Treatment of post-traumatic stress disorder in people with dementia: a structured literature review
Field of journal: Dementia Care and Epidemiology, BPSD and Non-pharmacological Therapy
Abstract
Post-traumatic stress disorder (PTSD) is associated with cognitive dysfunctions and is an independent risk factor for dementia. A recent study has found the prevalence of PTSD in people with dementia is 4.7%–7.8%. However, little is known about the effectiveness of PTSD treatment for people with dementia. The primary aim of the current study is to review previous studies on the treatment of PTSD in people with dementia. A structured literature review was performed using a ‘Preferred Reporting Items for Systematic Reviews and Meta-Analyses’ analysis in PubMed, Embase, PsycINFO and CINAHL. Two independent researchers screened titles and abstracts. The inclusion criteria were: PTSD symptoms present, diagnosis of dementia, PTSD treatment form described and effects of the treatment mentioned. Articles that matched these criteria were included and content and quality were analyzed. We included nine articles, all case reports, with a total of 11 cases. The discussed treatment options are eye movement desensitisation and reprocessing (EMDR) (n = 3), prolonged exposure (n = 1), cognitive behavioural therapy (n = 1) and pharmacological treatment (n = 4). All articles reported a positive effect of the intervention on several monitored symptoms. Evidence for positive effects and feasibility of EMDR were most reliable, and it was applied in two articles of sufficient quality published in 2018 and 2019. EMDR ‘on-the-spot’ was described with positive effect in one article in which three cases were discussed. The quality of included papers ranged from insufficient to sufficient. This review shows that people with PTSD and dementia can benefit from PTSD treatment. EMDR, prolonged exposure, acceptance and commitment therapy and pharmacological treatment are applicable in this population. EMDR treatment is most described in this population (n = 5) and shows positive results, and the studies are of sufficient quality (n = 3). Further research in the form of a randomised controlled trial is required to study the effectivity of different treatment interventions in this population.
INTRODUCTION
Post-traumatic stress disorder (PTSD) is a psychiatric condition that may develop after exposure to a traumatic event.1 Main symptoms of PTSD are the onset of intrusive symptoms after a traumatic event, hyperarousal, changes in mood or cognition and avoidance of trauma-associated triggers.2 The lifetime prevalence in the general population of PTSD is 7%–8%.3 People with PTSD experience a high burden of disease with a higher risk of suicide attempts and anxiety compared to people without PTSD.4 There is also a high caregiver burden related to the increased symptom severity in PTSD.5, 6 Effective treatments for PTSD can improve quality of life.7-9
In people with dementia, the combination of neurodegeneration and decreased cognitive reserve may increase the reactivation of traumatic memories and thereby elicit PTSD symptoms.10, 11 Although research on the prevalence of PTSD in people with dementia is scarce, a recent literature review described a prevalence of 4.7%–7.8%, based on three studies in veterans.12 It appears that in people with dementia, PTSD is difficult to recognise and a trauma history is often not documented.13 In addition, people with dementia and PTSD can show a variety of symptoms often associated with neuropsychiatric symptoms of dementia and not as symptoms of PTSD.14 Examples are verbal agitation, physical aggression, flashbacks, fear and nightmares.15, 16 For neuropsychiatric symptoms seen in people with dementia the treatment options reported are broad with low grades of evidence.17 A thorough investigation of the possible cause of the symptoms is required as the symptoms are often mistreated.18, 19 We believe recognising PTSD in this population can provide more effective treatment options. Currently caregivers are often not trained to recognise PTSD symptoms in people with dementia due to lack of available literature and diagnostic tools.12 To adequately reduce the symptoms of PTSD it is important to diagnose and adequately treat PTSD. This review focuses on the treatment options for PTSD in people with dementia.
Several treatment options exist for PTSD in adults and elderly people without dementia. For example, substantial empirical evidence exists for the effectiveness of eye movement desensitisation and reprocessing (EMDR) and (trauma-focused) cognitive behavioural therapy (CBT) in reducing PTSD symptoms.9, 20-22 Studies focusing on older people with dementia are scare. The purpose of this literature review is to systematically summarise the available literature on the treatment of PTSD in people with dementia.
