An Assessment of Third-Party Reporting of Close Ties to Measure Sensitive Behaviors: The Confidante Method to Measure Abortion Incidence in Ethiopia and Uganda
Abstract
Indirect estimation techniques are important tools for measuring sensitive and stigmatized behaviors. This includes third-party reporting methods, which have become increasingly common in the field of abortion measurement, where direct survey approaches notoriously lead to underreporting. This paper provides the first in-depth assessment of one of the most widely used of these techniques in the field of abortion measurement: the confidante method. We outline six key assumptions behind the confidante method and describe how violations of these assumptions can bias resulting estimates. Using data from modules added to the performance monitoring for action surveys in Uganda and Ethiopia in 2018, we compute one-year abortion incidence estimates using the confidante method. We also perform a validation check, using the method to estimate intrauterine device /implant use. Our results revealed implementation problems in both settings. Several of the method's foundational assumptions were violated, and efforts to adjust for these violations either failed or only partially addressed the resulting bias. Our validation check also failed, resulting in a gross overestimate of intrauterine device/implant use. These results have implications more broadly for the potential biases that can be introduced in using third-party reporting of close ties to measure other sensitive or stigmatized behaviors.
INTRODUCTION
Accurate estimates of the incidence of induced abortion are essential in order to track trends in fertility and contraception use. They also provide a necessary foundation for understanding the conditions under which abortions occur, risk factors for severe abortion complications, and unintended pregnancy rates. However, abortion is notoriously difficult to measure. In countries with restrictive abortion laws, information on abortion is not routinely gathered (Singh et al. 2018). In countries where abortion is legal yet highly stigmatized, the clandestine circumstances under which many abortions are performed make official records incomplete. Further, respondents are often reluctant to directly admit to having had an abortion in a survey (Jones and Forrest 1992; Jones and Kost 2007; Lindberg et al. 2020), and efforts to encourage direct reporting through anonymized response methods have failed to consistently generate reliable abortion incidence estimates (Juarez, Cabigon, and Singh 2010; Oliveras and Letamo 2010; Moseson et al. 2017).
As a result of these challenges, researchers have tended to rely on indirect estimation techniques for producing more robust abortion incidence estimates. One common indirect approach is the abortion incidence complications method (AICM) (Singh, Prada, and Juarez 2010). The AICM uses data on patients hospitalized with induced abortion complications in combination with estimates of the proportion of all abortions that do not lead to a facility-based treatment to calculate an abortion incidence rate. However, recent increases in the use of medication abortion likely limit the AICM's ability to accurately measure abortion incidence, as self-managed abortions become safer and reduce interactions with the formal healthcare system.
Another promising set of indirect methods for measuring abortion incidence are social network-based methods that use third-party reporting (TPR) to collect information on abortions within a respondent's social network. TPR methods represent an improvement over the AICM, as they are not reliant on interactions with the health care system. These methods include (1) anonymous third-party reporting (ATPR), which collects information on all close friends (Rossier 2010; Rossier et al. 2006; Sedgh et al. 2011); (2) the best friend approach, which collects information on a respondent's one closest female friend (or relative) (Yeatman and Trinitapoli 2011), and (3) the confidante method, which collects information on two to three women with whom the respondent reciprocally shares personal information (Sedgh and Keogh 2019).1 Based on the proliferation of the use of these methods to measure abortion, with the recent increase in the use of the confidante method, in particular, there is a pressing need to evaluate the assumptions underlying these methods, potential violations of those assumptions, and the resulting biases in abortion estimates.
This paper provides the first critical assessment of the confidante method to measure abortion. We outline six key assumptions behind the confidante method and describe how potential violations of these assumptions can introduce bias to both the numerator and the denominator of these estimates. Using data from modules added to the nationally representative performance monitoring for action (PMA) surveys in Uganda and Ethiopia in 2018, we employ the confidante method to compute one-year abortion incidence estimates, which we then compare to incidence estimates derived from self-reported abortions in the same surveys, as well as the most recent AICM abortion incidence estimate in each country. Ethiopia and Uganda represent different social and legal contexts for abortion; while abortion is largely stigmatized in both countries, safe abortion care is easily accessible in Ethiopia yet highly restricted in Uganda. This contrast provides further insight into how and why violations of assumptions may occur in different settings. We propose and test techniques to adjust for potential sources of bias in the confidante method. We also perform a validation check, using the method to estimate intrauterine device (IUD) and implant use, which can be reliably estimated through direct survey methods. Our findings highlight the serious challenges of using the confidante method to estimate abortion incidence, which has important implications for the use of this method to measure other sensitive and stigmatized behaviors.
BACKGROUND
There is a long history of the use of TPR of close ties to measure hidden behaviors or events. Early examples of this are the sibling method (and its sisterhood subset), which were developed to estimate mortality; respondents are asked for an exhaustive list of siblings (or sisters) born to the same mother, for whom they provide information about gender, age, and survival status (Bicego 1997; Gakidou and King 2006; Graham, Brass, and Snow 1989, Hill and Trussell 1977; Rutenberg and Sullivan 1991; Timæus and Jasseh 2004). Originally proposed by Hill and Trussell (1977), it is now one of the key methods for measuring maternal mortality in countries without accurate vital registration systems and has been included as a module in the Demographic and Health Surveys in 46 countries. Given its widespread use and longevity, there also exists a robust body of research interrogating its potential biases. This has included selection effects through survivor bias, biases introduced from sibship with no surviving siblings, recall errors in deaths and age at death, and reporting errors in sibship listings (Gakidou and King 2006; Helleringer et al. 2014; Masquelier et al. 2021; Stanton, Abderrahim, and Hill 2000; Trussell and Rodriguez 1990). Corrections have been proposed to adjust for these biases, including a weighting adjustment and a corrected sibling survival technique (Gakidou and King 2006; Obermeyer et al. 2010), which has since been criticized for potentially overestimating mortality (Masquelier 2013).
More recently, several indirect social network-based approaches that build off the sibling method have been developed to measure abortion incidence. The general assumptions shared by these methods are that respondents will be more willing to report others’ abortions than to report their own, and respondents’ social networks can be used to generate a surrogate sample. The first application of one such indirect network-based approach was the ATPR method (Rossier et al. 2006). Similar to the sibling method, the ATPR asks for an exhaustive listing of women who share secrets with the respondent and then asks whether each woman had an abortion (Rossier 2010; Rossier et al. 2006; Sedgh et al. 2011). The abortion rate is calculated as the rate among all reported close friends. A key benefit of this method is that information is collected on multiple close ties, creating a large denominator. However, the denominator is sensitive to whether the respondent gives an accurate listing of women who fit the close tie definition, which could potentially bias the ATPR estimate. Previous applications of the ATPR have provided mixed results of its effectiveness; while a 2001 application of ATPR in Burkina Faso produced a rate that was comparable to other estimates in the region at the time, a 2009 study in Burkina Faso as well as a similar study in India produced unreasonably low abortion rates (Rossier 2003, 2010; Sedgh et al. 2011).
