Postpartum specific anxiety in a French population: Validation of the French version of the Postpartum Specific Anxiety Scale [PSAS-FR]
Abstract
Purpose
This study aims to validate the Postpartum-Specific-Anxiety-Scale (PSAS) as a French-language instrument, which assesses maternal and infant-related anxieties during the postpartum period.
Design and Methods
The methodology included six stages: preliminary French translation; selection of most articulate items and back-translation; rectification of discrepancies; pilot study (n = 257); reliability and validity studies (n = 258; n = 874); and test–retest reliability study (n = 231).
Findings
The PSAS-FR demonstrated good acceptability, high internal consistency of the global scale (Cronbach's α = 0.93), and each of the factors; along with good validity, and test–retest reliability. The receiver operating characteristic analysis suggested a satisfactory screening tool.
Practice Implications
The PSAS-FR appears to be a valid and reliable tool to screen for postpartum anxieties in the French-speaking population.
1 INTRODUCTION
Perinatal anxiety represents an underestimated health issue in France which affects between 10% and 20% of women,1 either during pregnancy or the postpartum. Recent studies suggest postpartum anxiety may occur more frequently than depressive disorders,2 with between 2% and 4% of cases being comorbid.3 Despite its high prevalence rate, only 15% of women receive treatment.4
The postpartum is a complex transition period involving life-changing adjustments which can affect women's psychological health and increase anxiety symptoms.5 Mothers often experience concerns about the health and the well-being of the infant,6 and about their new maternal role or parenting skills.3 These anxieties may be considered as non-pathological evolutionary manifestations which aim to increase vigilance in the mother and protect the infant.7 However, anxiety becomes problematic when it consumes a significant proportion of a woman's time, prevents her from fulfilling her parenting role, and/or interferes with self-care.8 Motherhood can also exacerbate pre-existing psychological vulnerabilities and lead to a deterioration of maternal mental health, including high levels of anxiety and other comorbid symptoms.7
Although research has mainly focused on postpartum depression, the study of perinatal anxiety has increased recently due to its high prevalence and potentially harmful consequences on maternal and infant health.6 Recent studies suggest anxious-depressive symptoms are likely to generate difficulties in the parental role and disruptions of the early mother–infant bond.9 Links between maternal postpartum anxiety and infant cognitive, social, emotional, somatic, and motor developmental impairment have also been reported.10
To date, most researchers and health professionals use general anxiety assessment tools which are not specific to the perinatal period, such as the Spielberger State-Trait Anxiety Inventory (STAI-Y), or which focus on screening for postpartum depression, such as the Edinburgh Postnatal Depression Scale (EPDS), to assess postnatal maternal anxiety.6 Indeed, given the frequent comorbidity between anxiety and depression, postpartum-specific scales such as the EPDS have been used to screen for both depression and anxiety. Although in several studies three items from the EPDS have been retained in an anxiety factor among samples of postpartum women, researchers contend that the scale does not measure anxiety as in independent clinical entity.6 General anxiety assessment tools also may artificially inflate anxiety scores and the probability of false positives, due to the inadequacy of items to the specific characteristics of pregnancy and postpartum, particularly regarding somatic symptoms.11 Furthermore, a significant number of women who experience high levels of suffering and concerns linked to motherhood yet do not meet general anxiety criteria.6
To address this issue, the Postpartum Specific Anxiety Scale (PSAS6) was developed and validated to target a spectrum of manifestations of maternal postpartum anxieties. This scale has demonstrated excellent psychometric properties as well as a better predictive efficacy on infant-feeding outcomes12 and maternal bonding,13 compared with general anxiety and depression measures. More recently, a Turkish version has been developed, demonstrating good initial validity and reliability.14
1.1 Research aims
The purpose of this study is to validate the French version of the Postpartum Specific Anxiety Scale (PSAS-FR). A series of psychometric analyses were performed to assess factor structure, convergent validity, internal and test–retest reliability, sensitivity, and specificity.
2 MATERIAL AND METHODS
2.1 Participants
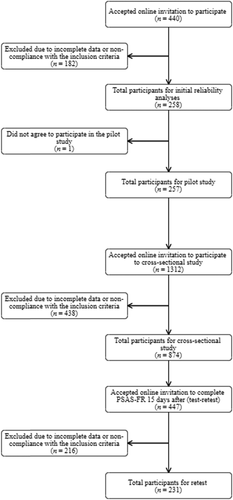
Participants were French-speaking women living in France (first study 90%; second study 89%), Europe (first study 7%; second study 6%), and other continents (first study 4%; second study 5%), who were mothers of infants aged between birth and 6 months. Women were primiparous or multiparous, aged between 18 and 45 years, and gave fully informed consent to participate. The exclusion criteria were poor language fluency in French, refusal to participate, and being aged less than 18 or more than 45 years. Among the 440 women who participated in the first study and the 1312 participants in the second study, 160 (36%) and 438 (33%), respectively, were excluded due to non-compliance with the inclusion criteria or missing data on the questionnaires (Figure 1).