METHOD
Data sources and search
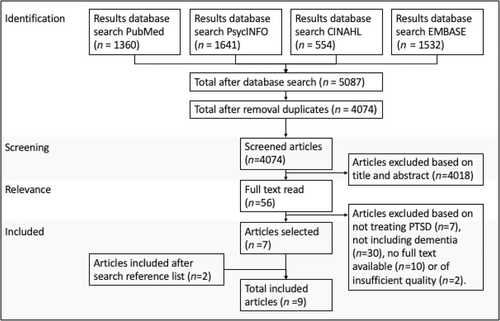
This review used a structured design. The literature search was conducted in PubMed, Embase, PsycINFO and CINAHL, according to the 'Preferred Reporting Items for Systematic Reviews and Meta-Analyses' (PRISMA) guidelines. The search strategy consisted of terms related to dementia and PTSD or trauma history. The complete search strategy is provided in Appendix A1.
Study selection
Publications until January 2022 were included in the search. Titles and abstracts were screened by two researchers and selected based on the following inclusion criteria1 inclusion of people with PTSD symptoms;2 inclusion of people with the diagnosis of dementia;3 the treatment form applied in the study must be adequately described;4 the effect of the treatment form applied must be reported;5 the study must have used one of the following designs: clinical trial, cohort study, cross-sectional study or case report.
The search was executed by two researchers in January 2022, including articles up to January 2022. When there was doubt about an inclusion, a third researcher was consulted, complete consensus was achieved. Studies were screened based on title and abstract, relevant full text studies were read and the reference list was screened to include possible missed studies.
Data extraction and quality assessment
Data were extracted by the first and second authors by using a standardised data collection table (Table 2).
The tool for evaluating the methodological quality of case reports and case series by Murad (2018) was used to assess the quality of the included case reports by the first author and checked by a second author.23 The paper's quality was then described as sufficient, dubious or insufficient, where sufficient papers score positive on more than 50% of the criteria, dubious scores positive on 50% of the criteria and insufficient scores positive on less than 50% of the criteria.
RESULTS
The results will be sectioned per treatment method. We will first describe the background of the treatment addressed in the articles. Second, the results described in the papers will be summarised, and their quality described. The systematic searches yielded a total of 5087 papers (4074 after the removal of duplicates). Of these articles, 4018 were excluded based on title and abstract. Then, 56 articles were selected for the screening of the full text. Seven out of these met the inclusion criteria. The screening of the reference lists resulted in the inclusion of two additional articles. This resulted in a total of nine articles (Fig. 1).
All included articles (n = 9) were case reports, in which a combined total of 11 cases were discussed. Of the nine case reports, four were of sufficient quality (Table 1). Eight case reports discussed one patient per paper, and one case report discussed three patients. All were without the use of control interventions. In three case reports, a combination of two treatment forms was used.24-26 Two cases were treated with EMDR,27, 28 and three cases with a modified form of EMDR, EMDR ‘on-the-spot’.24 In addition, four cases were treated with, each a different form of, pharmacological treatment,25, 29-31 one case received prolonged exposure therapy26 and one CBT.32 The way the diagnosis of PTSD was assessed, the form of dementia and comorbidities differed between cases. Table 2 shows the main study characteristics.
| Ahmed, 2018 | Amano, 2014 | Chopra, 2011 | Duax, 2013 | Hamilton, 1998 | Hargrave, 1993 | Jacobs, 2012 | Severson, 1997 | Van der Wielen, 2019 | ||
|---|---|---|---|---|---|---|---|---|---|---|
| Selection | 1. Represent(s) the whole experience of the investigator (centre/) or selection method unclear | N = 1 Method unclear | N = 3 Method unclear | N = 1 Method unclear | N = 1 Method unclear | N = 1 Method unclear | N = 1 Method unclear | N = 1 Method unclear | N = 1 Method unclear | N = 1 Method unclear |
| Ascertainment | 2. Was the exposure adequately ascertained? | Yes | Yes | Yes | Yes | Yes | Yes | Yes | Yes | Yes |
| 3. Was the outcome adequately ascertained? | Yes | No | Yes | Yes | No | No | Yes | No | Yes | |
| Causality | 4. Were other alternative causes that may explain the observation ruled out? | Not ruled out but mentioned | No | Not ruled out but mentioned | Not ruled out but mentioned | No | No | Not ruled out but mentioned | No | Not ruled out but mentioned |