The best friend method similarly asks about abortions within respondents’ social networks. However, each respondent is only asked to report on her one closest female friend (or relative) (Yeatman and Trinitapoli 2011). While this method corrects for the potential inaccurate listing limitation of the ATPR method, it results in a much smaller sample size. Also, the assumption that a sample comprised of each respondent's one “best friend” is representative of reproductive-age women may not be defensible if reported “best friends” have different abortion experiences than that of the general population. The best friend method was employed in Malawi, where it yielded higher estimates of abortion than self-reports, suggesting better but possibly incomplete reporting (Yeatman and Trinitapoli 2011).
The confidante method was designed to combine the strengthens of the ATPR and the best bfriend methods while making small adjustments to address their limitations (Sedgh and Keogh 2019). It asks each respondent to think of all of the women they know who would share their secrets with her, and with whom she would also share such secrets (a reciprocally defined relationship). Then, instead of asking respondents to report information on all of these women (as in the ATPR), respondents are only asked to report on a fixed number of women with whom they are the closest.2 Fixing the number of confidantes to a set maximum increases the sample size relative to the best friend method while also precluding respondents from having to produce an accurate list of all women who fit the tie definition. In addition, the ATPR and best friend method allow for the possibility that multiple respondents will report on the same person. If abortion is either negatively or positively correlated with “popularity,” the resulting incidence estimates would be biased. For example, a study on reported close ties in a closed social network study on Likoma Island, Malawi, found popularity bias among men who had multiple sexual partnerships, potentially limiting the utility of this method for estimating that sensitive behavior (Helleringer et al. 2019). The confidante method's stipulation of reciprocity in the tie definition is designed to help diminish this potential for “popular” confidantes to be repeatedly included in the sample.
There has been a proliferation of TPR methods to measure abortions in recent years. In addition to the applications of the ATPR and best friend method in Burkina Faso and Malawi (Rossier et al. 2006; Sedgh et al. 2011; Yeatman and Trinitapoli 2011), the confidante method has been tested broadly, including in Côte D'Ivoire (Bell, Sheehy, et al. 2020), Ghana (Keogh et al. 2020), India (Bell, et al. 2019), Indonesia (Stillman et al. 2020), Kinshasa, DRC (Ishoso et al. 2019), and Nigeria (Bell, Omoluabi, et al. 2020). Given the fact that all three of these methods share several potential biases and limitations that have been well documented in the sibling method literature, an in-depth examination of the methods’ assumptions and associated biases is needed in order to determine the validity of the resulting incidence estimates.
Some recent work has begun to describe the assumptions of the confidante method, many of which are also addressed in this paper (Bell, Shankar, et al. 2020; Sedgh and Keogh 2019; Stillman et al. 2020). However, these previous studies are either missing several key assumptions, do not fully discuss the implications of assumption violations, do not describe how to identify when biases may be present, and/or do not outline limitations in the researcher's ability to adjust for potential biases. Another previous study raised concerns about sampling bias in TPR using a unique complete network dataset, but this work did not look at nonsampling biases or errors that can emerge that are specific to abortion reporting (Helleringer et al. 2019). Our analysis builds off this previous work to comprehensively examine the underlying assumptions associated with the use of TPR of close ties to measure abortion incidence, the biases to which violations in these assumptions could lead, and possible adjustments that can be used to correct for such biases.
Key Assumptions Underlying TPR of Close Ties Methods
In order for TPR of close ties to accurately estimate the incidence of abortion, the method must produce a robust estimation of the behavior of interest (the numerator) and a valid surrogate sample that is representative of the general population (the denominator). To accomplish this, six key assumptions inherent in these methods must be met (Table 1). While the assumptions listed below are described in language specific to the confidante method and abortion measurement, similar assumptions underlie all TPR of close ties methods to measure sensitive behaviors.
| Assumption | Biases created by assumption violations | Methods for identifying violations | |
|---|---|---|---|
| Assumption 1 | Respondents and confidantes share information about their abortions | Study design bias |
|
| Assumption 2 | Respondents will have complete knowledge of their confidantes’ abortions | Transmission bias |
|
| Assumption 3 | Respondents are willing and able to disclose information on confidantes’ abortions in a survey |
Social desirability bias Recall bias |
|
| Assumption 4 | Respondents select confidantes with homophily | Selection bias |
|
| Assumption 5 | Respondents who report no confidantes do not differ systematically from respondents who report any confidantes |
Selection bias Barrier effects |
|
| Assumption 6 | Confidante inclusion in the surrogate sample is independent of their abortion status. |
Selection bias Popularity bias |
|
Measuring the Numerator: Creating an Accurate Indicator of Abortions among Confidantes
Assumption 1.Respondents and confidantes share information about their abortions.
All TPR approaches require that information about the behavior in question is shared between social network ties. This assumption is almost always met, although the degree to which women share information about their abortions may vary based on the tie definition or study context. Prior research has suggested that the highly restrictive nature of abortion in many settings necessitates the sharing of abortion information; respondents and confidantes use their social networks for assistance in accessing abortion services, as these services are often not publicly advertised and may rely on referrals from trusted sources (Rossier 2010; Rossier et al. 2006, 2018; Sedgh et al. 2011). Some have suggested that in settings where abortion is highly stigmatized yet broadly accessible (e.g., Ethiopia or India) there is less need for individuals to share information about their abortions with social network members (Rossier et al. 2018). However, individuals may still share their abortion experiences with close ties for other reasons (emotional support, shared experiences, etc.)
Assumption 2.Respondents will have complete knowledge of their confidantes’ abortions.
It is not sufficient for respondents and confidantes to generally share information about their abortions; respondents must additionally be aware of all abortions that have occurred among their listed confidantes. However, given the highly stigmatized nature of abortion in many settings, this assumption will almost certainly be violated, leading to a phenomenon known as transmission bias (Bernard et al. 2010; Killworth et al. 2006; Maltiel et al. 2015; Salganik et al. 2011). Transmission bias, or incomplete knowledge of abortions within social networks, has been identified as a major limitation in previous ATPR studies (Rossier 2010). The confidante method was designed to reduce the impact of this bias by asking respondents to only think of the women with whom they share “intimate secrets,” thereby increasing the likelihood that respondents will have better knowledge of their confidante's abortions. However, this specification is not sufficient to ensure that respondents have perfect knowledge of their confidantes’ abortions, and it is likely that incidence estimates will be biased towards the null (as overreporting of abortion is unlikely). Any application of this method must therefore make some adjustment to account for transmission bias.
Assumption 3.Respondents are willing and able to disclose information on confidantes’ abortions in a survey.
Irrespective of the completeness of respondent's information on confidante abortions, respondents must be willing to report this information in a survey. Social desirability bias may lead to violations of this assumption, which is a common problem when measuring sensitive behaviors (Tourangeau and Yan 2007). While it is well established that respondents tend to under-report their own *experiences of abortion (Jones and Forrest 1992; Jones and Kost 2007; Lindber g et al. 2020), the central assumption of the confidante method is that social desirability bias is lower when respondents report the abortions of other people rather than their own. While there is some evidence to support this for other sensitive behaviors (Bauman and Fisher 1986; Fisher 1993), it is unclear how far these findings can be extrapolated to abortion.