2.2 MEASURES
2.2.1 Demographics
A 25-item questionnaire collected socio-demographics; health information about the mother, including maternal age, obstetric history, course and complications of pregnancy and delivery, antenatal and current psychological care, current diagnosis of anxiety or depression and use of psychotropic medication; country of residence; professional and marital status; and educational attainment. Infant characteristics (age; gender; weight and size at birth; birth order; and mode of feeding) were also gathered.
2.2.2 Postpartum Specific Anxiety Scale
The PSAS6 is a 51-item self-report instrument, developed and validated in a sample of English-speaking women residing in the UK, which measures the frequency of maternal and infant-related anxieties specific to the first 6 months postpartum, experienced during the previous 7 days. Its structure comprises four factors: “Maternal Competence and Attachment Anxieties”; “Infant Safety and Welfare Anxieties”; “Practical Infant Care Anxieties”; and “Psychosocial Adjustment to Motherhood.”6 Items are scored on a 4-point Likert scale with a maximum score of 204. A threshold score of 112 was suggested as detecting clinically significant levels of anxiety. Psychometric analyses demonstrated excellent validity and high internal consistency (Cronbach's α = 0.95).
Before conducting the present study, authorization to translate was obtained from the PSAS Working Group, who also provided the translation procedure,15 which followed six stages: (1) preliminary translation into French by two independent translators. (2) A third member, who is a professional English-speaking translator, selected the most articulate items of the two translations and back-translated the scale blindly. (3) The scale was then checked by the PSAS Working Group and discrepancies were rectified. (4) A pilot study (n = 257) was then conducted to assess the scale acceptability through two questions which evaluated comprehensibility and ease of responding on a 10-point Likert scale (ranging from “Not at all easy to understand” [0] to “Extremely easy to understand” [10], for the first question; and “Not at all easy to complete” [0] to “Extremely easy to complete” [10], for the second), following the same guidelines of the English original validation study.6 Further information regarding the acceptability of the PSAS-FR was also collected through an optional text box at the end of the questionnaire which allowed participants to describe their experience during the scale completion. (5) Initial reliability analyses (first study, n = 258) and a second cross-sectional study (n = 874) were conducted to assess the psychometric properties of the scale. (6) Finally, a subsample (n = 231) was re-contacted 15 days after the first assessment to evaluate test–retest reliability.
2.2.3 Spielberger State-Trait Anxiety Inventory
The STAI-Y is a 40-item self-report instrument that evaluates general anxiety. It comprises two 20-item subscales which assess situational (state) and stable (trait) disposition to anxiety. Responses are scored on a 4-point Likert scale. The validated French version16 was used, having previously demonstrated good reliability and validity.
2.2.4 Edinburgh Postnatal Depression Scale
The EPDS is a 10-item self-report instrument to assess depressive symptomatology during the postpartum period. Items are scored on a 4-point Likert scale and scores range from 0 to 30. The validated French version17 was used, having previously demonstrated good validity and reliability, with a suggested cut-off score of 10.5 when screening for perinatal depression.
2.3 Procedure
Online recruitment was conducted via parenting associations (Maman Blues, CIANE), and social media platforms. A link to the Framaform software allowed participants to access the online survey. Participants were informed of the purposes and procedures of the study through an information sheet on the first page. Fully informed consent was collected by a mandatory question which had to be checked before gaining access to the questionnaires. Participation was voluntary, and mothers were free to withdraw from the research at any time without justification. To assess test–retest reliability, a sub-sample of women (n = 447) who had given their consent were re-contacted by e-mail to complete the PSAS-FR questionnaire again 15 days after the first assessment. Any situation of distress identified and any request for support was redirected to the principal investigator [JW] to offer an interview or therapeutic referral. For this purpose, participants' e-mail addresses and telephone numbers were requested at the end of the survey. Data were handled anonymously, and no link was made between participants' data and their contact details. Responses were associated with a code used when computing the data.
2.4 Statistical analyses
Descriptive and inferential statistical analyses were performed by using SPSS Statistics for Windows, version 1.0.0.1327.18 Kolmogorov–Smirnov and Lilliefors and normality tests by Shapiro–Wilk were performed to verify the normality of the data distribution. Since the PSAS, STAI-Y, and EPDS data followed a non-normal distribution and non-parametric statistical tests were used. To assess the psychometric properties of the PSAS-FR, exploratory factor analysis was conducted using Varimax rotation. Reliability and internal consistency were estimated using Cronbach's alpha coefficients. Convergent validity and test–retest reliability were assessed through Spearman rank correlation coefficients. A receiver operating characteristic (ROC) analysis was performed to evaluate the screening accuracy of the translated instrument, allowing to identify an optimal cut-off score for anxiety screening using the Youden index (= Sensitivity + Specificity − 1).