| 5. Was there a challenge/rechallenge phenomenon? | Not applicable | Not applicable | No | Not applicable | No | No | Not applicable | No | Not applicable | |
| 6. Was there a dose–response effect? | Not applicable | Not applicable | No | Not applicable | No | No | Not applicable | No | Not applicable | |
| 7. Was follow-up long enough for outcomes to occur? | Yes, 9 months | Yes, 6 months | Yes, 9 months | Yes, 6 months | No, 2 months | No | No, 1 month | No, 3 weeks | Yes, 13 months | |
| Reporting | 8. Is the case(s) described with sufficient details | Yes | Yes | Yes | Yes | Yes | Yes | Yes | Yes | Yes |
| Overall score | Yes = 1 No = 0 | 4/6 Sufficient | 3/6 Dubious | 4/8 Dubious | 4/6 Sufficient | 2/8 Insufficient | 2/8 Insufficient | 4/6 Sufficient | 2/8 Insufficient | 4/6 Sufficient |
| Case report | Case | Form of dementia | PTSD diagnosis (trauma related to) | Comorbidities | Age/gender/ethnicity | Treatment form | Follow-up (months) | Measurement tool | Treatment effect |
|---|---|---|---|---|---|---|---|---|---|
| Ahmed, 2018 | 1 | Mild Parkinson dementia | History of traumatic events (sexual abuse, family death, burglary) | Depression, neuropathic pain and ‘extensive comorbidities’ | 83/F, Caucasian | 6 weekly EMDR | 9 | HADS and qualitative experience of participant (9 months after) | Subjective improvement of PTSD symptoms and resilience/ Increase of depression and fear |
| Amano et al, 2014 | 1 | Early-onset Alzheimer dementia now severe | PTSD like symptoms (abusive childhood) | None mentioned | 67/F Asian | EMDR on-the-spot | 6 | Data extracted from patient files from clinical observations | Chronic jeering and cursing decreased, smiled more, wandering remained but silently or singing songs |
| 2 | Moderate vascular dementia | PTSD like symptoms (WWII, burglary, fire) | Asthma, cerebrovascular disease, lower limb paralysis | 85/M Asian |
EMDR on-the-spot | 6 | Data extracted from patient files and from clinical observations | Decrease of restlessness, almost ceased moments of falling into a painful state of mind for hours, no re-experiencing of trauma. | |
| 3 | Severe Alzheimer dementia | PTSD like symptoms (WWII) | Diabetes, hypertension and hyperlipidaemia | 83/M Asian |
EMDR on-the-spot with Yokukansan granular extract (Chinese supplement) and two forms of sleeping medication | 6 | Data extracted from patient files and from clinical observations | Calmed down and smiled more, bilateral tapping gave a sense of security. | |
| Chopra et al 2011 | 1 | Mild to moderate dementia | PTSD (WWII) | Depression (citalopram 40 mg daily) | 85/M Caucasian | Memantine | 9 | MMSE, self-report and informant report consistently using a PTSD-CI tool (before initiation, after 12 weeks and after 9 months) | Self-reported improvement of PTSD symptoms. Nightmares and reliving trauma remained. Staff reported no significant change. Improved cognition |
| Duax et al, 2013 | 1 | Early Lewy body dementia /parkinsonism plus syndrome | PTSD (Vietnam war) | Depression (200 mg sertraline/10 mg donepezil), anxiety, somatic preoccupation and suspiciousness | 65/M Not mentioned | 14 sessions of prolonged exposure in 4 months | 6 | PCL-C, also BDI-II for depression | Improvement of PTSD symptoms. Reduction of depressive symptoms. Decline in cognition |
| Hamilton & Workman 1998 | 1. | Alzheimer dementia, moderate | Combat-related post-traumatic stress symptoms | Delirium due to urinary tract infection and dehydration, near blindness | 94/M Caucasian | Haloperidol 2 mg, trazodone 200 mg, lorazepam 0.5 mg | 2 | Not stated | Improvement of sleep and no night0time agitation |
| Hargrave et al, 1993 | 1. | Multi-infarct dementia | PTSD | Cerebrovascular accident | 70/M Caucasian | Trazodone 400 mg, buspirone 15 mg | 2 | Not stated | Decreased combativeness and repetitive yelling. Flashbacks and nightmares resolved. |
| Jacobs & Dinoff, 2012 | 1. | Moderate vascular dementia | PTSD symptoms (WWII) | Depression, anxiety, undifferentiated somatisation disorder | 90/M Caucasian | Therapy sessions, CBT/ACT, psychoeducation (memory book) | 1 | SLUMS, GDS, self and informant report | Improved SLUMS/GDS, better QoL reported, less anxious, fewer somatic symptoms. No effect of CBT. |
| Severson & McCartney, 1997 | 1. | Alzheimer's dementia | PTSD (recent sexual trauma) | Glaucoma, arthritis | 82/F Caucasian | Trazodone 25 g, sertraline 25 mg and later 50 mg | - | Not stated | Calmer, no more running down the hallway |