Further, many applications of the confidante method aim to measure a time-defined incidence of abortion. Therefore, we must also assume that respondents are able to report the date of each confidante abortion with relative accuracy. However, respondents may also have incomplete or imperfect knowledge of when abortions occurred, leading to recall bias. Similar recall biases for the reporting of the age of living siblings and at death have been documented in the sibling method, which downwardly biases mortality estimates (Masquelier et al. 2021). While impactful events may be better remembered, respondents may also incorrectly infer recency from the clarity of the memory (Loftus and Marburger 1983; Sudman and Bradburn 1973). If abortion reporting is subject to this type of telescoping, one-year incidence estimates calculated from reports for the past year could become inflated.
Measuring the Denominator: Producing a Surrogate Sample of Confidantes That Is Representative of the General Population
Assumption 4.Respondents select confidantes with homophily.
Helleringer et al. (2019) identified structural assumptions about underlying social networks that are essential for TPR to produce unbiased estimates. One of these assumptions is that the surrogate sample must be representative of the population of interest, which is assumed to occur through homophily (i.e., individual's tendency to seek out and know others who are similar to themselves). A violation of this assumption will result in homophily bias and create a nonrepresentative sample of confidantes (Helleringer et al. 2019; McPherson, Smith-Lovin, and Cook 2001; Rossier 2010; Rossier et al. 2006).
Assumption 5.Respondents who report no confidantes do not differ systematically from respondents who report any confidantes.
Some respondents may not have any social network members who fit the confidante tie definition and thus contribute zero confidantes to the surrogate sample. In order to produce a robust incidence estimate, one must assume that respondents with zero confidantes do not differ systematically in sociodemographic characteristics, social network attributes, or abortion experiences from respondents with any confidantes. Violations of this assumption may result in the creation of an unrepresentative surrogate sample. Further, violations of this assumption could potentially lead to a biased estimation of abortion incidence due to a phenomenon known as “barrier effects.” Barrier effects are when groups of people have differential propensities to know people in different groups, that is, individuals who have abortions may be more likely to know others who have abortions. In the case of the confidante method, if respondents who report any confidantes have a higher abortion incidence rate than their counterpart respondents with zero confidantes, their corresponding confidantes may also be more likely to have abortions than the general population, ultimately resulting in a confidante incidence rate that is an overestimate of the true rate.
Assumption 6.Confidantes’ inclusion in the surrogate sample is independent of their abortion status.
We assume that respondents will only identify confidantes based on the social-network tie definition provided, regardless of whether the confidante had an abortion. If respondents deliberately include (or exclude) social network members who are known to have had an abortion, the resulting surrogate sample will be biased. For example, research has found that including the word “abortion” in the confidante definition resulted in an overestimation of abortion (Sedgh et al. 2011). Further, independent of a respondent's selection motivations, we assume that a confidante's likelihood of being included in the surrogate sample is not associated with their likelihood of having had an abortion. If some confidantes are more popular (and therefore reported by multiple respondents) and popularity is correlated with abortion, the estimates will suffer from “popularity bias” (Helleringer et al. 2019). In the case of the confidante method, if respondents inappropriately select confidantes based on their abortion status, or some confidantes are more likely to be selected multiple times and this likelihood is correlated with their likelihood of abortion, then the resulting abortion incidence estimate will be unduly biased.
METHODS
Data Sources and Sample
This study utilizes data from an abortion module that the Guttmacher Institute designed and added to the 2018 PMA female surveys in Uganda and Ethiopia (PMA 2021), which was fielded in partnership with Makerere University School of Public Health, Addis Ababa University, and Johns Hopkins Bloomberg School of Public Health. Surveys were conducted face-to-face on Android smartphones using Open Data Kit software. Data collection occurred from April to May 2018 in Uganda and from June to July 2018 in Ethiopia. The sampling plan in both countries was designed to produce a nationally representative sample of women aged 15–49 and relied on a two-stage cluster sampling design. A more detailed explanation of the PMA survey methodology and sampling procedure is provided elsewhere (PMA 2018; Zimmerman et al. 2017).
A total of 4,454 female respondents were sampled in Uganda and 7,690 in Ethiopia. After excluding women who did not consent to participate in the survey (Uganda = 166, Ethiopia = 144), half of the respondents were randomized to be administered the Confidante module (Uganda = 2,089, Ethiopia = 3,725). To identify confidantes, each respondent was asked to think of her female friends or relatives with whom she shares “intimate secrets” and who shares “intimate secrets” with her. There was no mention of secrets as related to sexual activity or reproductive health status, and we did not specifically mention abortion in the consent materials for the study. Eligible confidantes were limited to women with whom the respondent has been in contact in the past year, are between the ages of 15 and 49, and currently live in the country. Respondents were asked to report up to three women who fit this description, each of whom was identified to the interviewer using a fake name. Respondents first reported on the confidante with whom she was most likely to share intimate secrets, and when applicable, the second and third most likely. This process resulted in the identification of 3,268 confidantes in Uganda and 4,612 confidantes in Ethiopia.
The Institutional Review Boards of the Guttmacher Institute, Johns Hopkins Bloomberg School of Public Health, Makerere University, and Addis Ababa University provided ethical approval for the study.
Measures
Abortion was measured among respondents and confidantes. For each confidante, respondents were asked “as far as you know, has [confidante fake name] ever done something that intentionally ended a pregnancy?”3 Response options included “yes, I'm certain,” “yes, I think so,” and “no.” Respondents who replied “yes, I think so” constituted less than 2 percent of the responses across all confidantes in both countries (Online Appendix A). Therefore, “certain” and “probable” responses were collapsed to identify abortions among confidantes. For each reported confidante abortion, respondents were asked for the year in which their most recent abortion occurred. In some cases, respondents did not know the year of their confidante's abortion (5 percent of lifetime confidante abortions in Ethiopia, 8 percent in Uganda; Online Appendix B). If the respondent was not sure, she could choose from the following categories: “less than 1 year ago,” “1 to less than 3 years ago,” “3 to less than 5 years ago,” or “5 or more years ago.” To measure self-reported abortion, respondents were asked if they have ever done anything to successfully end a pregnancy. Respondents who indicated “yes, I succeeded” were coded as ever having had an abortion. Respondents were then asked what month and year their most recent abortion occurred.
Sociodemographic characteristics, including age, educational attainment, and region, were also measured for both respondents and confidantes. Additional sociodemographic characteristics collected only for respondents included household wealth, urban/rural residence, marital status, and parity.