2.5 Ethics
The ethical approvals for this study were obtained from the Research Ethics Committee CER UP No. 2019-90. All procedures of the study were performed in accordance with the 1964 Helsinki Declaration and its later amendments or comparable ethical standards.
3 RESULTS
3.1 Sample characteristics
Women and infant mean age (n = 874) ranged from 18 to 44 years (M = 30.47; SD = 4.30) and 2 days to 27 weeks (M = 13.94; SD = 6.87), respectively. The sample was mainly composed of French (89%), partnered (98%) women, who had tertiary-level educations (77%), and were pursuing careers (86%). Regarding obstetric and health information, women were mainly primiparous (59%), with few having had multiple pregnancies (2%) or difficulty conceiving (19%). Some women encountered complications during pregnancy (28%) and during childbirth (32%). One hundred and eighteen women received psychological/psychiatric care during pregnancy (14%), but fewer were under psychological/psychiatric care at the time of taking the survey (7%), with a small percentage of those using psychotropic medication (3%). Sixty-three participants declared having a current diagnosis of anxiety or depression disorder (7%) by a health professional (Table 1 and Table 2).
| Maternal characteristic | Value | Maternal characteristic | Value |
|---|---|---|---|
| Age (years) | Difficulties in becoming pregnant (n/%) | ||
| Min–Max | 18–44 | Yes | 163 (18.6) |
| Mean (SD) | 30.47 (4.30) | No | 711 (81.4) |
| Country of residence (n/%) | Complications in pregnancy (n/%) | ||
| France | 777 (88.9) | Yes | 246 (28.1) |
| Other European | 53 (6.1) | No | 628 (71.9) |
| Other non-European | 44 (5.0) | Complications in childbirth (n/%) | |
| Marital status (n/%) | Yes | 279 (31.9) | |
| Married/PACS | 855 (97.8) | No | 595 (68.1) |
| Single | 15 (1.7) | Mode of delivery (n/%) | |
| Separated/divorced/widowed | 4 (0.5) | Spontaneous vaginal delivery | 538 (61.6) |
| Socio-professional category (n/%) | Triggered vaginal delivery | 168 (19.2) | |
| Farmer | 8 (0.9) | Planned cesarean | 59 (6.8) |
| Artisan, shopkeeper, and head of company | 46 (5.3) | Emergency cesarean | 109 (12.5) |
| Managerial and professional occupation | 222 (25.4) | Psychological care during pregnancy (n/%) | |
| Technician and associate professional | 103 (11.8) | Yes | 118 (13.5) |
| Employee | 361 (41.3) | No | 756 (86.5) |
| Manual laborer | 9 (1.0) | Current psychological/psychiatric care (n/%) | |
| Student | 15 (1.7) | Yes | 64 (7.3) |
| No professional activity | 110 (12.6) | No | 810 (92.7) |
| Educational attainment (n/%) | Current prescribed medication for anxiety/depression (n/%) | ||
| Master's and doctoral degree | 280 (32.0) | Yes | 25 (2.9) |
| Bachelor's degree | 395 (45.2) | No | 849 (97.1) |
| A-level or equivalent | 117 (13.4) | Current diagnosis of anxiety/depression (n/%) | |
| High school without diploma | 16 (1.8) | Yes | 63 (7.2) |
| BTEC First Diploma or equivalent | 45 (5.1) | No | 811 (92.8) |
| Secondary school education | 16 (1.8) | ||
| No qualifications | 5 (0.6) | Difficulties in mother–child interactions (n/%) | |
| Primiparous (n/%) | Yes | 117 (13.4) | |
| Yes | 512 (58.6) | No | 757 (86.6) |
| No | 362 (41.4) | Difficulties in infant care practices (n/%) | |
| Miscarriage (n/%) | Giving the bath | 33 (3.8) | |
| Yes | 231 (26.4) | Breastfeeding | 116 (13.3) |
| No | 643 (73.6) | Bottle feeding | 36 (4.1) |
| Abortion (n/%) | Starting baby's dietary diversification | 2 (0.2) | |
| Yes | 142 (16.2) | Changing the nappy | 5 (0.6) |
| No | 732 (83.8) | Helping the baby fall asleep | 248 (28.4) |
| Medical abortion/fetal death in utero (n/%) | Helping the baby sleep through the night | 3 (0.3) | |
| Yes | 33 (3.8) | Soothing the baby | 170 (19.5) |
| No | 643 (73.6) | Understanding baby's behavior/needs | 204 (23.3) |
| Planned pregnancy (n/%) | Creating emotional bond with the baby | 4 (0.5) | |
| Yes | 716 (81.9) | Responding to baby's proximity need | 3 (0.3) |
| No | 158 (18.1) | Leaving the baby with familiar adults/at a childcare setting | 4 (0.5) |
- Note: n = 874.
