhesion and protein absorption,55 and foreign body response.56 ML can be used to identify interactions between heterogeneous inputs such as chemical composition, processing conditions, concentration of additives, and others.57
To design biomaterials with the help of ML, a large library of experimental data must first be created. Li et al.54 created a library of 2000 self-assembled hydrogels based on Fmocamino acids, aldehydes, isocyanides, and amines. They were able to predict the relationship between the type and sequence of peptides and hydrogel properties by evaluating their molecular structure, rheological properties, cell adhesion, and morphology, with the help of regression models. This library played a significant role in determining the optimal sequence for various applications. Pugar et al.57 used the combination of inputs related to the composition and stoichiometry of polyurethane monomers with thermodynamic and physicochemical properties predictors to predict the mechanical properties and Young's modulus of different polyurethane formulations.
Barrett et al.58 evaluated the effect of amino acid motifs on the antifouling and antimicrobial properties of the resulting peptide using Bayesian networks. This model helps them to find that the effect of the background distribution of amino acids on the above properties is greater than that of sequence motifs. Kwaria et al.55 used a combination of SVM, Regression, and NN models and the chemical and structural information of the constituent molecules of 145 monolayers to predict the wettability and protein absorption of self-assembled monolayers. Their results showed the ability of the resulting models to predict the wettability and protein absorption of layers and the effect of each of the structural parameters on it, which helped to design optimal materials. Using an artificial NN, Echezarreta-López et al.59 examined the available data on bioactive glasses to determine the relationship between motif design, bioactive glass concentration, silver doping, and silicon doping on antimicrobial activity. Their results show the ability of NNs to predict interactions between parameters that traditional statistical analyses are unable to do.
2.3 AI-based design of scaffolds and bioinks for 3D printing
Scaffold fabrication methods are divided into two categories: conventional methods (including electrospinning, solvent casting, and phase separation) and modern 3D printing methods or additive manufacturing (AM, such as fused deposition modeling, extrusion, stereolithography, and VAT photopolymerization).60, 61 3D printing, as a revolutionary technology, has been widely used in the fabrication of drug release devices, scaffolds, artificial organs, and 3D drug screening models by eliminating the disadvantages of traditional methods.60 3D printing with layer-by-layer deposition of materials under computer control provides the possibility of reproducible construction of cost-effective, accurate, and patient-specific scaffolds with complex architecture, controllable pores, and high efficiency from a wide range of biomaterials.61 However, the fabrication of these scaffolds requires the optimization of fabrication parameters such as speed, temperature, nozzle diameter, and pressure.62, 63 In addition, the properties of the biomaterial used as bioink, such as printability, viscosity, and curing mechanism, are also effective in this optimization, which requires adjustment between a large number of different but highly correlated variables. bioink generally includes ceramics, polymers, cells, growth factors, etc., whose optimization requires exhausting, time-consuming, and expensive experimental tests that have delayed the introduction of this technology to the bedside.63, 64
Using AI to distinguish between low-quality and more promising print conditions is the first step to developing a suitable print condition detection system.23 AI can be helpful by using algorithms and ML networks to increase speed and dimensional accuracy, optimize bioink, and improve various stages of scaffold fabrication and 3D printing.23, 65 Algorithms predict the properties and printability of different bioink formulations and the correct ratio of various components in bioink based on input data (and not fixed program instructions).63 ML recognizes incompatible biomaterials in bioink preparation and provides an optimal protocol for different stages of printing (preprocessing, processing, and postprocessing).66 Menon et al.67 were able to predict the behavior of complex systems, increase the printing speed (2.5 times), and provide optimal formulations for silicone elastomer printing. ML can provide new proposals for scaffold design and upgrade existing designs based on customized recommendations and can be useful in maximizing repeatability, structural properties, printability, and print quality assessment (minimizing the use of materials and services) by predicting and optimizing printing parameters.68 For example, by providing the nozzle size, temperature, and pressure used for 3D printing and their corresponding outputs such as cell damage, time, mechanical properties, and cost, algorithms can be trained to predict the performance of new input data. Gu et al.69 used a combination of artificial NNs and various geometric data to predict the geometric configuration of different materials to print scaffolds with optimal mechanical properties (high toughness and strength). Conev et al.23 used regression and classification-based models (based on Random Forests) to predict the effect of poly(propylene fumarate) concentration and printing speed and pressure on the dimensional accuracy of materials. Their results indicated the ability of both models to correctly label most of the tested configurations.
