RETRACTED: Association of partial infections with the risk of psoriasis: A two-sample Mendelian randomization study
Minghui Lu and Changyong Gao contributed equally to this study.
Abstract
Background
As a common chronic recurrent inflammatory skin disease, psoriasis is characterized by erythema and scaly skin lesions, with infection as an integral part of the pathogenesis of many diseases. Many previous cases reported the impact of psoriasis on infection. However, the existing research fails to completely clarify the infection factors associated with the potential of these diseases and causality.
Materials and methods
Thirteen kinds of pathogens and their immune responses and psoriasis in the phenotype of 46 species of SNPs data were respectively obtained from the GWAS catalog database and the UK biobank database. With the help of R software, three methods of inverse variance weighted (IVW), weighted median (WME), and MR-Egger regression were used to analyze the causality of the dataset.
Results
According to the results of IVW analysis, there is a causal relationship between anti-Epstein Barr virus antibody and psoriasis (OR: 1.003, 95% CI: 1.001∼1.006, P = 0.046) with a positive correlation.
Conclusion
Based on the results of MR analysis, there is a causal relationship between psoriasis and EBV infection, which indicates that EBV infection can increase the risk or severity of psoriasis. Therefore, in clinical scenarios, patients afflicted with psoriasis should be prevented from contracting the infection and recurrence of EBV as well as symptoms of psoriasis. The underlying immunological mechanism also provides a new perspective for experimental research.
1 INTRODUCTION
As a common chronic recurrent inflammatory skin disease characterized by erythematous and scaly skin lesions, psoriasis is usually immune-mediated in genetics, infection factors, endocrine factors, mental factors, drug factors, etc.1 The prevalence of the disease in the global population is about 2%.2 In addition to skin lesions, psoriasis can often implicate multiple systems, putting patients at increased risk of other comorbidities such as metabolic syndrome and cardiovascular disease.3
There is a pathophysiological relationship between infection and many chronic non-infectious diseases,4 such as cancer, psoriasis, rheumatoid arthritis, etc., which is an integral part of the pathogenesis of many diseases. In the study of Marius Rademaker et al.,5 possible infection factors associated with the onset of psoriasis were summarized, including streptococcus, staphylococcus aureus, pseudomonas aeruginosa, candida, helicobacter pylori, HPV, HIV, HBV, etc. However, the existing research fails to completely clarify the potential associations and causal relationship between infection factors and these diseases.
Mendelian randomization (MR) is an approach that helps to clarify the above-mentioned association. Through the study of the body's immune response to infection and disease of genetic markers, the potential causal relationship between the two can be revealed. With genotype as the instrumental variable, MR can be used to analyze the causal relationship between exposure factors and outcomes. Given that this method requires instrumental variables to have a strong correlation with exposure factors but have no direct relationship with possible confounding factors or outcome variables, the causality obtained by MR can avoid the influence of confounding factors with higher credibility.6 In this study, MR will be used to explore the causal relationship between psoriasis and some infections.
2 MATERIALS AND METHODS
2.1 Collection of instrumental variables
“Antibody immune responses” and “psoriasis” were retrieved as keywords in the GWAS catalog database (https://www.ebi.ac.uk/gwas/) and the UK biobank database (http://www.nealelab.is/uk-biobank). The SNPs dataset of the antibody immune response to some infections was obtained from the study4 Butler-Laporte G et al. in the GWAS catalog database.4 The SNPs dataset of the psoriasis was obtained from the UK biobank database, including 462 933 samples, 5314 cases, and 457 619 control groups.7 All respondents in the samples were of European ancestry to avoid the bias caused by ethnic factors. Meanwhile, all data used have been published in the public domain, with informed consent obtained from the participants. The local ethics committee also approved the study protocol without additional ethical approval.