Analysis Plan
We calculated one-year respondent and confidante abortion incidence estimates within each country. For the respondents, the numerator includes all abortions that occurred in the 12 months prior to the date of the interview, and the denominator is the number of respondents in the analytic sample. For confidantes, we did not collect the month that the abortion occurred, only the calendar year. Therefore, the numerator for the confidante incidence rates includes all confidante abortions that occurred in 2017 (the last completed calendar year). If a respondent did not know the calendar year of their confidante's abortion, we included abortions if the respondent reported that the abortion occurred “less than one year ago” (Ethiopia n = 0; Uganda, n = 2). The denominator for the confidante incidence rate is the total number of confidantes. Both the respondent and confidante incidence rates are then multiplied by 1,000 to get the incidence per 1,000 women of reproductive age.4
In order to adjust for the likelihood that respondents do not have perfect knowledge of their confidantes’ abortions (Assumption 2), we calculated a transmission bias adjustment factor. Respondents with any confidantes who also self-reported an abortion were asked whether they told each of their confidantes about their abortion. We then calculated the proportion of respondents who told Confidantes 1–3. This is done separately for each confidante to account for the likelihood that sharing is most common between the respondent and Confidante 1. We then compute an adjustment factor for the confidante abortion estimates that is the inverse of this proportion. (e.g., if 70 percent of respondents who self-reported an abortion told their Confidante 1 about this abortion, then the adjustment factor would be 1.0/0.7 or 1.43. Given that these relationships are meant to be reciprocal, we would interpret this to mean for every Confidante 1 abortion reported by a respondent, there is an additional 0.43 abortions that are not being reported.) We then apply the confidante-specific adjustment factors to inflate the reported abortions in the past year separately among Confidantes 1–3. To get the one-year transmission bias-adjusted abortion incidence estimates among all confidantes, we first sum the inflated number of abortions by each confidante, then divide by the total number of confidantes, and multiply this estimate by 1,000.
Respondent abortion incidence estimates were weighted using the PMA-generated individual sample weights. However, we found evidence that respondents likely did not select confidantes with homophily, in violation of Assumption 4, as there were statistically significant differences in age, education level, and the region between respondents and confidantes in both countries (Online Appendix C). In an effort to partially account for this violation, we used multivariable logistic regression to create poststratification weights so that the confidante samples are nationally representative based on available characteristics. It is important to note that this procedure only adjusts for differences in characteristics that were measured for the confidantes; the reweighted confidante samples may still differ from the underlying populations in other important, yet unmeasured, ways.
Sensitivity Analyses
To determine whether recall bias in reporting of confidante abortion timing was present (in violation of Assumption 3), we calculated three-year incidence rates using the same methodology for determining the one-year rates (36 months from interview date for the respondent, abortions that occurred less than three years ago or in calendar years 2015, 2016, and 2017 for confidantes), and then divided these estimates by three to create annualized one-year abortion incidence estimates. We then compare the annualized estimate to the directly reported confidante past one-year incidence estimate.
While we began with a nationally representative sample of respondents, we also observed that not all respondents reported having at least one confidante. This effectively removes these respondents’ social networks from the sample, increasing the likelihood that the confidante sample will be nonrepresentative. In order to assess whether barrier effects related to women's experiences with abortion are present (in violation of Assumption 5), we estimated unadjusted odds ratios to determine whether there were key differences in respondent abortion rates and sociodemographic characteristics based on whether or not they reported any confidantes.
Validity Check
To test the overall performance of the method, we estimated the prevalence of another hidden reproductive health behavior: IUD or implant use among confidantes. We chose IUD/implant use as there are valid external estimates with which to compare the confidante estimate. In addition, information about IUD/implant use would need to be disclosed between respondents and confidantes in a similar manner to abortion, as opposed to respondents learning of this use by observation. We asked respondents to report their confidantes’ current use of IUDs or implants and calculated a corresponding Confidante prevalence rate. We hypothesize that stigma associated with IUD/implant use is much lower than abortion in both settings. As such, using a similar method for the respondents who self-reported abortions, we asked current IUD/implant users whether they reported this use to each of their confidantes. We then used this information to additionally adjust the confidante method produced IUD/implant estimates for transmission bias. We then compare the unadjusted and adjusted IUD/implant estimates to the self-reported prevalence calculated from the PMA survey as well as to the most recent estimates from the Demographic and Health Survey (DHS) in Ethiopia and Uganda.
All analyses were performed using Stata version 16.0 (StataCorp LP, College Station, TX).
RESULTS
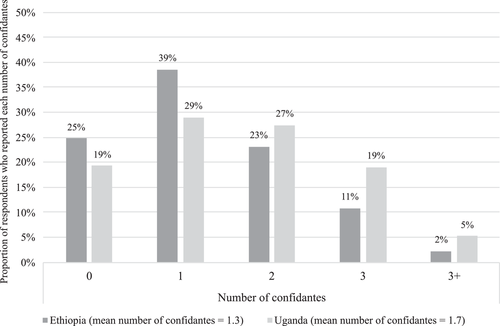
Approximately 25 percent of respondents in Ethiopia and 19 percent of respondents in Uganda reported having zero confidantes. The average number of confidantes per respondent among all respondents was 1.3 in Ethiopia and 1.7 in Uganda (Figure 1). Confidante age, educational attainment, and region were similar to their corresponding respondents in each country, as a result of the poststratification weighing (Table 2).
| Ethiopia | Uganda | |||||||
|---|---|---|---|---|---|---|---|---|
| Respondents (N = 3,725) | Pooled confidantes (N = 4,612) | Respondents (N = 2,089) | Pooled confidantes (N = 3,268) | |||||
| Age, mean (SD) | 27.9 | 9.3 | 27.1 | 8.9 | 27.8 | 9.0 | 28.6 | 9.1 |
| Education, % (n) | ||||||||
| Never | 38.2 | 1,107 | 34.6 | 1,102 | 9.9 | 257 | 10.0 | 433 |
| Primary | 38.9 | 1,314 | 39.0 | 1,524 | 53.5 | 1,127 | 50.0 | 1,407 |
| Secondarya | 14.5 | 737 | 16.7 | 1,114 | 29.1 | 569 | 35.8 | 1,195 |
| Postsecondaryb | 8.5 | 560 | 9.7 | 835 | 7.5 | 135 | 4.1 | 125 |
| Residence, % (n) | ||||||||
| Urban | 25.3 | 1,929 | n/a | n/a | 22.8 | 578 | n/a | n/a |
| Rural | 74.7 | 1,796 | 77.2 | 1,511 | ||||
| Union/marital status, % (n) | ||||||||
| Married/cohabiting | 64.2 | 2,157 | n/a | n/a | 63.7 | 1,323 | n/a | n/a |
| Formerly married | 8.9 | 389 | 12.0 | 253 | ||||
| Never married | 27.0 | 1,178 | 24.3 | 513 | ||||
| Parity, % (n) | ||||||||
| No children | 35.6 | 1,490 | n/a | n/a | 25.9 | 554 | n/a | n/a |
| 1–2 | 22.8 | 954 | 27.9 | 570 | ||||
| 3–5 | 24.9 | 813 | 27.6 | 581 | ||||
| 6+ | 16.8 | 468 | 18.6 | 383 | ||||
- NOTES: Weighted proportions with unweighted Ns shown. Ns may not sum to total N due to missing data. Valid percentages shown.
- a Secondary includes: secondary (ET); ‘O’ level, ‘A’ level (UG).
- b Postsecondary includes: technical, higher (ET); tertiary, university (UG).
Figure 2 displays the proportion of respondents who reported their abortions to their respective confidantes. Contrary to our initial hypothesis, reporting did not decline in a linear way from Confidante 1 to Confidante 3 in either country, and the proportion of respondents who reported their abortions to their confidantes ranged from 41.7 percent to 56.8 percent. (See Online Appendix D for the transmission bias calculations.)