| van der Wielen et al, 2019 | 1 | Mild stage Alzheimer's dementia | Trauma history (family) | None mentioned | 69/F Caucasian | One session of EMDR | 13 | Multiple interviews, BDI-II and HADS-A (before treatment and 6 months after) | Decrease of guilt and flashbacks based on interviews. No difference on BDI-II and HADS-A |
- Abbreviations: ACT, acceptance and commitment therapy; BDI-II, Beck Depression Inventory - II; CBT, cognitive behavioural therapy; EMDR, eye movement desensitization and reprocessing; GDS, Geriatric Depression Scale; HADS-A, Hospital Anxiety and Depression Scale – Anxiety subscale; PCL-C, PTSD checklist - civilian; PTSD, post-traumatic stress disorder; SLUMS, Saint Louis University Mental Status Examination; QoL, Quality of life; WWII, World war two.
EMDR
EMDR is a protocolised psychological treatment method aimed at reducing the distress related to an experienced traumatic life event. It requires a person to recall the traumatic event and select the most distressing part of this event that is accompanied by dysfunctional thoughts and feelings. While visualising and discussing this moment, a distracting stimulus is applied. The participant must follow the therapist's finger movements from right to left. This uses the working memory and decreases the ability to feel the emotions connected to the traumatic event, giving the body the ability to connect a different emotional and physical meaning to the event – rescripting.33-35
Our literature search resulted in two case reports that described EMDR in two people with PTSD and dementia.27, 28 Van der Wielen (2019) described a woman of 69 with a mild stage of Alzheimer's dementia and trauma-related stress symptoms. She suffered from intrusive trauma-related memories about her mother's institutionalised palliative care phase paired with emotional outbursts and feelings of guilt. She received one session of EMDR-conforming standard care with the presence of her husband during the therapy session. The authors concluded that EMDR according to the protocol is applicable for people with mild Alzheimer's dementia (Table 2). The quality of this paper is sufficient with a relatively long follow-up of 13 months (Table 1).
Ahmed (2018) described a case of a Caucasian woman 83 years old with mild Parkinson's dementia who had experienced multiple traumatic life events. She had a history of depression and neuropathic pain. She underwent six weekly EMDR sessions according to standard protocol. She reported fewer complaints of tension related to the traumatic memory, less avoidance and felt more resilient. Her depression and fear increased, which she reported being a consequence of her decline due to parkinsonism. The authors concluded that EMDR is a realistic treatment option for the treatment of people with dementia who suffer from traumatic memories but requires more research (Table 2). The quality of this case report is sufficient with a follow-up of 9 months and an adequate description of the intervention (Table 1).
EMDR ‘on-the-spot’
EMDR ‘on-the-spot’ is a version of EMDR where, when the person shows the mentioned symptoms, therapy is executed by bilateral tapping on shoulders or knees and using simple words while they are reliving the traumatic experience (whereas in EMDR, a person is asked to actively think of this experience).24 Amano (2014) described three cases in a case series, involving three Asian nursing home residents. All three cases experienced challenging behaviour often associated with neuropsychiatric symptoms of dementia, such as physical aggression, screaming, restlessness, agitation, wandering and sleeping disorders. Due to trauma in the past, they were thought to have PTSD, but a formal diagnosis was not made. In these cases, a personalised and more simplified form of EMDR, which they named EMDR ‘on-the-spot’, was used as people included could not follow the therapist's instructions due to the severity of the dementia. The EMDR ‘on-the-spot’ sessions were held four to six times. All three cases showed a significant improvement in symptoms (less anger, less reliving of the trauma, more smiling) in the caregiver reports (Table 2). The quality of this paper is dubious as the outcome was evaluated using only patient files and clinical observation (Table 1).