2.2 Screening of instrumental variables
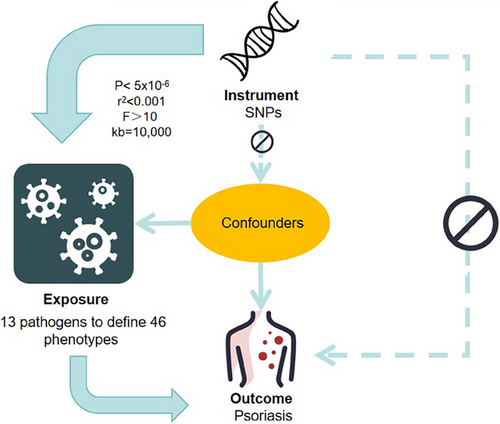
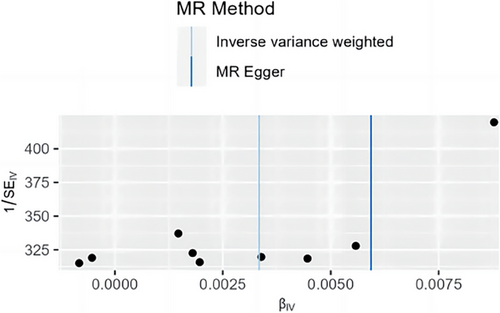
MR requires instrumental variables to satisfy three basic conditions as follows. (1) The strong correlation between instrumental variables and exposure factors. (2) The instrumental variables and confounding factors were independent of each other. (3) Instrumental variables only affect outcome variables through exposure factors. Therefore, P < 5×10−5, F > 10, and MAF > 0.01 were set to screen SNPs strongly correlated to exposure factors to avoid the influence of weak instrumental variables. Then, the r2 threshold was set to 0.001, with 10 000 KB as the regional scope of base pairs, to ensure that the results have no linkage disequilibrium (as seen in Figure 1). Finally, the PhenoScanner database was used to rule out confounding factors (Table S1).
2.3 Mendelian randomization analysis
The data of 46 phenotypes defined by 13 pathogens and SNPs of psoriasis were analyzed by three methods of MR analysis using the “TwoSampleMR” package in R software 4.2.1. The three methods mentioned above of MR analysis were Inverse-variance weighted (IVW), MR-Egger, and the weighted median (WME), respectively, usually with IVW analysis as the main reference basis. The results of MR-Egger regression and WME were used as the secondary reference. Then, IVW and MR-Egger combined with Cochran's Q test were used to test the heterogeneity of the data. If P < 0.05, there was heterogeneity of the data, leaving a certain influence on the analysis results. The intercept obtained by the MR-Egger was analyzed to test the data horizontal pleiotropy. P < 0.05 indicates that the data is pleiotropic, and the results do not meet the basic requirement of MR. Finally, the “leave-one-out” method was adopted to remove SNP individually and analyze the rest of the SNP, to determine whether there is a significant influence on the result of SNP.
3 RESULTS
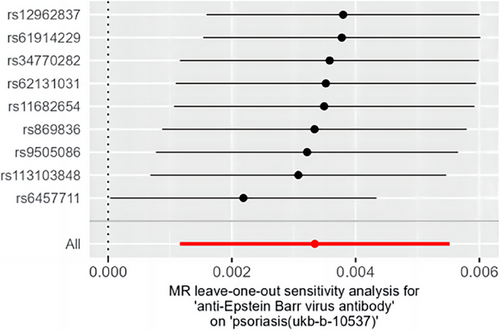
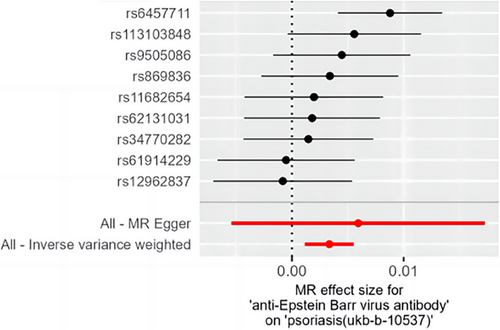
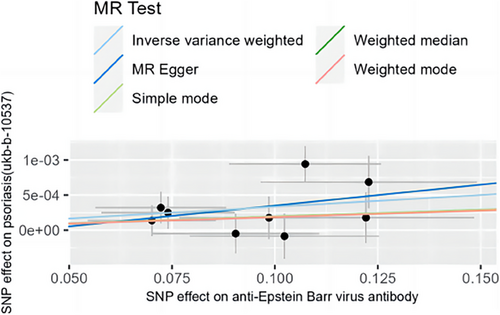
After IVW analysis, the results show that there is a positive causal relationship between anti-Epstein Barr virus antibody) and psoriasis (OR: 1.003, 95% CI: 1.001–1.006, P = 0.046), indicating that EB virus infection can increase the risk of psoriasis. In addition, P values obtained by the MR-Egger regression and WME analysis were greater than 0.05, so there is no statistical significance (Tables 1, S4, S5). According to Cochran’s Q test, P values obtained by IVW and MR-Egger were 0.268 and 0.208 respectively, greater than 0.05. Thus, the result has no heterogeneity (Table S3). Besides, the P value of the intercept obtained by MR-Egger was 0.662, which shows that the result has no horizontal pleiotropy (Table S2). After removing SNP by the “leave-one-out” method, the effect size of the remaining SNP was not much different from the total effect size. Thus, there was no SNP in the study that had a significant effect on the results as seen in Figure 2. The forest plot, funnel plot, and scatter plot obtained by MR analysis are shown in Figures 3, 4, and 5.