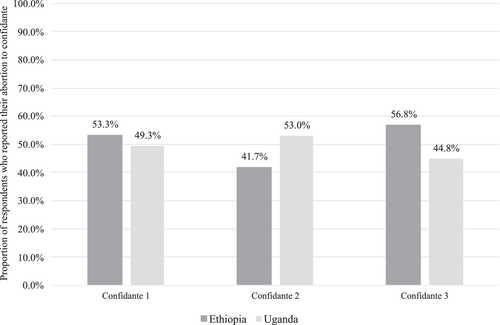
Figure 3 shows one-year abortion incidence rates among respondents and confidantes as well as the most recent AICM estimate in each country. In Ethiopia, the unadjusted confidante abortion rate was almost double that of the respondents, though confidence intervals for the two estimates overlap (confidantes: 7.1 per 1,000, 95 percent CI: 4.6–11.0; respondents: 4.3 per 1,000, 95 percent CI: 2.5–7.3). After adjusting for transmission bias, the confidante abortion rate increased to 18.6 per 1,000 (95 percent CI: 12.0–28.8). Both the unadjusted and transmission bias-adjusted confidante rates were considerably lower than the 2014 AICM rate for Ethiopia (28.0 per 1,000, UI: 23.5–33.0) (Moore et al. 2016). In Uganda, the difference between respondent and unadjusted confidante incidence rates was much larger, with the confidante rate being almost five times larger than the respondent rate (confidantes: 39.5 per 1,000, 95 percent CI: 31.7–49.1; respondents: 8.6 per 1,000, 95 percent CI: 4.7–15.8). While the unadjusted confidante rate is almost identical to the 2013 Uganda AICM incidence rate (39.0 per 1,000, UI: 24.0–55.0) (Prada et al. 2016), the transmission bias-adjusted rate appears unrealistic high, at almost double that of the most recent AICM estimate (76.8 per 1,000, 95 percent CI: 61.7–95.4).
Sensitivity Tests
Table 3 displays three-year and annualized one-year confidante abortion incidence estimates. In Ethiopia, the reported one-year confidante estimate is similar to the annualized estimate (6.1 per 1,000, 95 percent CI: 4.7–8.0). In Uganda, the one-year confidante estimate is almost twice as large as the annualized one-year estimate (24.3 per 1,000, 95 percent CI: 21.0–28.2), suggesting that reporting errors may have occurred when respondents reported the timing of their confidantes’ abortions.
| Ethiopia | Uganda | |||||
|---|---|---|---|---|---|---|
| Rate | 95% CIs | Rate | 95% CIs | |||
| One-year | 7.1 | 4.8 | 10.6 | 39.5 | 31.9 | 48.9 |
| Three-year ratea | 18.4 | 14.2 | 23.9 | 73.0 | 62.9 | 84.5 |
| Annualized one-year | 6.1 | 4.7 | 8.0 | 24.3 | 21.0 | 28.2 |
- NOTES: Incidence estimates adjusted using poststratification rates. Estimates have not been adjusted for transmission bias.
- a Reflects confidante abortions reported to have occurred in 2015–2017 calendar years.
In both countries, older age, lower levels of education, and having more children were significantly associated with reporting zero confidantes (Table 4). In Ethiopia, rural residence, lower household wealth, and being married were also associated with having no confidantes. There were no statistically significant differences in one-year or three-year self-reported abortions for respondents in Ethiopia based on whether the respondents reported any confidantes. In Uganda, self-reporting an abortion was negatively associated with reporting zero confidantes, although unadjusted odds ratios (ORs) were not statistically significant. Although not statistically significant, the one-year incidence rate among respondents in Uganda reporting at least one confidante was almost double that of respondents reporting zero confidantes (9.4 per 1,000 vs. 5.3 per 1,000, p = 0.102; results not shown). An even larger gap exists for the three-year incidence estimates (15.5 per 1,000 vs. 6.3 per 1,000, p = 0.051).
| Ethiopia | Uganda | |||||
|---|---|---|---|---|---|---|
| (N = 3,725) | (N = 2,089) | |||||
| uOR | 95% CIs | uOR | 95% CIs | |||
| Self-reported abortion | ||||||
| Respondent abortion in last 12 months | 0.79 | 0.26 | 2.38 | 0.22 | 0.03 | 1.63 |
| Respondent abortion in last 36 months | 0.98 | 0.48 | 2.02 | 0.26 | 0.06 | 1.11 |
| Residence | ||||||
| Urban | ||||||
| Rural | 1.51 | 1.30 | 1.75 | 0.89 | 0.70 | 1.13 |
| Wealth Quintile | ||||||
| Lowest quintile | ||||||
| Lower quintile | 0.94 | 0.72 | 1.23 | 1.01 | 0.73 | 1.41 |
| Middle quintile | 0.72 | 0.55 | 0.95 | 0.83 | 0.59 | 1.18 |
| Higher quintile | 0.73 | 0.56 | 0.94 | 0.81 | 0.57 | 1.15 |
| Highest quintile | 0.51 | 0.41 | 0.64 | 1.11 | 0.81 | 1.51 |
| Age | 1.03 | 1.03 | 1.04 | 1.02 | 1.01 | 1.03 |
| Union/marital status | ||||||
| Married/cohabiting | ||||||
| Formerly married | 1.50 | 1.19 | 1.88 | 1.24 | 0.90 | 1.71 |
| Never married | 0.56 | 0.47 | 0.67 | 0.81 | 0.62 | 1.06 |
| Education | ||||||
| Never | ||||||
| Primary | 0.40 | 0.33 | 0.48 | 0.98 | 0.70 | 1.36 |
| Secondarya | 0.28 | 0.22 | 0.35 | 0.67 | 0.46 | 0.98 |
| Postsecondary b | 0.25 | 0.20 | 0.33 | 0.79 | 0.47 | 1.35 |
| Parity | ||||||
| No children | ||||||
| 1–2 | 1.48 | 1.22 | 1.80 | 0.93 | 0.69 | 1.26 |
| 3–5 | 2.21 | 1.82 | 2.69 | 0.98 | 0.72 | 1.32 |
| 6+ | 2.16 | 1.71 | 2.72 | 1.39 | 1.01 | 1.90 |
- NOTES: Results in bolded indicate statistical significance at p < 0.05.
- a Secondary includes: secondary (ET); “O” level, “A” level (UG).
- b Postsecondary includes: technical, higher (ET); tertiary, university (UG).