Data sources used for AI-aided 3D printing are provided through clinical diagnostic, histological, and immunohistochemistry images. Layered images of scaffold printing steps are also involved in creating large-scale data libraries for ML analysis. With the help of these images, AI can be involved in the quality control of scaffolds and the detection of defects such as microstructure errors, wrongly positioned cells, and curved layers.70 By developing a DL method, Francis et al.71 predicted the amount of distortion of printed pieces with a laser-based method. Using sparse representation, naïve Bayes, decision tree, support vector machine, NN, and KNN ML algorithms, Tootooni et al.72 predicted the dimensional changes in the structure obtained from 3D printing and showed the best classification performance belongs to sparse representation.
Although there are few studies on the use of ML in 3D bioprinting processes, the combination of printing and ML can help evaluate drugs, reduce animal testing, reduce costs, predict the in vivo behavior of scaffolds, and accurately printing of damaged organs to help in replacement of damaged tissue and accelerates the progress of regenerative medicine.
2.4 ML for image analysis
Today, with the development of TE and the complexity of the resulting structures, various non-invasive medical imaging methods such as magnetic resonance imaging (MRI), computed tomography (CT), and optical coherence tomography (OCT) are needed for a more accurate evaluation of the tissue, each of which has various spatial resolution and use.73 The use of AI along with these imaging techniques can lead to the improvement of diagnostic information, the reduction of operator errors when reading images, and the improvement of image analysis (such as classification, localization, regression, and segmentation), which will be evaluated in detail in this section (Figure 3).
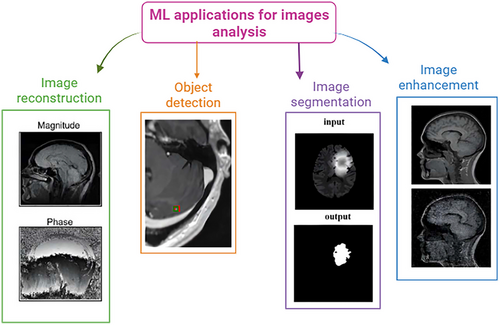
AI uses special algorithms for each step of image analysis. Classification algorithms lead to the classification of images (e.g., diseased and non-diseased images) into completely separate categories, regression algorithms lead to assigning a specific number to an image (for example, bone age estimation), and localization algorithms lead to determining specific tissue or part location in the image as the location of the center pixel, and the segmentation algorithms result in the segmentation of each pixel in the image as part of a specific object.77
MRI is one of the common soft tissue contrast imaging methods used to image implanted scaffolds and structures inside the body based on nuclear magnetic resonance.78 MRI has been used in various areas of TE, such as evaluation of the maturity of implanted cartilage scaffolds,79 continuous imaging of transplanted tissue,80 measuring the depth of skin tumors, the degree of involvement of underlying tissues, and the possibility of recurrence in grafts,81 prediction of abnormal brain structure in atopic dermatitis,82 and assessment of vascular growth within the scaffold.83 MRI image analysis is extensive and multifaceted. AI can help improve image reconstruction, noise removal and resolution improvement, object detection, image segmentation, and disease diagnosis and prediction based on MRI.39, 84 Wang et al.85 used functional MRI and AI software to compare brain responses to mechanical scratching stimuli (a nylon thread) in various types of skin [hairy (forearm) and glabrous (fingertip)]. Their results predicted and inferred that a scratch on the fingertip's skin turns into tactile information. On the skin of the forearm by stimulating the precuneus part of the brain, it turns into sensory information and itch, resulting in a stronger burning sensation. AI-assisted compressed sensing is an advanced DL NN that shortens the scanning time required for MRI, accelerates reconstruction and improves the quality of images.84 Hammernik et al.86 proposed a network of variables using ML, which accelerated the reconstruction of MRI images by examining free parameters, reducing the reconstruction time to 193 ms.