| Infant characteristic | Value | Infant characteristic | Value |
|---|---|---|---|
| Age (weeks) | Birth order (n/%) | ||
| Min–Max | 0–27 | First | 515 (58.6) |
| Mean (SD) | 13.94 (6.87) | Second | 244 (27.9) |
| Gender (n/%) | Third | 92 (10.5) | |
| Female | 468 (53.5) | Fourth | 14 (1.6) |
| Male | 406 (46.5) | Fifth and more | 12 (1.4) |
| Height at birth (cm) | Timing of birth (n/%) | ||
| Min–Max | 30–62 | Premature (<37 weeks) | 59 (6.8) |
| Mean (SD) | 49.56 (2.64) | Early term (>37 <39) | 357 (40.8) |
| Weight at birth (g) | Full term (>39 <41) | 343 (39.2) | |
| Min–Max | 1200–4840 | Late term (>41 >42) | 113 (12.9) |
| Mean (SD) | 3311.31 (505.35) | Postterm (>42 weeks) | 2 (0.2) |
| Multiple birth (n/%) | Mode of feeding (n/%) | ||
| Yes | 17 (1.9) | Exclusively breastfeeding | 532 (60.9) |
| No | 857 (98.1) | Exclusively formula feeding | 207 (23.7) |
- Note: n = 874.
The sample characteristics were compared with data from the last national perinatal inquiry carried out in France.19 The sample (n = 874) does not differ substantially regarding the distribution of maternal age (national data: M = 30.3; SD = 5.2) and the type of pregnancy (national data: 98.2% had a single pregnancy and 1.8% had multiple pregnancies). Participants in this study were more likely to be primiparous, married or partnered, and had higher educational attainment and socio-economic status than those from the general population (national data: 42.2% primiparous; 81.9% married or partnered; 55.4% had tertiary-level education; and 16.8% unemployed). However, women in this study received more professional help due to psychological difficulties during pregnancy than those in the national inquiry (national data: 6.4%). This would, however, be consistent with the fact that this sample had a higher level of state anxiety (28%; based on the STAI-Y cut-off score) and depression (38%; based on the EPDS cut-off score) (Table 3).
| PSAS-FR | STAI Y– A (State) | STAI Y– B (Trait) | EPDS | ||
|---|---|---|---|---|---|
| n = 258 | Mean (SD) | 98.12 (22.45) | 42.05 (12.87) | 43.71 (11.08) | 10.02 (5.24) |
| Min–Max | 49–154 | 20–73 | 21–75 | 1–27 | |
| n = 874 | Mean (SD) | 95.85 (22.76) | 37.38 (13.36) | – | 9.27 (5.84) |
| Min–Max | 47–164 | 20–79 | – | 0–29 |
- Note: First study n = 258. Second study n = 874.
- Abbreviations: EPDS, Edinburgh Postnatal Depression Scale; PSAS-FR, Postpartum Specific Anxiety Scale-French language; STAI-Y, Spielberger State-Trait Anxiety Inventory.
3.2 Pilot study
The pilot study (n = 257) revealed a good face validity of the PSAS-FR. The mean score for the item evaluating comprehensibility was 8.34 (±1.79), and 8.63 (±1.74) for ease of responding. Thirty-nine women provided qualitative responses, which were predominantly positive, testifying to the acceptability of the PSAS-FR. Negative comments mainly concerned the difficulty to understand some items which were removed after the first-factor analysis, as well as the fact of not being concerned by Item 35 (“I have worried about leaving my baby in a childcare setting”). The response to this item was then deemed to be optional.
3.3 Factor structure
The factor structure of the PSAS-FR was determined through exploratory factor analysis. The choice of factors was based on the Kaiser criterion (Eigenvalues > 1), the scree plot elbow point and the cumulative variance explained. Four factors were initially retained, however, this analysis revealed that items 2, 7, 19, 26, 30, 42, and 43 had low communalities and factor loadings below the 0.3 threshold after Varimax rotation. These items were therefore removed resulting in a 44-item French-language Postpartum Specific Anxiety Scale (PSAS-FR).
The factor analysis was reconducted and suggested a 4-factor structure (Table 4). Although according to Kaiser's criterion 5 factors were obtained, the last factor had a low Eigenvalue and variance explained. Finally, 4 factors were retained which explain 38.61% of the variance of the model. Additional factor analyses were performed afterward considering 3, 2, and 1 factors and corroborated the 4-factor structure. The PSAS-FR showed low-to-moderate inter-item correlations, ranging from 0.01 to 0.70. Although items 10, 21, 22, 27, 46, and 48 had communalities below the 0.2 threshold, the factor loadings were above 0.3, and they were therefore retained.
| Factor | Eigenvalue | % Total variance | % Cumulative variance |
|---|---|---|---|
| 1 | 10.92 | 24.81 | 24.81 |
| 2 | 2.75 | 6.26 | 31.07 |
| 3 | 1.74 | 3.97 | 35.04 |
| 4 | 1.57 | 3.57 | 38.61 |
| 5 | 1.01 | 2.31 | 40.92 |
- Note: n = 258. Retained factors in bold.