Prolonged exposure
Prolonged exposure is a form of trauma-focused CBT.36 It combines exposure in thoughts and in practice in such a way that the traumatic memory can be processed. The focus is on repetitive and long reliving in which avoidance is brought to a minimum.37, 38 Prolonged exposure requires 8–15 sessions, each of 60–90 min; it is a validated form of psychotherapy for PTSD.36
One article was found that used prolonged exposure for the treatment of PTSD in a person with dementia26 (n = 1). Duax et al. described a 65-year-old male veteran with PTSD and early-stage Lewy body dementia. He had symptoms of agitation, apathy, sleeping disorders, nightmares and cognitive problems. PTSD was diagnosed following clinical interviews and a detailed history with his wife. The standard protocol for prolonged exposure was adjusted to better fit the needs of the patient; some sessions lasted longer, sessions were recorded for re-watching by the patient, and the partner was present to guide the patient in the first five sessions. After the 14 sessions of prolonged exposure, additional therapy sessions were held every 2 weeks for 6 months to monitor progress and/or decline. The content of these sessions was diverse, among others, behavioural activation and exposure, risk assessment and monitoring, discussions of caregiver burden. After the treatment, the Clinician-Administered PTSD Scale for Diagnostic and Statistical Manual of Mental Disorders 4th edition showed a positive effect of treatment on PTSD symptoms as did the self-reports. The positive effect was still present 6 months after treatment (Table 2). This case report is of sufficient quality with good ascertainment of the treatment outcomes (Table 1).
Multiple psychological interventions
We found one case report that used multiple forms of interventions not included in the other case reports.32 They combined CBT, acceptance and commitment therapy (ACT), psychoeducation and the formation of a memory book.
CBT is based on the theory that a person's problems are maintained by potentially modifiable cognitions and behaviour. It is a form of psychotherapy that teaches to think differently about a stressful event in such a way that it does not raise intense emotions.39 In contrast, in ACT, the goal is not to analyze and change your cognitions, but rather to accept them for what they are and instead to focus on personal values and goals. The goal is that as a consequence, internal experiences will have less influence on emotion and behaviour.40 Jacobs and Dinoff discussed the case of a 90-year-old Caucasian man, with significant vascular dementia, somatoform disorder and PTSD symptoms after WWII trauma. The patient experienced a fear of dying, gastrointestinal symptoms, feelings of depression, lack of energy and agitation. He was also aggressive. The patient received multiple therapy sessions divided into three phases using multiple forms of therapy: CBT, ACT and psychoeducation combined with a memory book.
In the study by Jacobs and Dinoff, phase I consisted of a geropsychological evaluation with a behavioural analysis and therapy sessions. In the therapy sessions, both the patient and his wife were involved for 6 months and specific issues, such as the fear of abandonment by his wife, were addressed. Following this, primary improvements in mood, agitation and anxiety were seen. Phase II consisted of CBT and ACT. The CBT was adjusted to accommodate vascular dementia. Sessions were slower than usual, visual aids were used, and information was repeated more often. Regardless, it did not appear possible for him to challenge his own thoughts sufficiently for the CBT to have an effect. Therefore, ACT started, and it was possible for the patient to experience creative hopelessness and he felt grief for his situation. He no longer wanted to go home and accepted living in the nursing home, but the distress and fear of dying remained. Phase III consisted of psychoeducation and ‘treatment’ of the dementia in the form of a memory book. The memory book and psychoeducation helped the participant when he was agitated, resulting in a decrease in lorazepam use32 (Table 2). The paper by Jacobs and Dinoff is of sufficient quality with a short follow-up term but a detailed case description (Table 1).
Pharmacological treatment
The symptoms of PTSD can also be targeted with pharmacological treatment. Clinical practice shows that people with PTSD and dementia are often administered anti-psychotics.41 PTSD is not a registered indication for treatment with anti-psychotics, and often anti-psychotics have a high risk of adverse events and side effects, requiring caution in their administration for off-label use.42 Specific serotonergic agents have been proven to be effective in the treatment of PTSD, but not superior to trauma-focused-psychotherapy forms.21, 43
We found four case studies in which pharmacological treatment was given to people with PTSD and dementia25, 29-31 (n = 4). Chopra (2011) described an 85-year-old Caucasian man with PTSD and mild to moderate dementia. He had PTSD as a consequence of WWII trauma. At the onset of the study, he had been receiving treatment with citalopram 40 mg once daily over the past 2 years, which was continued during the course of the study. The patient suffered from sleeping disorders and nightmares and first prazosin 1 mg was started, which was increased to 3 mg over the course of 5 weeks with no effect. Due to side effects, orthostatic hypotension causing falls, the prazosin was stopped. Consequently, memantine was titrated to 10 mg twice daily without side effects (Table 2). This paper is of dubious quality with no challenge-rechallenge phenomenon, but a relatively good measurement of outcomes using a structured but not validated measuring tool (Table 1).
