Detection of superficial lymphatic malformation with dermoscopy and reflectance confocal microscopy
Er-Yi Lin and Lang Rao contributed equally to this work.
Abstract
Background
Superficial lymphatic malformation (SLM) is a congenital disorder of the lymphatic channels. It usually appears as clusters of vesicles filled with lymphatic fluid and blood on the skin that resemble frogspawn, making it difficult to distinguish from haemangiomas, angiokeratomas, and pyogenic granulomas. Although pathological results have diagnostic values, the significance of noninvasive examination in the diagnosis and differential diagnosis is also worth exploring.
Materials and Methods
A 24-year-old female presented with a history of multiple asymptomatic, pink lesions located on the chest since age 10. Histopathological examination was performed, and results informed the diagnosis of SLM. Lesions were detected by dermoscopy and reflectance confocal microscopy (RCM).
Results
Dermoscopy (polarized, 30×) revealed multiple yellowish-red lacunae in a light red background that were separated by pale septa and “hypopyon sign” was observed. RCM displayed a honeycomb pattern and multiple dark cavities in the upper dermal layers separated by thin septa with a few hypo-refractile cells at the periphery that demonstrated slow fluid flow via dynamic scanning.
Conclusion
We described a case of SLM detected by dermoscopy and RCM. Dermoscopic and RCM features may provide a potentially powerful, noninvasive instrument for the recognition and differentiation of SLM.
A 24-year-old female presented with a history of multiple asymptomatic, pink lesions located on the chest since age 10. The lesions gradually increased in size and blister-like structures appeared on the surface over a period of 4–5 years. The patient was otherwise healthy and had no significant family history. Physical examination revealed clusters of yellowish to pink blisters with a smooth surface and mulberry-like structure (Figure 1A). Dermoscopy (polarized, 30×) revealed multiple yellowish-red lacunae in a light red background that were separated by pale septa. A portion of the lesions contained blood that had accumulated in the lowest part of the lacunae (Figure 1C,D). Reflectance confocal microscopy (RCM, Vivascope 1500 Multilaser; CALIBER ID, Rochester, NY, USA) displayed a honeycomb pattern and thinning of the epidermis. Within the upper dermal layers, there were multiple dark lacunae (cavities) separated by thin septa with a few hypo-refractile cells at the periphery that demonstrated slow fluid flow via dynamic scanning (Figure 2A,B). Histopathological examination was performed, and results informed the diagnosis of superficial lymphatic malformation (Figure 1B).
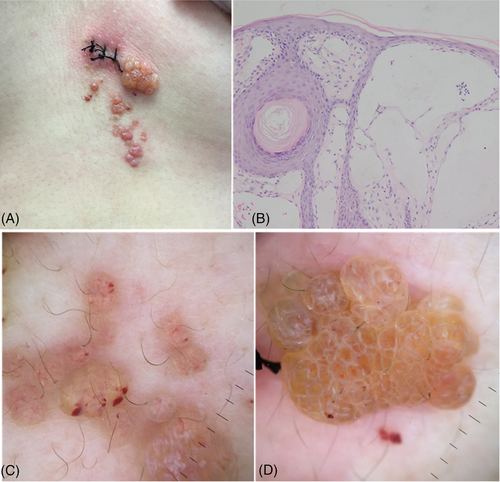
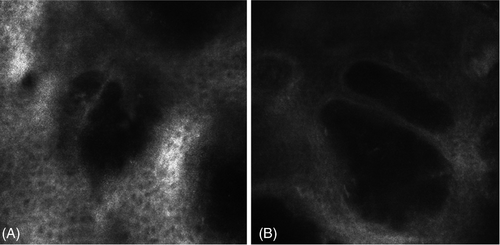
Superficial lymphatic malformation (SLM), also called lymphangioma circumscriptum, is a congenital disorder of the lymphatic channels that usually arise at childhood but can occur at any age. It is clinically characterized by clusters of vesicles filled with lymphatic fluid and blood on the skin that resemble frogspawn or mulberry.1 These vesicles correspond to dilated cavities in the RCM and dermoscopically present as yellowish and/or red lacunae with pale septa that correlate with the medium-refractile thin septa around the dark cavities in RCM. This observation is consistent with a histopathological finding that shows a lesion composed of multiple separated lymphatic vessels expanding into the upper dermis. In this case, lesions with two-toned lacunae, caused by lymphatic fluid in the upper part and accumulated blood at the bottom, were observed. In the literature, this SLM phenomenon is known as the “hypopyon sign” and is a hallmark dermoscopic feature that aids in the differentiation from haemangiomas, angiokeratomas, and pyogenic granulomas.2 Dark lacunae structures are most clearly observed in SLM by RCM; however other diseases also present with this feature, including haemangioma, angiokeratoma, and herpes simplex or herpes zoster. In RCM, hemangioma discloses many hypo-refractile cells, consistent with erythrocytes, moving rapidly within the central portion of the vessel lumen.3 Conversely, SLM is characterized by a small number of cells with different refraction rates–consistent with leukomonocyte, histocyte or erythrocytes–moving slowly at the periphery of the lacunae. Angiokeratoma typically presents via RCM as ectatic vascular lacunae with highly reflective scales, consistent with hyperkeratosis, on the surface and bright particles indicating blood cells within the lacunae. Further differentiation of angiokeratoma and SLM requires the combination of dermoscopy and pathological examination.4 Additionally, the dark spaces present in herpes simplex or herpes zoster appear as intraepidermal cavities with giant, ballooning cells that are easily identified by RCM.5 Isil Karaarslan and colleagues had reported a case of SLM with numerous hyper-refractile globular structures corresponding to lymphoid cells within the dark cavities revealed by RCM.6 However, this differs from our case, as here only dark lacunae and a small number of hypo-refractile cells were observed. Our histopathological findings may be due to the dilated lymphatic channels were predominantly filled with lymphatic fluid and few lymphoid cells was detected.
In summary, we described a case of SLM detected by dermoscopy and RCM. To our knowledge, the RCM characteristics of SLM are rarely reported. Dermoscopic and RCM features may provide a potentially powerful, noninvasive instrument for the recognition and differentiation of SLM.
ACKNOWLEDGMENTS
We gratefully acknowledge Professor Wang (Professor of Dermatology Hospital, Southern Medical University) for her guidance in writing.
CONFLICT OF INTEREST
The authors declare that there is no conflict of interest that could be perceived as prejudicing the impartiality of the research reported.
Open Research
DATA AVAILABILITY STATEMENT
The data that support the findings of this study are openly available in none at none.