Varimax rotation revealed the first factor (“Maternal Competence and Attachment Anxieties”) included 10 items (items 4, 9, 17, 18, 20, 23, 24, 36, 38, and 40), which explained 24.81% of the variance of the model (Cronbach's α = 0.88). The second factor (“Infant Safety and Welfare Anxieties”) comprised 12 items (items 3, 8, 11, 15, 16, 22, 33, 35, 44, 47, 50, and 51), and explained 6.26% of the variance (Cronbach's α = 0.85). The third factor (“Practical Infant Care Anxieties”) explained 3.97% of the variance (Cronbach's α = 0.77) and included seven items (items 13, 14, 28, 29, 31, 34, and 49). Finally, the fourth factor (“Psychosocial Adjustment to Motherhood”), explained 3.57% of the variance (Cronbach's α = 0.83) and included 15 items (items 1, 5, 6, 10, 12, 21, 25, 27, 32, 37, 39, 41, 45, 46, and 48) (Table 5).
| Factor loadings | |||||
|---|---|---|---|---|---|
| Item | Original item/French translation | 1 | 2 | 3 | 4 |
| 1 | I have felt unable to juggle motherhood with my other responsibilities./Je me suis sentie incapable de concilier mon rôle de mère avec d'autres responsabilités. | 0.35 | −0.10 | 0.12 | 0.35 |
| 3 | I have worried about accidentally harming my baby./J'ai craint de blesser accidentellement mon bébé. | 0.40 | 0.45 | 0.17 | 0.03 |
| 4 | I have worried about how I will cope with my baby when others are not around to support me./Je me suis inquiétée de la façon dont je me débrouillerai avec mon bébé lorsque d'autres personnes ne seront pas là pour me soutenir. | 0.57 | 0.12 | 0.09 | 0.19 |
| 5 | I have felt that I do not get enough support./J'ai eu l'impression de ne pas recevoir assez de soutien. | 0.20 | 0.12 | 0.14 | 0.55 |
| 6 | I have been less able to concentrate on simple tasks than before my baby was born./J'ai eu plus de difficultés à me concentrer sur des tâches simples qu'avant la naissance de mon bébé. | 0.31 | 0.08 | 0.21 | 0.39 |
| 8 | I have felt frightened when my baby is not with me./J'ai eu peur quand mon bébé n'était pas avec moi. | 0.04 | 0.68 | 0.08 | 0.10 |
| 9 | I have worried I will not know what to do when my baby cries./Je me suis inquiétée de ne pas savoir quoi faire quand mon bébé pleure. | 0.72 | 0.08 | 0.29 | −0.26 |
| 10* | I have worried more about my relationship with my partner than before my baby was born./Je me suis davantage inquiétée de ma relation avec mon partenaire qu'avant la naissance de mon bébé. | 0.14 | 0.13 | 0.13 | 0.36 |
| 11 | I have worried that my baby feels more content in someone else's care./J'ai craint que mon bébé se sente plus heureux auprès de quelqu'un d'autre. | 0.29 | 0.37 | −0.04 | 0.30 |
| 12 | I have felt isolated from my family and friends./Je me suis sentie isolée de ma famille et de mes amis. | 0.15 | 0.06 | 0.08 | 0.54 |
| 13 | I have worried about my baby's weight./Je me suis inquiétée du poids de mon bébé. | 0.05 | 0.31 | 0.63 | 0.16 |
| 14 | I have worried about getting my baby into a routine./Je me suis inquiétée d'arriver à instaurer une routine avec mon bébé. | 0.37 | 0.12 | 0.42 | 0.18 |
| 15 | I have worried that I will become too ill to care for my baby./J'ai eu peur de tomber trop malade pour m'occuper de mon bébé. | 0.01 | 0.41 | 0.22 | 0.22 |
| 16 | I have worried about my baby being accidentally harmed by someone or something./J'ai craint que mon bébé puisse être accidentellement blessé par quelqu'un ou quelque chose. | 0.24 | 0.66 | 0.20 | −0.04 |
| 17 | I have felt unconfident or incapable of meeting my baby's basic care needs./Je me suis sentie pas assez en confiance ou incapable de répondre aux besoins fondamentaux de mon bébé. | 0.64 | 0.13 | 0.21 | 0.12 |
| 18 | I have worried about being unable to settle my baby./J'ai craint d'être incapable de calmer mon bébé. | 0.75 | 0.09 | 0.22 | 0.08 |
| 20 | I have had negative thoughts about my relationship with my baby./J'ai eu des pensées négatives concernant ma relation avec mon bébé. | 0.62 | 0.10 | 0.06 | 0.25 |
| *21 | I have worried more about my relationship with my friends than before my baby was born./Je me suis plus inquiétée de ma relation avec mes amis qu'avant la naissance de mon bébé. | 0.18 | −0.01 | 0.06 | 0.32 |
| *22 | I have thought of ways to avoid exposing my baby to germs./J'ai pensé à des moyens d'éviter d'exposer mon bébé à des germes. | −0.06 | 0.32 | 0.24 | 0.14 |
| 23 | I have worried that my baby is less content than other babies./J'ai craint que mon bébé soit moins heureux que les autres bébés. | 0.52 | 0.36 | −0.07 | 0.36 |