Hamilton, Workman Jr., Hargrave and colleagues and Severson and McCartney performed studies dating further back.25, 30, 31 One of the case reports describes a Caucasian man of 94 years old with moderate Alzheimer's dementia and combat-related post-traumatic stress symptoms. The patient was treated with trazodone combined with haloperidol and lorazepam. A good effect of the combination therapy with an improvement of sleep and no more night-time agitation was described.31
The case report of Hargrave (1993) describes a Caucasian man of 70 years old with multi-infarct dementia and PTSD without trauma description. He was treated with trazodone and buspirone. It shows a positive effect of the treatment with decreased combativeness, decreased yelling and resolved flashbacks and nightmares.30
The case report of Severson and McCartney describes a Caucasian woman of 82 years old with Alzheimer's dementia who suffered from PTSD after sexual trauma. She was treated with trazodone and sertraline. The person became calmer and showed less rushing through the hallways25 (Table 2). These papers are all of insufficient quality due to the short description of treatment outcomes without the use of measuring tools (Table 1).
DISCUSSION
This review shows that studies of the treatment of PTSD in people with dementia are rare and only identified a few studies in the form of case reports. The quality of the nine case reports varies. There were three case reports, all discussing pharmacological intervention, of insufficient quality,25, 30, 31 two dubious studies discussing EMDR ‘on-the-spot’24 and memantine29 and four case reports of sufficient quality,26-28, 32 of which two described EMDR,27, 28 one applying prolonged exposure26 and a fourth describing a combination of therapies.32
The quality of case reports describing EMDR were sufficient; a clear case description was given (Table 1).24, 27, 28 EMDR is an approved intervention for PTSD and is described in practice guidelines.33-35 All three studies that describe EMDR in people with dementia, describe it as a feasible intervention. The case reports show positive effects on the symptoms measured or described, such as fewer flashbacks, more acceptance of the past and less restlessness.24, 27, 28 Positive effects of EMDR on neuropsychiatric symptoms often associated with challenging behaviour of dementia can reflect the alternative clinical presentation of PTSD in people with dementia, showing symptoms such as screaming.16 These case reports indicate that EMDR might be also feasible and effective for reducing PTSD symptoms in people with dementia. In the case report of Amano et al. the intervention was combined with pharmacological intervention.24 As a consequence, the effect of the EMDR alone cannot be established, but these results are transferable to common practice, where patients often also receive pharmacological treatment.
Four papers discuss pharmacological treatment, but the quality of these papers is dubious29 or insufficient.25, 30, 31 Chopra (2011) showed a careful positive effect of memantine in addition to citalopram on PTSD symptoms and cognitive decline in people with mild–moderate dementia, but a challenge-rechallenge and dose–response effect is not ascertained. Further studies on pharmacological interventions for PTSD, such as an open label trial by Ramaswamy, also showed a positive effect of memantine in 26 veterans with PTSD and mild cognitive disorders, but this study excluded people with dementia.44 Future research could be beneficial to explore the effects of memantine in people with PTSD and dementia. The other three included case reports all administered trazodone in combination with another form of medication, such as haloperidol with lorazepam, buspirone or sertraline. They reported positive effects with improved sleep, yelling less, being calmer and smiling more.25, 30, 31 The paper of Bruneau described treatment with antipsychotic medication in two cases of PTSD with dementia. In one case, it was ceased due to side effects and in a second case it was effective, but the specific type of antipsychotic is not mentioned.45 The quality of found literature provides insufficient reliable evidence for the pharmacological treatment of PTSD in people with dementia.
Prolonged exposure is described in one case report with positive effects on PTSD symptoms, even after 6 months. The quality of the paper is sufficient, but due to the combination of pharmacological treatment, the positive results cannot be directly linked to prolonged exposure. Prolonged exposure is a well-researched form of therapy proven successful in the treatment of PTSD.46 The current case report shows us that prolonged exposure can also be applied in people with dementia. Nonetheless, there is insufficient evidence of the positive effect of prolonged exposure in people with dementia.