Validity Check
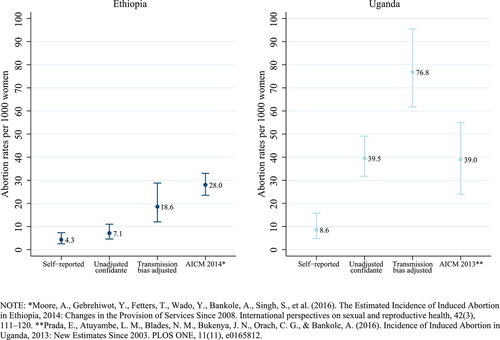
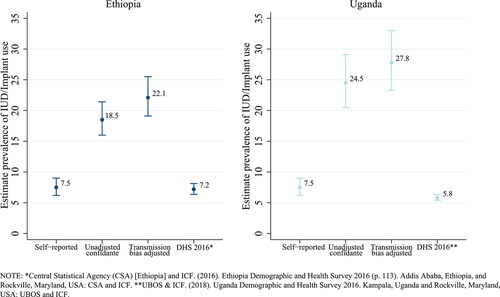
In Ethiopia, the most recent DHS estimate for current IUD/implant use is 7.2 percent (95 percent CI: 6.4–8.1) (CSA and ICF 2016), and respondent reports from the 2018 PMA survey were nearly identical to the DHS (7.5 percent, 95 percent CI: 6.2–9.0) (Figure 4). In contrast, the unadjusted confidante IUD/implant use estimate in Ethiopia was more than double that of the DHS or direct report estimates (18.5 percent, 95 percent CI: 16.0–21.4). We observed a similar pattern in Uganda; the 2016 DHS and 2018 PMA estimates for current IUD/implant use were similar to each other (DHS = 5.8 percent, 95 percent CI: 5.4–6.3; PMA = 7.5 percent, 95 percent CI: 6.2–9.0) (UBOS and ICF 2018), and the unadjusted confidante IUD/implant estimate was substantially larger than either the DHS or PMA rate (24.5 percent, 95 percent CI: 20.5–29.1). IUD/implant use appears to be a more visible SRH behavior than abortion, with 54 percent -88 percent of respondents reporting their current IUD/implant use to their corresponding confidante (Figure 5). As such, adjusting for transmission bias only slightly elevated the confidante IUD/implant use estimates (Ethiopia: 22.1 percent, 95 percent CI: 19.1–25.5; Uganda: 27.8 percent, 95 percent CI: 23.3–33.0). (See Online Appendix D for IUD/implant transmission bias calculations.) However, our validity check illustrates that the confidante method dramatically overestimates the prevalence of IUD and implant use in both countries.

DISCUSSION
The results of this study provide important insights into the use of the confidante method to measure abortion incidence in clandestine settings. One of the largest difficulties in assessing new methods for measuring abortion incidence is that there is no gold standard against which to compare the estimates to fully validate the results. However, the results from this study nevertheless suggest that the confidante method is not a good solution to the challenges of abortion measurement. Several of the method's foundational assumptions were violated, and our analysis revealed important biases in both the numerator and denominator for producing the confidante estimate, as well as variation in these biases between the two countries. Efforts to correct for violations of the key assumptions either failed or only partially addressed the resulting biases. It is not surprising, then, that our external validity check revealed that the confidante method failed to produce a valid estimate of IUD/implant prevalence in either country.
Evaluation of Assumptions Associated with the Numerator
In both study settings, it appears that Assumption 1 (respondents and confidantes share information about their abortions), was not violated; it is clear that at least some transfer of abortion information is occurring, given the frequency and certainty with which respondents report confidante abortions. However, in line with our a priori hypothesis, our results suggest that Assumption 2 (respondents have complete knowledge of their confidantes’ abortions) was violated. One indication of this is that respondents only disclosed their own abortions to approximately half of their confidantes. Unfortunately, there are several major methodological limitations to accurately measure the magnitude of this bias. When designing our method for measuring transmission bias, we hypothesized that most respondents learned of confidante abortions directly from their confidante, as the social tie definition stipulated that the respondent-confidante dyad reciprocally shares intimate secrets. As such, we asked respondents if they told their confidante directly about their abortion. However, it may be that individuals learn of others’ abortions indirectly through other social network members. Further, even if we had been able to modify our measure of transmission to capture these indirect instances of abortion information sharing, which may partially reduce potential measurement error, respondents could still be unaware of all instances of indirect knowledge transfer. If this type of indirect information sharing is common, it may have inappropriately inflated our transmission bias adjustment factors.
In addition, our measure of transmission bias likely suffered from selection bias; we were only able to measure abortion information transmission among women who disclosed their abortion in the survey. Women who self-report abortions in research settings may also be more or less likely to disclose their abortions to their close confidantes, which would introduce error into our measurement of transmission bias. Finally, there is no way to validate our method for measuring transmission bias or test for the magnitude of the concerns outlined above. Previous confidante method studies have used an alternative approach, where respondents’ certainty about their confidantes’ abortions is used as a proxy for transmission bias, arguing that the inclusion of “less certain” abortions accounts for the incomplete transmission of abortion information (Bell, Shankar, et al. 2020). However, this method is unlikely to appropriately adjust for transmission bias, as it cannot account for abortions for which the respondent is completely unaware. Future research is needed to better understand how abortion information is transmitted within social networks and how transmission varies across cultural contexts in order to develop more robust methods for measuring transmission bias among confidantes.
Although transmission bias was measured in a standardized way in both Ethiopia and Uganda, adjusting for this bias produced very different results in the two countries. In Uganda, the transmission bias-adjusted abortion rate was improbably high. Conversely, the adjusted abortion rate in Ethiopia was lower than the AICM estimate, suggesting it was too low if we consider the AICM estimate to be the most valid measure of abortion with which to compare. Some of this variation may be due to differences in the cultural contexts of Ethiopia and Uganda. For example, it may be that indirect sharing of abortion information is more or less common based on underlying levels of abortion-related stigma, norms around gossip, and other factors. In the case that indirect abortion information sharing is rare, our method of measuring transmission error would be less biased. Further, if women who self-report abortions differ between the study contexts, the precision of our method for estimating transmission error could similarly vary in Ethiopia and Uganda.
Our differing results after adjusting for transmission bias may also be evidence of a much larger concern: even when transmission error is accurately measured, it requires that the unadjusted abortion incidence estimates are not unduly biased. In this study, we found that other foundational assumptions were indeed violated (described in detail below), resulting in the inaccurate measurement of the unadjusted abortion rates. In this case, even if transmission bias is accurately measured, adjusting incidence estimates for transmission bias will amplify other sources of bias.
Assumption 3 addresses respondents’ willingness and ability to accurately disclose the confidantes’ abortions of which they were aware. Our sensitivity test results from Uganda, which showed large differences between the unadjusted one-year and annualized one-year abortion incidence rates, suggest that respondents likely had difficulty accurately reporting abortion information. Similar results were found in a study in Ghana using the confidante method, where abortion rates in the past year were over twice as high as those estimated occurring one to two years ago (Keogh et al. 2020). This may be evidence of telescoping, with respondents inappropriately including some confidante abortions as occurring “in the past year.” Further, a recent US-based study found that accurate abortion reporting varies by length of recall (Lindberg and Scott 2018), which could also explain the differences between one and three-year rates. One possible solution to this reporting issue is to calculate one-year annualized abortion rates from three or five-year rates, the one done by Keogh et al. (2020). However, before this technique is employed, a better understanding of the extent to which telescoping and recall bias influence the reporting of confidante abortion in a particular setting is needed. For example, if higher abortion reporting in the past year is due to more accurate recall, then calculating an annualized abortion incidence rate from the past three years would result in an underestimation of abortion incidence.