Image segmentation is done to accurately describe the contours of organs, tissue, and lesion structures, but generally, noise and artifacts of MRI images interfere with it.87 Various AI networks, such as U-Net, Mask RCNN, V-Net, and UNet++ have been designed to overcome this problem. Zhang et al.88 used Mask RCNN to segment breast tumor MRI images and achieved an accuracy of 0.75. Ronneberger et al.89 also used U-Net (with U encoder and decoder structure and a unique connection) to segment 2D medical images.
Object recognition is an important part of medical image processing, which uses a frame to mark the desired areas (such as lesions) and leads to improved segmentation accuracy. MRI slices include 2D and 3D sets. Despite the larger volume of information in 2D methods, the 3D ones provide background information and higher accuracy.90 Using convolutional NNs, Qi et al.91 were able to improve the diagnosis of cerebral microbleeds based on MRI images to an accuracy of more than 93.16%.
ML tools are also used to diagnose diseases based on MRI images. Various networks such as AlexNet and NNs have been used for more accurate classification and diagnosis of Parkinson's,92 Alzheimer's,93 survival of brain tumors,94 and schizophrenia95 based on MRI images.
CT is used as one of the typical diagnostic methods in clinics to image body tissues based on the attenuation of X-rays in different layers of the body and 3D reconstruction of the layers by computer.96 Various AI networks play a role in improving the above-mentioned aspects of CT image analysis. For example, the cone-beam back projection and the combination of filtered back projection algorithm with NN can be used to overcome limited-angle tomography and the inability of back projection to complete the end-to-end network in CT images.97 Solomon et al.98 used an AI reconstruction algorithm to reduce noise when reconstructing CT images. Generative adversarial networks (GAN) and sharpness loss, perceptual loss, and adversarial loss functions have been used to improve the quality of low-dose CT images and reduce their noise.99 In addition, ML models based on CT images were also used for the diagnosis of COVID-19100 and lung cancer.101
OCT, as a non-invasive, high-resolution optical imaging technique, can evaluate different degrees of absorption and scattering of light by different tissues to create images.102 Neural and GAN networks lead to noise removal from OCT images. Zhou et al.103 used the CycleGAN and conditional GAN networks to unify the style of OCT images and remove noise, respectively. In addition, AI helps to diagnose diseases related to retinopathy104 and glaucoma105 based on OCT images. OCT angiography can be used with the help of AL to segment and observe retinal blood vessels that cannot be seen with other methods. In general, ML networks help improve the analysis of medical images by improving the segmentation results or increasing the ability of a single network to extract data.