| Horizontal pleiotropy | Heterogeneity Cochran's | |||||||||||
|---|---|---|---|---|---|---|---|---|---|---|---|---|
| Exposure | Outcome | nSNP | Methods | β | SE | pval | OR (95%CI) | Egger intercept | SE | pval | Q | pval |
| anti-Epstein Barr virus antibody | Psoriasis | 9 | Inverse variance weighted | 0.003 | 0.001 | 0.046 | 1.003 (1.001–1.006) | 9.957 | 0.268 | |||
| MR Egger | 0.006 | 0.006 | 0.340 | 1.006 (0.995–1.017) | 0.0002 | 0.0005 | 0.662 | 9.669 | 0.208 | |||
| Weighted median | 0.002 | 0.001 | 0.185 | 1.002 (0.999–1.005) | ||||||||
- Abbreviations: CI, confidence interval; MR, Mendelian randomization; OR, odds ratio; SNPs, single nucleotide polymorphisms; WM, weighted median.;.
4 DISCUSSION
According to some case reports, the onset or exacerbation of psoriasis has been observed to be associated with infection.8-10 Loh E et al. found that the case of psoriasis occurred after EBV infection. Meanwhile, Jiyad Z et al. observed a type of pustular psoriasis patient afflicted with the EBV virus disease, and the correlation of available evidence was from observational studies. Due to deviation confusion and reverse causation, no reliable causal conclusions can be achieved. Therefore, the causal relationship between EBV infection and psoriasis is not clear-cut at present. However, this study investigated the possible causal relationship between some infection-mediated immune responses and psoriasis. The results suggest that EBV infection has a causal relationship with psoriasis, as EBV infection can lead to an increased risk of psoriasis.
Although there are few studies on this mechanism, some hypotheses could explain this causal relationship. According to previous studies, EBV DNA can regulate Th17 cells through Toll-like receptor 9 to induce IL-17 secretion.11, 12 Ohta et al. found that the peripheral blood of patients with chronic EBV infection has increased Th17 content and enhanced its ability to secrete IL-17,13 which is a key proinflammatory cytokine in the pathogenesis of psoriasis.14 Meanwhile, IL-17A can induce keratinocytes to produce TNF-α, vascular endothelial growth factor, IL-8, CXCL10, and other cytokines, which promotes the proliferation of keratinocytes, inhibits the differentiation of keratinocytes, attracts immune cells, and initiates and aggravates the skin inflammatory response.15 Additionally, this pathway is also an important link between psoriasis and many complications such as ulcerative colitis.16 Thus, it can be seen that the increased expression of Th17 in the dermis and the elevated levels of IL-17 may be one of the main potential mechanisms by which EBV infection triggers and exacerbates psoriasis.
As a new discovery in 2015 of cytokines, IL-39 (p19/ Epstein-Barr virus induced (EBI) 3) has shared p19 subunits with IL-23.17 IL-23 is also a key proinflammatory factor in psoriasis pathogenesis and rises in psoriatic lesions in the skin. Anti-IL23Ap19 antibody is known to be clinically effective in moderate to severe psoriasis,18 while anti-IL23AP19 antibody can bind to both IL-23 and IL-39, suggesting that both cytokines are involved in the pathogenesis of psoriasis. The results of immunohistochemical analysis confirmed that the expression of IL-23Ap19 and EBI3 was up-regulated in psoriatic lesions, and the expression of p19 and EBI3 was increased in keratinocytes, which also supported this view. Kota et al. found that the stimulation of TNF-α, IL-17A, and IFN-γ can raise EBI3 levels in psoriasis skin,19 while dexamethasone, vitamin D3, and vitamin A can inhibit such a process, which also has to do with the onset of psoriasis and treatment approaches. Therefore, EBI3 may be a potential therapeutic target for psoriasis in the future.
It is worth mentioning the possible role of the Notch signaling pathway, which is highly conserved and plays a role in regulating cell function, differentiation, and development. There are four major receptors, including Notch1, Notch2, Notch3, and Notch4. In the process of EBV infection, EBV can activate the Notch pathway through nuclear antigens, which further activate downstream signaling molecules.20 Some studies have observed that Notch1, Notch2, Notch3, and Notch4 receptors are expressed to a certain extent during the development of psoriasis. This pathway can mediate the proliferation and differentiation of epidermal keratinocytes, the generation of microvessels, and the proliferation, differentiation, and function regulation of T cells.21 Thus, the Notch signaling pathway may also be a vital way for EBV infection to affect the occurrence and development of psoriasis.