| 24 | I have felt that other mothers are coping with their babies better than me./J'ai senti que d'autres mères se débrouillaient mieux que moi avec leur bébé. | 0.58 | 0.13 | 0.11 | 0.45 |
| 25 | I have felt that I am not the parent I want to be./J'ai senti que je ne suis pas le parent que je veux être. | 0.39 | 0.18 | −0.03 | 0.52 |
| *27 | I have not taken part in an everyday activity with my baby because I fear they may come to harm./Je n'ai pas participé à des activités quotidiennes avec mon bébé car je crains qu'elles puissent lui être préjudiciables. | 0.16 | 0.22 | 0.04 | 0.33 |
| 28 | I have worried about my baby's milk intake./Je me suis inquiétée de la quantité de lait prise par mon bébé. | 0.12 | 0.14 | 0.76 | 0.10 |
| 29 | I have felt that I have had less control over my day than before my baby was born./J'ai eu le sentiment que j'avais moins de contrôle sur ma journée qu'avant la naissance de mon bébé. | 0.21 | −0.08 | 0.34 | 0.22 |
| 31 | I have worried about my baby's health even after reassurance from others./Je me suis inquiétée de la santé de mon bébé même après avoir été rassurée par d'autres personnes. | 0.27 | 0.42 | 0.42 | 0.16 |
| 32 | I have felt that when I do get help it is not beneficial./J'ai senti que lorsque je reçois de l'aide, ce n'est pas bénéfique. | 0.04 | 0.17 | 0.03 | 0.46 |
| 33 | I have worried that my baby will stop breathing while sleeping./J'ai craint que mon bébé ne cesse de respirer pendant son sommeil. | 0.10 | 0.69 | 0.07 | 0.04 |
| 34 | I have used the internet for reassurance about my baby's health./J'ai utilisé Internet pour me rassurer sur la santé de mon bébé. | 0.20 | 0.26 | 0.32 | 0.12 |
| 35 | I have worried about leaving my baby in a childcare setting./Je me suis inquiétée de laisser mon bébé dans un lieu de garde d'enfants. | −0.00 | 0.62 | −0.06 | 0.21 |
| 36 | I have felt that my baby would be better cared for by someone else./J'ai senti que quelqu'un d'autre prendrait mieux soin de mon bébé. | 0.50 | 0.05 | −0.11 | 0.17 |
| 37 | I have worried that I am not going to get enough sleep./Je me suis inquiétée de ne pas réussir à dormir suffisamment. | 0.32 | 0.08 | 0.23 | 0.34 |
| 38 | I have felt that motherhood is much harder than I expected./J'ai trouvé mon rôle de mère beaucoup plus difficile que ce à quoi je m'attendais. | 0.47 | −0.03 | 0.17 | 0.40 |
| 39 | I have worried that my baby is picking up on my anxieties./Je me suis inquiétée que mon bébé soit conscient de mes angoisses. | 0.33 | 0.32 | 0.23 | 0.40 |
| 40 | I have worried about the bond that I have with my baby./Je me suis inquiétée du lien que j'ai avec mon bébé. | 0.51 | 0.18 | 0.13 | 0.43 |
| 41 | I have worried about the length of time that my baby sleeps./Je me suis inquiétée de la durée de sommeil de mon bébé. | 0.28 | 0.22 | 0.16 | 0.37 |
| 44 | I have had difficulty sleeping even when I have had the chance to./J'ai eu des difficultés à m'endormir même quand j'en ai eu l'occasion. | 0.14 | 0.37 | 0.14 | 0.32 |
| 45 | I have worried that other people think that my parenting skills are inadequate./J'ai craint que d'autres personnes pensent que mes compétences parentales sont inadéquates. | 0.28 | 0.26 | 0.08 | 0.53 |
| *46 | I have worried that my partner finds me less attractive than before my baby was born./J'ai craint que mon partenaire ne me trouve moins attirante qu'avant la naissance de mon bébé. | 0.01 | 0.26 | 0.14 | 0.32 |
| 47 | I have worried that my baby is not developing as quickly as other babies./J'ai craint que mon bébé ne se développe pas aussi vite que les autres bébés. | 0.22 | 0.36 | 0.24 | 0.28 |
| *48 | I have felt resentment towards my partner./J'ai eu du ressentiment envers mon partenaire. | −0.02 | 0.06 | 0.09 | 0.43 |
| 49 | I have worried about the way that I feed my baby./Je me suis inquiétée de la façon dont je nourris mon bébé. | 0.17 | 0.14 | 0.67 | 0.20 |
| 50 | I have repeatedly checked on my sleeping baby./Je suis allée surveiller de façon répétée mon bébé pendant son sommeil. | 0.02 | 0.64 | 0.10 | 0.07 |
| 51 | I have felt tired even after a good amount of rest./Je me suis sentie fatiguée même après beaucoup de repos. | 0.12 | 0.38 | 0.16 | 0.33 |
| % of variance explained | 24.81 | 6.26 | 3.97 | 3.57 | |
| Cronbach's alpha | 0.88 | 0.85 | 0.77 | 0.83 | |
- Note: n = 258. Items numbering corresponds to the original 51-item version. Items marked with an asterisk (*) are optional items. All significant loadings are in bold.
