Unintended outcomes: Double halo nevus and vitiligo following laser therapy
Dear editor,
A 23-year-old female presented with a congenital dark-brown nevus on her upper left thigh, which has gradually enlarged over time and featured elongated hair at its center. Notably, a white halo appeared 3 years ago, which measured approximately 0.5 cm in width and was located about 1.0 cm away from the nevus (Figure 1A). Laser therapy was performed to the central nevus at a local hospital. One year later, a dark-red scar developed at the site of the laser treatment. The skin around the scar gradually became depigmented and presented with a halo, resulting in the distinctive appearance of a “double halo nevus”. Simultaneously, scattered depigmented patches were observed in other body regions, prompting the patient to present to our clinic. The patient denied any other significant medical history and family history.
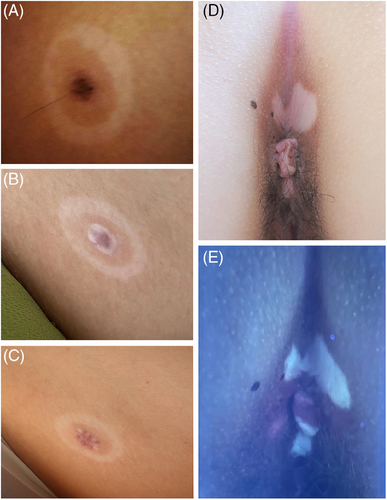
Physical examination revealed a four-ring elliptical skin lesion on the upper left thigh near the groin area, measuring approximately 3.0 cm × 2.0 cm (Figure 1B). This lesion exhibited a unique appearance, characterized by a central dark-red scar surrounded by inner and outer depigmented halos, with normal color skin between them. Interestingly, the three layers appeared to be roughly parallel in arrangement. Furthermore, we observed two irregularly shaped white patches around the anal mucosa. These two patches displayed a distinctive porcelain-white fluorescence under a Wood's lamp (Figure 1D,E). Similar vitiligo lesions were noted on her back.
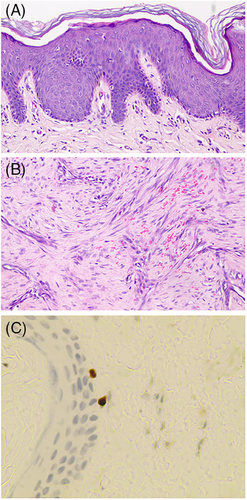
The central scar was excised and subjected to a biopsy. Histopathological analysis revealed a subtle increase in epidermal thickness, a reduction in melanocytes within the basal layer, increased fibroblast proliferation in the mid dermis, and localized collagen sclerosis (Figure 2A,B). These findings were in accordance with the characteristics of scar tissue. SOX-10 immunostaining revealed scattered melanocytes, albeit in lower numbers (Figure 2C). A diagnosis of vitiligo associated with nontypical halo nevus had been made based on all the examinations.
Halo nevus (HN) features a centrally pigmented melanocytic nevus encircled by a depigmented zone resembling halo. It is often associated with vitiligo. A recent study proposed a similar pathogenic mechanism for both conditions, marked by a dense infiltration of CD8+ T cells in the skin lesions.1 Workman et al. reported a case of a girl with congenital melanocytic nevus surrounded by a halo, along with vitiligo near the eyes and armpits.2 They suggested that if an autoimmune mechanism underlying both vitiligo and halo formation was assumed, removing the nevus, which acted as a potent antigen, led to a decrease in melanocytic antibodies. The residual melanocytes might have continued to trigger autoimmune responses. Some believe that individuals with HN may be more prone to developing vitiligo. As the age of HN patients decreases, the risk of developing vitiligo increases.3 Zemtsov et al. reported a case of systemic reaction occurring following CO2 laser tattoo removal, suggesting a potential inducement of generalized immune system activation by laser treatment.4 Furthermore, a recent study demonstrated that the development of vitiligo could be associated with immune-mediated melanocyte pyroptosis.5 This complex interplay of immune mechanisms may contribute to the development of vitiligo.
After the removal of central melanocytic nevus, our patient's depigmented area did not improve. Instead, a second depigmented ring and vitiligo appeared. Pathological examination found melanocytic cells, though significantly reduced. We hypothesized that laser therapy may not have eliminated all melanocytes, and the presence of residual melanocytic cells could explain the second HN. Interestingly, our patient displayed a distinctive first HN presentation with a ring of unaffected normal-colored skin encircling the nevus. We suspected that the depigmented area initially developed around the nevus as the secondary ring and then expanded outward centrifugally, leading to the formation of a ring-like lesion with atypical characteristics for HN. Caution is essential when contemplating the removal of melanocytic nevi, as procedures like laser therapy that result in nevus destruction may lead to the expansion of depigmented areas or even trigger the development of vitiligo.
ACKNOWLEDGMENTS
This research received no funding.
CONFLICT OF INTEREST STATEMENT
There is no conflict of interest.
INFORMED CONSENT STATEMENT
Signed consent was obtained from the patient for the publication of the case details included publication of the images.
Open Research
DATA AVAILABILITY STATEMENT
The data that support the findings of this study are available from the corresponding author upon reasonable request.