While the Uganda results indicate that respondents may not be able to report confidante abortions with the necessary accuracy, the results from Ethiopia suggest that respondents may not be willing to report all available confidante abortion information. The directly reported respondent abortion rate was improbably low, and the unadjusted confidante rate was only slightly higher. While this could suggest that transmission error plays a much larger role in Ethiopia, meaning that respondents were simply less aware of their confidante's abortions, the highly stigmatized nature of abortion in Ethiopia may have made confidante abortion reporting more sensitive to social desirability bias (Rossier et al. 2018). Recent work supports this notion; in Java, Indonesia, and Rajasthan, India, confidante abortion rates were implausibly low when compared to other abortion estimates for those countries, which were both similarly attributed to respondents’ willingness to report confidante abortions (Bell, Shankar, et al. 2020; Stillman et al. 2020). However, until there is an accurate measure of abortion visibility in Ethiopia, it is impossible to determine whether transmission error, willingness to report known confidante abortions, or some combination of the two is driving this study's improbably low abortion incidence rates.
Differences in abortion reporting in Uganda and Ethiopia highlight the role that cultural contexts likely play in TPR. The violations described above point to the need for formative research to investigate the appropriateness and design of the confidante method in specific study settings before it is implemented widely. This formative research should examine the extent to which Assumptions 1–3 may be violated, as well as provide culturally specific insight into nuances in the language used to define a “confidante” or discuss abortion in a given setting. To date, many applications of the confidante method, including the ones described in this paper, have not conducted formative research specifically designed to answer these questions and concerns. This is a missed opportunity to evaluate the appropriateness of this method and/or improve its implementation in a particular setting.
Evaluation of Assumptions Associated with the Denominator
This study found extensive violations of assumptions associated with the denominator, likely resulting in unrepresentative surrogate samples in both countries. First, when we compare the confidante sample to respondents on key sociodemographic characteristics, we found significant differences between the pooled confidante samples and the nationally representative sample of respondents, violating Assumption 4. Other recent applications of the confidante method that used similar methodologies to our study also reported homophily assumption violations; systematic differences between nationally representative samples of respondents and their corresponding confidante samples were observed in Cote D'Ivoire, Ghana, Indonesia, and Nigeria (Bell, Shankar, et al. 2020; Keogh et al. 2020; Stillman et al. 2020). All of these recent studies employed recommendations from Sedgh and Keogh (2019) aimed at improving the accuracy of abortion reporting through TPR; requiring reciprocity of intimate secret sharing was meant to improve the likelihood of accurate and complete abortion reporting and limiting the number of reported confidantes was meant to reduce biases associated with accurately reporting an exhaustive list of all women who fit the confidante definition (Sedgh and Keogh 2019). While the underlying premise behind the confidante method is that it can produce representative estimates due to homophily, the results from this recent set of studies raise serious questions about whether the confidante method is an improvement on other TPR approaches due to its inability to generate a representative surrogate sample.
To this point, the findings from ours and other recent studies are in contrast to prior work by Helleringer et al. (2019), which found that the surrogate sample of friends generated through TPR was comparable to the respondent sample. Further, an ATPR study in Burkina Faso from 2008 found that respondents and reported confidantes were similar in age and education level, but not region (Rossier 2010; Sedgh et al. 2011). The lack of homophily in the confidante method compared to previous TPR/ATPR studies may be due to different tie definitions (including the geographic spread, contact frequency, and reciprocity) as well as the confidantes fixed-degree design that limits the number of alters reported.
We attempted to address the violation of Assumption 4 by creating adjusted confidante weights. Despite this, our confidante samples may still be unrepresentative, as we could only adjust for a limited set of characteristics that were measured in the survey (e.g., region, education, and age). One solution to this problem is to collect more data on confidante characteristics, and future research should investigate whether this approach can further improve the weighting adjustment, or whether a different tie definition may be necessary to generate accurate incidence estimates.
Another cause of the unrepresentativeness of the surrogate confidante sample is systematic differences between respondents who report zero versus any confidantes (Assumption 5); respondents with no confidantes were more likely to be married, have children, be less educated, and live in a household with less wealth than respondents with at least one confidante. This suggests that “zero confidante” respondents are more socially marginalized, and therefore a similar group of women is likely “missing” from the confidante sample. This is a major limitation of the confidante method in measuring abortion incidence; socially isolated and/or marginalized women will likely always be underrepresented due to the social connectedness necessary to be included in the confidante sample. Some previous research has suggested that these women may have different abortion experiences, and thus their exclusion would bias results. For example, qualitative research in Zambia has suggested that networked women may be better able to access abortion services (Coast and Murray 2016). Without accounting for this type of selection bias, resulting estimates of abortion might overestimate abortion incidence or overly represent safer abortion experiences. Before the confidante method can be used to accurately measure abortion, it is imperative that future work address how to reduce or adjust for this type of selection bias.
Previous work has identified the existence of this type of bias in other social network–based incidence studies, including the problem of the “zero female respondent” in the sibling method (Gakidou and King 2006; Masquelier 2013). Gakidou and King (2006) proposed a weighting adjustment to correct this problem in measuring mortality. While this approach has been adapted by other confidante method studies (Bell, Omoluabi, et al. 2020; Bell, Sheehy, et al. 2020; Keogh et al. 2020), we do not believe it is appropriate to use with the confidante method, in its current form, for abortion measurement. The technique adjusts for “missing” confidantes and is intended to address the problem that respondents who report zero confidantes are not represented in the surrogate sample. In this approach, “missing” confidantes are added to the surrogate sample by assuming that each respondent who reported zero confidantes has one confidante who shared their characteristics (i.e., assuming perfect homophily). Next, the relationships between reported confidante abortions and other respondent and confidante characteristics are used to predict the probability that each “missing” confidante had an abortion (Bell, Shankar, et al. 2020).
While the issue of “missing” confidantes certainly biased the abortion incidence estimates produced in this study, we did not attempt to adjust for this bias using a similar approach, as we find that adjustments to the sample in this way likely introduce a number of additional biases of unknown magnitude. First, by assigning the “missing” confidantes the characteristics of the corresponding respondent, one must assume perfect homophily between the respondents and this group of confidantes. However, in both Ethiopia and Uganda, we did not observe homophily between respondents and confidantes, and as such, it is not defensible to assume that there was homophily between respondents who reported zero confidantes and an imputed confidante. Further, this approach assumes that the relationship between reported confidante abortions and corresponding respondent/confidante characteristics will be similar for the missing group of socially marginalized confidantes. However, the very nature of their marginalization may also make them more or less likely to have had an abortion, potentially invalidating this assumption. Finally, in both Uganda and Ethiopia, a sizeable proportion of respondents reported zero confidantes, meaning that using this approach would have amounted to imputing approximately 20 percent of the data used to estimate abortion incidence. Given the fact that this imputation approach requires two substantial assumptions that are not supported by the available data, it seemed untenable to produce estimates when a large portion of the data was imputed and not observed. Other studies using this adjustment technique have imputed even larger proportions of their data, ranging from one-third in Ghana (Keogh et al. 2020) to over 50 percent in Nigeria (Bell, Omoluabi, et al. 2020; Bell, Sheehy, et al. 2020), and interpretations of the resulting incidence estimates should be made with caution.