- Abbreviation: PSAS-FR, Postpartum Specific Anxiety Scale - French - language.
As in the original PSAS validation study,6 the choice of cross-loading items was made according to a theoretical congruence criterion. Thus, item 1 (“I have felt unable to juggle motherhood with other responsibilities”), loading onto factors 1 and 4, was retained in factor 4. Item 31 (“I have worried about my baby's health even after reassurance from others”), loading onto factors 2 and 3, was included in factor 3 (Table 5).
Finally, the four factors' internal consistency was good to excellent (Cronbach's alpha coefficients ranged from 0.77 to 0.88), which testifies to a high reliability of the PSAS-FR.
3.4 Convergent validity
To assess the convergent validity of the PSAS-FR, Spearman's rank correlation analyses were performed with other validated tools for the screening of anxiety and depression through the first study (n = 258). Spearman's rank was used instead of Pearson's because the data was not normally distributed and displayed a skew towards the right. The correlation coefficients obtained revealed a significant and positive association between the total scores of the PSAS-FR and the anxiety scores of the forms Y-A and Y-B from the STAI inventory, as well as with the scores of the EPDS scale, indicating good convergent validity (Table 6).
- Note: n = 258. 95% CI.
- Abbreviations: CI, confidence interval; EPDS, Edinburgh Postnatal Depression Scale; PSAS-FR, Postpartum Specific Anxiety Scale-French language; STAI-Y, Spielberger State-Trait Anxiety Inventory.
- * p < 0.05.
3.5 Screening accuracy and cut-off score
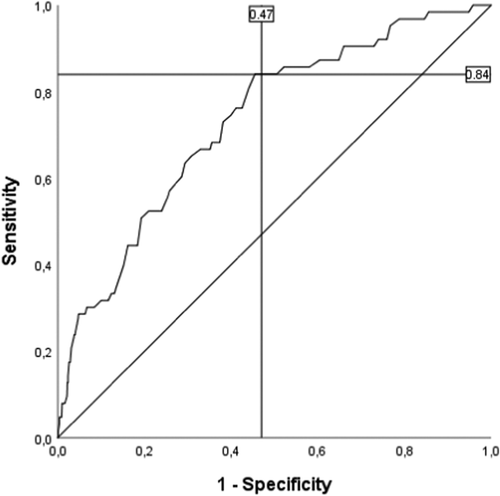
A ROC analysis was performed to assess the screening accuracy of the PSAS-FR and to determine a cut-off score for clinically significant levels of postpartum anxiety. The distinction between participants with and without a current diagnosis of anxiety or depression was used as a criterion to determine true positive and negative rates. The area under the ROC curve (AUC) was 0.73 (SE 0.03; p < 0.001; 95% confidence interval 0.67–0.79) (Figure 2), indicating satisfactory performance of the instrument. The cut-off score retained for screening purposes was 95, with a sensitivity of 0.84 and a specificity of 0.47. The PSAS-FR demonstrated a better screening performance for postpartum anxieties than other validated anxiety and postpartum-specific depression measures, detecting 84% of true positive cases. The STAI-Y A form (State) only identified 67% of women experiencing anxiety, whereas the EPDS revealed a slightly lower performance than the PSAS-FR, identifying 83% of women with psychological distress.
3.6 Test–retest reliability
To explore test–retest reliability, Spearman's rank correlation analyses were conducted for a sub-sample of women (n = 231) who agreed to be re-contacted 15 days after the first administration to complete the PSAS-FR questionnaire. The correlation coefficient obtained was 0.84 (p < 0.001), demonstrating high stability for the PSAS-FR scores.
4 DISCUSSION
The purpose of this study was to validate the PSAS-FR, a 44-item instrument that assesses a wide range of anxieties experienced by women during the first 6 months postpartum. Pilot and psychometric analyses, assessing acceptability, reliability, and validity of the translated instrument, allowed for adaptation of the original scale to the characteristics of the French population. The PSAS-FR demonstrated good acceptability, construct and convergent validity, internal, and test–retest reliability, and the psychometric properties were consistent with those obtained for the original English-language version.6
The exploratory factor analysis suggested a 4-factor structure which explained 38.61% of the cumulative variance of the model. The four dimensions of the PSAS-FR replicated those found in the English-language PSAS6, 15: “Maternal Competence and Attachment Anxieties”; “Infant Safety and Welfare Anxieties”; “Practical Infant Care Anxieties”; and “Psychosocial Adjustment to Motherhood.” The reliability of each factor was good to excellent (Cronbach's alpha ranged between 0.77 and 0.88).