Jacobs and Dinoff describe an elaborate combination of therapy forms: CBT, ACT and psychoeducation combined with a memory book.32 CBT is an approved form of PTSD treatment in people without dementia.47 The case described showed the complexity of CBT, due to the combination of PTSD with dementia and this part of the treatment was unsuccessful. ACT managed to give the patient insight into his limitations and the effects of the memory book were not described. This case report of sufficient quality describes expected challenges in the use of CBT in people with dementia; there is too little evidence to exclude CBT in this population altogether.
Overall, the studies included patients with different forms of dementia with varying severity. We found no description regarding the objective assessment of severity of dementia. The severity of dementia plays an important part in clinical practice as certain neuropsychiatric symptoms are more prevalent in certain stages of dementia.48 Five cases describe Alzheimer's dementia, three describe vascular dementia, two describe a form of Lewy body or Parkinson's dementia and in one case the aetiology is not mentioned. There is no literature describing the influence of different forms of dementia on trauma processing and/or PTSD. PTSD increases the risk of dementia in general, but so far, studies have not found PTSD to accelerate certain aetiologies of dementia.49 Four females and seven males are included in the case reports. Six men had combat and/or war-related traumas; in one of the cases, the cause of trauma was not mentioned. Two of the women experienced sexual trauma and two experienced violence during their childhood. Women have a higher risk of developing PTSD due to gender roles, predisposition and hormonal influences.50
Besides the variation in the diagnosis of dementia, in five case reports, a clear diagnostic description and/or tool for diagnosing PTSD in people with dementia is missing. In multiple cases, there was no formal diagnosis of PTSD but the descriptive diagnosis of ‘PTSD symptoms’24, 31, 32 or ‘history of traumatic events’.27, 28 Of the included studies, Ahmed (2018), Jacobs and Dinoff (2012), and van der Wielen (2019), did not use tools for the specific evaluation of PTSD symptoms but tools aimed at fear, depression and/or cognition to measure treatment outcome. Amano extracted data from patient files and clinical observations which are not further specified. Chopra and Duax used a structured tool, the PTSD – cognitive impaired tool, which is a structured but not yet a validated tool. The PTSD checklist – civilian is used by Duax.
This study contributes to the existing knowledge and marks the need for further research, but there are limitations. The scientific evidence of this review is limited due to the absence of any controlled and/or randomised studies. Four of the included case reports have a sufficient level of quality, but the sole inclusion of case reports may lead to publication bias with mainly positive results. Selection bias is increased as the method of inclusion is not clear in any of the case reports. In addition, although the results are assessed with objective questionnaires, only afew are specifically aimed at measuring PTSD symptoms. Thus, an objective comparison of the effects between the case reports is not feasible. In five of the nine case reports the formal diagnosis of PTSD has been formed.25, 26, 29, 30, 32 Relevant comorbidities are described in all but two case reports.24, 25
CONCLUSION
The case reports in this structured literature review show us PTSD treatment in people with dementia can be effective in reducing symptoms possibly related to PTSD. EMDR, prolonged exposure, ACT and pharmacological interventions are feasible interventions in this population, even in cases of severe dementia. The case reports show the most hopeful results of EMDR. The clinical implications of the included studies are limited due the demographic variables such as type of dementia and severity, absence of validated diagnostic tools for PTSD and validated PTSD symptom evaluation tools, making the quality baseline comparison for treatment effects limited.
The treatment of PTSD in people with dementia starts with recognising PTSD in this population. To recognise PTSD it is important to differentiate PTSD from symptoms often associated with neuropsychiatric symptoms of dementia; for this, a structured diagnostic tool of PTSD for people with dementia could be beneficial.51 Besides this, more research is required to study the effectiveness of different treatment interventions in this population using a standardised measuring tool for PTSD symptoms. Based on this review, randomised controlled trials to analyze the effect of EMDR in people with dementia and PTSD are most hopeful, but so far, evidence is limited due to the low number of studies in this population.
Funding Information
This research received no specific grant from any funding agency in the public, commercial, or not-for-profit sectors.
Conflict of interest
The authors have no potential conflicts of interest to disclose.
Open Research
DATA AVAILABILITY STATEMENT
Data sharing is not applicable to this article as no new data were created or analyzed in this study.