In addition, NF-κB signaling pathway may be a link between EBV infection and psoriasis. LMP1 is the major transforming antigen of EBV, which can mimic the CD40 receptor, recruit tumor necrosis factor receptor-associated factor (TRAF), activate NF-κB-inducing kinase, and then activate the NF-κB signaling pathway. Moreover, LMP1 can activate the PI3K-AKT-mTOR signaling pathway.22 NF-κB signaling pathway and PI3K-AKT-mTOR signaling pathway are crucial signaling pathways involved in the occurrence and development of psoriasis, which makes a difference in regulating the inflammatory process and keratinocyte proliferation.23
This study has several strengths. Firstly, this is the first study to use the two-sample MR method to explore the relationship between the immune responses to infectious diseases and psoriasis and to derive causal conclusions. Since the MR method is commonly used to investigate potential relationships between two factors that have been observed but not definitively proven to be associated, MR studies can help to more comprehensively understand the pathogenesis of diseases, thereby offering new clinical treatment perspectives. For example, an MR study by Wang Z. and colleagues analyzed the causal relationships between 975 blood metabolites and the risk of psoriasis, identifying the beneficial effects of unsaturated fatty acids on psoriasis and the negative effects of lipids, which may be mediated through pathways such as insulin resistance and inflammatory responses.24 This suggests that clinical treatment of psoriasis should consider the synergistic effects of a low-fat diet, as well as the potential of incorporating unsaturated fatty acids as an adjunctive treatment method. Similarly, MR studies like the one by Liu M et al. provide valuable evidence of a link between psoriasis and chronic obstructive pulmonary disease (COPD),25 which suggests that clinicians should be aware of the potential for some psoriasis patients to develop secondary COPD and provide timely and appropriate treatment. Our MR study clarifies the previously observed association between EBV infection and the onset of psoriasis, indicating that in clinical diagnostics and treatment, the possibility of EBV infection as a trigger should be considered and prompt administration of drugs like acyclovir that suppresses EBV, or the intake of substances like vitamin C and vitamin D that have inhibitory effects on EBV [26], should be considered. Therefore, this provides a novel reference for studying the relationship between EBV and the onset of psoriasis. Secondly, in the original literature, the UK Biobank cohort (UKB) was used to conduct up to 10 000 serological measurements on 20 infectious diseases,27 with 46 phenotypes defined using data from 13 pathogens. Compared with traditional studies, the data of this study were more reliable and comprehensive, which complemented the shortcomings of traditional observational studies. Thirdly, novel infectious diseases, such as polyomaviridae, Chlamydia trachomatis, and Toxoplasma gondii, were included in the MR analysis.
However, there are still some limitations to this study. First, the used dataset contained only populations from Europe. Although it was possible to minimize the effect of population stratification, this may have biased the results, preventing the analysis from being extended to all populations. Secondly, a few SNPs were below the common bioinformatics cutoff value of P < 5 × 10−8. Therefore, 5 × 10−5 was selected as the screening criterion for SNP based on previous studies.28, 29 Nevertheless, it may cause slight bias in instrumental variables and reduce the reliability of the results. Finally, many of the loci related to infectious diseases are also associated with other diseases, and the statistical effect size alone cannot clarify the underlying mechanism of causality. Therefore, stronger biological evidence is still needed to support a substantial causal relationship between EBV infection and psoriasis.
5 CONCLUSIONS
This study investigated the causal relationship between some infections and psoriasis using MR analysis, which is the first study to explore the causal relationship between EBV infection and an elevated risk of developing psoriasis using MR analysis. The results of this study further shed light on the pathogenesis of psoriasis factors and provide a new direction for experimental research to reveal the immunological mechanisms associated with EBV infection. At the same time, it can provide some reference for clinicians. When psoriasis patients are afflicted with EBV infection, intervention measures should be started as soon as possible to avoid the aggravation of the disease.
ACKNOWLEDGMENTS
This study did not receive any funding in any form.
CONFLICT OF INTEREST STATEMENT
The authors declare no conflicts of interest.
ETHICS STATEMENT
The data used in this study were retrieved from previous studies. Therefore, ethical approval was not required.
Open Research
DATA AVAILABILITY STATEMENT
Publicly available datasets were analyzed in this study. The summary level statistics of GWAS dataset for antibody immune responses and psoriasis can be accessed through the GWAS catalog database (https://www.ebi.ac.uk/gwas/) and the UK biobank database (http://www.nealelab.is/uk-biobank).