It is difficult to tell whether Assumption 6 (respondents will select confidantes independently of their abortion status) was held or violated. A recent confidante method study in Ghana found that this assumption was likely violated, which may have inadvertently inflated the resulting abortion incidence estimate (Keogh et al. 2020). In that study, the researchers theorize respondents were primed to think of abortion while they were selecting their confidantes, which possibly led respondents to purposely select confidantes who had previous abortion experiences. While it is difficult to assess whether this assumption was violated in our current study, our study design likely reduced the probability that this occurred; we did not mention abortion previously in the survey, and we did not mention sexual health in the description of the kinds of information confidantes should share with each other. However, we do not know how respondents may have interpreted the phrase “intimate secrets”; some respondents may have interpreted this to mean secrets related to sexual or reproductive matters, including abortion. Further, the logic underpinning the confidante method suggests that stigmatized and sensitive personal information is only disclosed between close social ties. However, it is possible that the very act of sharing abortion information may cause individuals to consider others as “confidantes” according to the study definition of sharing “intimate secrets” when they may not have otherwise considered the relationship to be a close tie. The extent to which this may be occurring represents a violation of Assumption 6.
In light of the extensive violations of the assumptions associated with the denominator, which likely biased the surrogate sample towards women who were more socially connected and engaged in more diverse fertility regulation practices, it may not be surprising that our validation check failed, with the confidante method resulting in a gross overestimate of IUD and implant use. Given that abortion is chronically underreported, a common trend in the field of abortion measurement is to assume that the highest estimate in a given setting is likely the least biased. However, our validation check suggests that the concerns with measuring the denominator may lead the confidante method to overestimate abortion incidence. We strongly caution against the interpretation of a confidante method–produced abortion incidence estimate as the most accurate solely based on its greater magnitude.
This study outlined many weaknesses of the confidante method. However, efforts to seek solutions to these problems are called for due to the potential to use the confidante method to collect background characteristics of members of the hidden population as well as additional information related to the sensitive behavior under study (Sedgh et al. 2011; Sedgh and Keogh 2019). For example, applications of the confidante method have contributed valuable insight into the safety of induced abortion in Nigeria, Cote d'Ivoire, and Rajasthan, India (Bell et al. 2019). Even though the safety estimates derived from this method are likely biased, this work is still essential to the design of policies and programs for addressing the needs of individuals seeking abortion in these countries. This benefit differentiates the method from other indirect methods for measuring abortion, such as the network scale-up method, which can only produce an overall estimate of incidence (Sully, Giorgio, and Anjur-Dietrich 2020). This presents an opportunity for further methodological improvements; the more the biases associated with the confidante method can be quantified and adjusted for, the more readily this method can be used to understand sociodemographic differences in risk factors associated with sensitive behaviors.
CONCLUSIONS
The confidante method, as implemented in this study, is likely unsuitable for the accurate measurement of abortion incidence. Our analysis revealed several major limitations as well as pervasive violations of key assumptions. Some of this failure may have to do with the behavior in question; abortion is notoriously challenging to measure, and it may be particularly sensitive to the biases we observed in measuring the numerator. Given the variability in abortion stigma across the setting, violations of key confidante method assumptions may be particularly sensitive to the cultural context where the study is implemented. To address these concerns, it is imperative that future studies first conduct formative research to understand the appropriateness of using the confidante method to measure abortion in a given setting, as well as how the method should be implemented. This formative research should investigate several facets, including levels of abortion-related stigma in the study-specific context, how information is shared within social networks to better estimate the visibility of abortion, the most appropriate definition of a social tie to elicit accurate reporting, the cultural and social norms around disclosing abortion information, and the types of details that respondents might be able to report on about their confidantes’ abortions.
Our results also revealed larger problems with the basic structural assumptions associated with the creation of the surrogate sample. Violations of assumptions associated with the denominator are pervasive in this study, exist regardless of cultural context, and are more difficult to address with adjustments. This finding is more problematic than the biases observed in the numerator, as it has implications beyond the use of the confidante method to measure abortion and extends to other TPR approaches for measuring hidden or stigmatized behaviors. Major concerns shared across these approaches are the sensitivity of estimates to social-tie definitions and violations of the assumption of homophily. For example, the success of the sibling method may stem from the clearly defined nature of the sibling tie, while the confidante method definition of “secret sharing” was likely too interpretive and/or too restrictive, resulting in the large proportions of respondents who reported zero confidantes and an inappropriate surrogate sample more prone to biases. Future research is needed to thoroughly investigate the extent to which differences in key features that distinguish TPR methods, including definitions of social tie relationships and numbers of social network members selected, result in unduly biased estimates of sensitive behaviors. In addition, it is important for future research using TPR approaches to include external validation tests in order to better evaluate the robustness of the resulting estimates. Understanding the magnitude and direction of biases associated with the TPR is essential before the generated estimates can provide insight into the incidence of hidden or sensitive behaviors. In light of the considerations outlined in this paper, we believe this future work is needed and warranted. However, until that work has identified vast improvements to the method, abortion incidence, and safety estimates generated using the confidante method should not be considered valid or accurate.
CONFLICT OF INTEREST DISCLOSURE
The authors declare no conflicts of interest.
ETHICS APPROVAL STATEMENT
The Institutional Review Boards of the Guttmacher Institute, Johns Hopkins Bloomberg School of Public Health, Makerere University, and Addis Ababa University provided ethical approval for the study.
PATIENT CONSENT STATEMENT
Informed consent to publish anonymized data from the research was obtained from all participants recruited to the study.
Open Research
DATA AVAILABILITY STATEMENT
The data that support the findings of this study are openly available from Performance Monitoring and Accountability at https://www.pma2020.org/request-access-to-datasets.
REFERENCES
ACKNOWLEDGMENTS
This work was supported by The David and Lucile Packard Foundation under Grant 2017-66627, 2019-69000, 2020-69738; an anonymous foundation; and The William and Flora Hewlett Foundation under Grant 2017-6475. The views expressed are those of the authors and do not necessarily reflect the positions and policies of the donors.
- 1 Nonbinary individuals, transgender men, and people of other genders are capable of becoming pregnant and have abortions. However, the surveys we discuss in this paper that have implemented ATPR, the best friend method, and the confidante method use recruitment strategies that rely on respondents self-identifying as cisgender female or cisgender women, as well as social tie definitions that use the terms “female” and “women” to define which social network members can be included in the surrogate samples. As such, throughout this paper, we refer to respondent and surrogate samples as being composed of women.
- 2 Recent applications of the confidante method have limited this number to two or three close ties (Bell, Shankar, et al. 2020; Keogh et al. 2020; Stillman et al. 2020).
- 3 Other studies using the confidante method have used more expansive definitions of abortion to include actions around period regulation (i.e., doing something to bring on menstruation at a time when the respondent thought she was pregnant) (Bell, Shankar, et al. 2020; Keogh et al. 2020; Stillman et al. 2020).
- 4 In order to ensure that reporting reliability did not diminish with each subsequent confidante, we first computed one-year incidence estimates separately among Confidantes 1-3 (Online Appendix B). After determining that abortion incidence did not dramatically decline across confidantes, we pooled all confidantes together to compute final one-year incidence estimates for the full confidante sample.