2.5 AI-enabled TE and therapeutics development
Considering the potential role of AI in various parts of TE, it is not far from expected that AI plays a role in the RM in clinical steps. When transplanting engineered tissue or constructs, AI can help choose an optimal immunosuppressive regimen and quickly assess the matching of the transplanted organs.106 In addition, by using AI in monitor systems, it is possible to observe the reaction in a real-time of the tissue repair process and help to maximize the repair efficiency with timely reactions.107 The use of AL-based approaches, especially cranioplasty, shows their increasing importance.108
On the other hand, the development of new drugs and therapies with conventional methods is a multi-step and expensive process (in three phases), and post-marketing monitoring, which costs more than 2 billion dollars.109-112 AI can speed up this processes and stimulate tissue repair by using databases and predicting effective therapeutic combinations.113, 114 Several ML algorithms have been used in each of these steps, such as SVM, convolutional NNs, DL, and deep NNs (for predicting drug-target interactions) and random forest, artificial NNs, and simple Bayesian (to evaluate the relationship between the physicochemical qualities of materials and their biological activity).109, 115
3 DESIGN AND IMPLEMENTATION OF TE EXPERIMENTS BASED ON AL
Some limitations in TE and RM such as loopholes in production, like trial-and-error inefficiency and lengthy processes and other shortcomings, may be managed by AI, automation, and robot's equipment. It is expected that AI automation through robotics revolutionizes traditional TERM and bring new hope to patients.116, 117
AI can determine the depth of laser-treated surfaces, and predict the topography of bone stem cells and their response, using artificial NNs and DL.118 Applications of DL in biology, medicine, and drug development have produced achievements that would have been virtually impossible without it,119, 120 for example, in clinical imaging, electronic health records, genomics, smart health monitoring, even the use of sensor-equipped smartphones.120-128
Recently, DL has been applied to microtopographies to indicate cell location in response to various (unseen) surface textures, yielding statistically significant predictions of adult skeletal stem cells from donors not used in the training dataset.121 Similar study was done on the response of human bone marrow stem cells (HBMSCs) to microenvironmental cues, and the morphology was analyzed using simpler ML models. in the case of microtopography studies, an accurate DL-based model of stem cell behavior can significantly reduce time and resources needed for long laboratory experiments. Importantly, these statistically significant predictions were made using a training set of about 200 images, far fewer than the thousands or tens of thousands that DL often requires.129, 130 The integration of AI by stem cell research is not limited to topographic response, but has also been used to understand differentiation potential,131, 132 determine response to microenvironmental signals,133 predict and detect pluripotent colony formation,122, 134 study immunosuppressive results,135 and provide general quality control automation.136, 137 In bioreactor-based experiments, machine learning models were able to predict whether the final level of human pluripotent stem cell-derived cardiomyocytes with therapeutic potential would be classified as “adequate” with an accuracy of 84% and would reach 90% after five days of feature analysis treatment after seven days.132
3.1 Robotic platforms and automated systems
TE plays an important role in prolonging life not only on Earth but also in space exploration; long space flights would benefit from TE/organ growth with robotic surgery to extend astronaut life.138
Robotics can improve TE steps performance.139-142 For example, recent soft robotics research has raised awareness of the importance of material properties,142, 143 shifting the focus from rigid elements to soft materials.143 Although recent advances have promised to close the performance gap with animals, current soft-robot actuators based on, for example, electroactive polymers, shape memory alloys or pressurized fluids are not yet mature enough to mimic the complex with high resolution.141, 142
3.2 Scaffolds as robots
-
Scaffold vibration (sequential compression and expansion at specific points/axes). This movement provides a quasi-static and dynamic stress/stimulus to the cells growing in the scaffold (see, e.g., the honeycomb structure of muscle tissue referred to earlier). The driving signal for these oscillations can be periodic, perhaps sinusoidal; Optimal configuration profiles should be determined through experimentation and are problem dependent.
-
Relative move between parts (at the larger scale): When two parts can move and rotate against each other, scaffolds that have this flexibility can help tissues grow better than ones that cannot move.
-
Isotropic size modifications (preserves shape, uniform in all directions), for example, increasing size to accommodate growth in life. This can be useful when the handle is implanted in, for example, a newborn and needs to adapt to an increase in body size. It also seems useful for building large scaffolds138: the literature points to the fact that traditional cell seeding techniques may not provide sufficient cell mass for larger structures.144 In this case, we recommend starting with a smaller seeded stand and gradually increasing its size.138
-
Embryotype developmental growth is supported by anisotropic size changes where some may grow earlier, some later, some may dissolve/disintegrate earlier and others later, ensuring the temporal growth of complex organ structures. Controlled biodegradation/absorption can also be the basis of the scaffold construction method (morphable, in vivo design).138
Other features will also be useful for future scaffolds and bring them closer to today's robots. In addition to movement/reconfiguration enabled by guided activity, other applications of scaffold robots can be used in detection, computation/control, and communication and sensing physical and chemical parameters, such as pH, temperature, and stress. Computing even simple algorithms for feature detection mapping is complex and could benefit from good models. It defines the controls for effective/optimal release and movement of drugs. It seems useful to equip the scaffold with a communication capability: as a receiver, for remote control (motion, drug release) or as a transmitter of information detected or determined by the scaffold, scaffold status, etc., interactions with other tissues/organs, interaction with extracorporeal instruments, and remote access, from outside the human body.138
3.3 Computational optimization
Traditionally, scaffolds were made based on trial-and-error method in a very time-consuming, expensive, and sometimes lacks precise control manner. The use of computational methods such as computer-aided design (CAD), finite element analysis (FEA), and computational fluid dynamics (CFD) can significantly reduce the number of test iterations to improve scaffold properties. With reasonable accuracy of simulation results, CAD has also become a tool to predict scaffold properties before production and testing.145-147 It is particularly useful to predict some properties and behaviors of the framework that are rarely experimentally investigated, such as the stress-strain distribution. All this means the advantages of using computational methods in the design of the scaffold. Overall, computational methods for scaffold design not only improve the traditional scaffold manufacturing process, but more importantly, open a new path in tissue engineering, providing researchers with a wide and flexible choice for scaffold design and optimization.145
It is important to note that the spread of computer-aided frame design cannot be separated from the development of 3D printing or AM. Production technology places strict limits on frame design. For example, pore size cannot be precisely controlled by traditional manufacturing methods such as gas foaming, solvent casting, and freeze drying.148 As a result, if computationally designed and optimized scaffolds cannot be easily and accurately produced, this may undermine the importance of designing such scaffolds. Fortunately, using 3D printing, scaffolds can be manufactured according to a CAD in less time, with greater flexibility and precision than traditional scaffolding techniques.148, 149 Compared to traditional scaffold fabrication techniques, 3D printing can produce scaffolds with highly complex microstructures with precise control and easy design modification.145, 150 Although current 3D printing techniques are not yet perfect for producing scaffolds of all desired shapes and sizes, their advantages over traditional production techniques and the great potential of scaffold fabrication still make it promising for the manufacture of computer-designed scaffolds.111
Different loads on transplanted scaffolds include compressive, tensile, shear, torsional, bending, and biomechanical/physiological loads.151-153 Compression is the most common in vivo loading.154 The loading sizes vary greatly between apps. For example, the forces experienced in a bone scaffold are hundreds or even a few thousand Newton.155 However, some polymer scaffolds can only withstand up to 100 Newton.154 Therefore, it is very important to consider the mechanical properties and behavior of scaffolds.
Topology optimization is a much more powerful tool in scaffold design than size and shape optimization.156, 157 The purpose of topology optimization is to determine the best distribution of a limited number of materials in a given area under certain loading conditions to achieve certain desired properties.158-161 Porosity, structural modulus, and compatibility are some of the important properties that are often studied in scaffold topology optimization. Many studies have introduced topology optimization to design unit cells and support structures with desired porosity and mechanical properties. Typically, the objective function is to maximize stiffness (equal to minimizing compliance or strain energy) with constraints such as minimum porosity (equal to maximum volume fraction). In some cases, stiffness is also limited to achieve maximum porosity/permeability. Based on previous work, Hollister and Lin,156 one of the earliest researchers to introduce topology optimization, optimized a maximum permeability unit cell with a limited tolerance between targeted and effective flexibility and minimum porosity. In other early works, the unit cell was optimized to meet the desired stiffness by limiting its porosity and/or pore size.157, 162 Recently, Kang et al.163 optimized unit cell with an objective function to minimize the error between the targeted and effective bulk moduli and diffusivities by limiting its porosity. Almeida and Bártolo159 proposed a topology optimization method to obtain an optimal unit cell topology with minimal compatibility under different porosity and loading conditions. They further investigate optimized structures based on material interconnectivity to determine valid designs.159 Dias et al.160 introduced topology optimization to explore the best possible unit cell structure with maximum permeability limiting the elastic strain energy and volume fraction; they prepared the optimized structures using SLS and compared the experimental and computational results. Youssef et al.164 combined topology optimization with CFD and optimized frame structure to achieve a uniform shear stress distribution.
4 INTEGRATION OF TISSUE-LEVEL DATA WITH CLINICAL METADATA
4.1 ML-based integration of tissue engineering data for clinical decision support
ML refers to computer systems that create learning patterns using existing data and patterns. These patterns assist in better analysis, problem-solving, and decision-making.165 This data can encompass various topics, including laboratory data, particularly data derived from experimental work in TE.166 Today, ML is being utilized in clinical decision support systems and assist physicians at different levels of clinical decision, such as prediction, interpretation, diagnosis, and management of diseases.167
This technology can combine information and experimental data from laboratory research with clinical data to create new learning patterns. AI and ML reasoning techniques can assist physicians in the diagnosis and treatment of diseases, prediction of probable responses, increasing speed and accuracy, reducing medical errors, and selecting the best therapeutic strategies from larger data sets, more precise decision-making, and the choice of more cost-effective approaches.168, 169 As data is collected and stored using different objectives and methods results in increases in the level of dispersion, they must be stored in a common format in information systems to be utilized in AI-based systems and clinics. For example, digital imaging standards and communications in medicine (DICOM), picture archiving, and communication systems (PACS) are employed in medical imaging management. Therefore, establishing a platform for storing laboratory data (such as TE), clinical data, and information related to patients' clinical history in a suitable format for AI systems, can be the facilitator.170 Furthermore, the novelties of the field of TE and the diversity and complexity of human cells, tissues, and organs have resulted in insufficient data and strategies for conducting new experiments. Therefore, conducting new experiments requires examining various scattered resources and employing trial-and-error strategies, which can also increase human error. Based on input data, AI and ML are capable of creating algorithms to predict experimental results and the body's response to the methods employed in the experiments.171
Several experiments have been conducted to investigate the mechanisms of stem cells and molecular genetics in different organism, resulting in diverse data in this field. In a study, AI was utilized to develop insights and patterns from diverse datasets regarding the mechanisms of regeneration in worms. The created model holds the potential to be a valuable asset in advancing the field of TE.172 Consequently, selecting the optimal combination based on tissue type and patient requirements presents a challenging task. The presence of an intelligent system to integrate experimental data and facilitate appropriate selection becomes imperative.173 In this regard, AI was employed in a study to predict the outcomes of using various strategies for vascular TE.32 In another study, AI based on ANNs and decision trees was utilized to integrate experimental data in the field of tendon TE and establish a decision support system for selecting safe and cost-effective approaches. The results of this research indicated that 28 out of 30 models with tendon defects were successfully treated using the proposed AI-driven therapeutic strategies based on established patterns173
AI can provide a scheme for categorizing experimental data that enables searching between different datasets. In this context, a group employed AI aggregated experimental data of cartilage TE in a centralized system. They successfully identified suitable treatment schemes for 18 animals of 20 examined animals.41 Dhondalay et al. constructed an AI system based on ANNs and gathered experimental data on the impact of various factors on the quality, efficiency, and surface markers of cells used in cell therapy. Their work demonstrated that ANNs can help in selecting influential factors in large-scale cell processing and production.174 Thus, it can be concluded that AI, through DL approaches, enables the establishment of connections between new and old data in TE and help to more accurate and faster clinical decisions.41
4.2 AI-assisted analysis of patient-specific data
ML and other subsets of AI not only can be beneficial in the analysis of medical and biomedical data and disease prediction, analysis, and enhancing the resolution of medical imaging and analyzing histopathological images, but also can help selecting appropriate therapeutic methods with lower error rates based on specific patient data. These systems help physicians with high accuracy and without fatigue, enabling the comparison of individual patient data with large volumes of laboratory and clinical data.175 In image classification, the objective is to classify or predict a specific class of object in an image, which can aid in disease prediction based on existing patterns. In object detection, it identifies and classifies specific regions within an image, enabling the search for specific objects, such as the detection of specific cell types.176 Histopathological images are utilized for diagnosing diseases, including cancers. Analyzing histopathological images and comparing them with existing data is time-consuming and subject to disagreement. AI and ML methods for analyzing images and diagnosing patient diseases assists in more accurate and faster decision-making.177
4.3 Personalized medicine
Precision medicine or PM provides a new approach to targeted treatment based on individual genetic, biochemical, and physiological characteristics, including genes and proteins.178, 179 For this purpose, the use of clinical data and omic data together can be a way forward, and the use of clinical trials alone is not effective enough due to the lack of attention to individual genetic differences. Omic data includes various information including genomics, transcriptomics, proteomics, epigenomics, metagenomics, metabolomics, and nutrigenomics.180 To investigate and development of new drugs in the treatment of diseases, various experiments and clinical trials in different phases of preclinical (laboratory) and clinical stages are required. Pre-clinical phases are conducted to determine the pharmacokinetic properties, optimal dosage, and the drug's effects based on the type of disease by using cell and animal studies or expanding methods based on TE such as organ-on-chip and microfluidics.
Clinical trials are divided into four phases. In Phase I, the drug's effects and the optimal effective dosage are examined in a small group. Then, in Phases II and III, the drug's effects are studied in a larger population of patients.111 In Phase II, clinical trials evaluate the drug's efficacy, while in Phase III compare the efficacy of the new drug with previous standard treatments. Finally, Phase IV involves the introduction of the drug to the market and use in the general population and monitoring of unforeseen side effects of the drug. The integration of AI with each of these phases can enhance the accuracy of assessing and evaluating the efficacy of drugs and interventions, based on individual characteristics and contribute to the advancement of PM. In Phase I clinical trials, the potential impact and possible side effects of the new drug based on genetic factors in the patient are investigated. For this purpose, N-of-1 trials can be used where studies are conducted on one person.181 Also, the use of organoids together with cells isolated from the patient for pathology and drug tests is increasing as an effective approach in helping PM. The use of AI in these researchers for analysis can be helpful.182 In Phase II of studies, drugs and effective interventions must be examined in larger populations. The use of AI in this phase can assist in selecting the most suitable intervention based on available information and patterns. For example, several different drugs may be under investigation for a particular disease, and AI can propose the best treatment based on the patient's genetic characteristics and the mechanism of action of the drugs. If the safety and efficacy of drugs are approved, they can be used in Phase III clinical trials after approval by the FDA. By utilizing AI and creating “learning systems” based on the information obtained from the drug's effects on consuming individuals in clinical trials of Phases I, II, and III, as well as clinical histories and pharmacogenetic characteristics of patients, we can take another step towards PM. Recording and monitoring the effects of drugs or therapeutic interventions, as well as registering feedback or potential side effects, enables the support of advancing or replacing new therapeutic methods in the designed learning system during the subsequent phase.181
5 CONCLUSION
AI has many capabilities in RM that can solve or improve many limitations in this field. ML and DL have been successfully applied in the selection of biomaterial and cell, scaffold manufacturing methods, improvement of characterization methods and imaging, image analysis, prediction of results and outcomes, data classification, translation to the clinic and implantation, and even PM.
ACKNOWLEDGMENTS
The research was supported by grant no. 3867 (Semnan University of Medical Sciences).
CONFLICT OF INTEREST STATEMENT
The authors declare that they have no conflict of interest.
ETHICS STATEMENT
This article was approved by the ethical committee of Semnan University of medical sciences (Ethical Code: IR.SEMUMS.REC.1402.239).
Open Research
DATA AVAILABILITY STATEMENT
The data that support the findings of this study are available from the corresponding author upon reasonable request.