Similar to Fallon et al.6 and Duran,14 low-to-moderate correlations between the items were found, indicating that they do not derive from a unique variable. Except for Items 21, 35, and 43, the remaining items with low communalities values were preserved in the final version. These items correspond to those identified as not being applicable to all mothers in the original instrument.
Items removed from the initial 51-item version appeared to have low performance in identifying French women's postpartum anxieties, which may correspond to a cultural connotation issue (see also Laliberté et al.20). This was also the case of Items 2 (“I have worried more about my relationship with my family than before my baby was born”), 7 (“I have felt that I should not need help to look after my baby”), 42 (“I have worried about returning to work”), and 43 (“I have worried more about my appearance than before my baby was born”) which did not perform well in the recent Turkish PSAS validation study.14 In the present study, the poor performance of Item 2 could be explained by the fact that the postpartum may be a moment of closeness between the mother and the baby characterized by extreme attention to the baby and disinterest towards herself and others,21 and it was described, in the French culture, as a moment that generally leads to appeasement and reconciliation in family relationships, even if temporary.22 Concerning Item 7, the low factor loading could be explained by the fact that there are many public domestic help services in France that support women during the postpartum period.23 The use of these services is therefore widespread among the French population. This could also contribute to explain the low factor loadings of Items 19 (“I felt a greater need to do things in a certain way or in a certain order than before the birth of my baby”) and 26 (“I was more concerned about completing household chores than before the birth of my baby”), meaning that French mothers may feel reduced stress about household tasks and other routines in the postpartum period. In the same way, the low performance of item 30 (“I was more worried about my finances than before the birth of my baby”) may be explained by the fact that French mothers can benefit from maternity and parental (up to 3 years) leave without any threat of losing their jobs, which ensures financial stability for most of them. Regarding Item 42, the mother's return to work does not seem to give rise to fears or anxieties, given that work is one of the main areas of interest for French women alongside their family responsibilities.24 In our sample, 85.7% of mothers were indeed engaged in professional activity. Finally, the low performance of item 43 could reflect the fact that anxieties about physical appearance are not specific to postpartum. French women pay special attention to the 'cult of thinness' regardless of the context of motherhood.25
The PSAS-FR had a positive correlation with previously validated and widely used anxiety and postpartum-specific depression measures such as the STAI and the EPDS scales, which is in agreement with the results obtained by Fallon et al.6, Duran14, and Silverio et al.15; and indicates a good convergent validity. In addition, a stronger link was observed with the STAI Y-B form (Trait), intended to evaluate the general disposition to anxiety, in comparison with the STAI Y-A form (State) measuring situational anxiety. This could be explained by the fact that the anxiety experienced during the postpartum could respond to an exacerbation of psychological vulnerabilities, such as anxiety vulnerability as a character trait, due to the multiple psychological adjustments that motherhood implies.7 Positive correlation with the EPDS is consistent with the results from Dayan3 and Fallon et al.6 and confirms that comorbidity between anxiety and depression may exist in the postpartum.
Test–retest reliability analysis revealed high stability of the PSAS-FR scores. ROC analysis confirmed that the PSAS-FR is a reliable instrument for screening for anxieties during postpartum. The 95-cut-off score retained identified 84% of women with a current diagnosis of anxiety or depression, performing better than the STAI and the EPDS. Sensitivity and specificity were estimated at 0.84 and 0.47 respectively, values which are coherent with those obtained by the authors of the original English-language versions.6, 15 These results highlight the relevance of using PSAS-FR, an instrument that detects clinical levels of anxiety in new mothers that is specific to the postnatal period, compared with other validated measures of general anxiety.
4.1 Limitations
Future research will be necessary to address the limitations of this study. Firstly, the sample was mainly composed of French women (89%), which implies the need to assess the performance of the PSAS-FR with other francophone samples. As in Fallon et al.6, this study employed an online data collection, which allows less control over the sampling. Our sample is not sufficiently representative of at-risk populations, indicating the need to evaluate the PSAS-FR performance with other samples of mothers, such as those with poor social support, high levels of social complexity and multiple disadvantage, or having a personal or familial history of mental disorders.
Since the English-language PSAS proved to be a better predictor of infant12 and maternal13 outcomes than general anxiety measures, further lines of research may focus on the assessment of the predictive validity of the PSAS-FR in the context of different maternal and infant perinatal issues. Assessing the psychometric performance of the recently developed French-language Postpartum Specific Anxiety Scale – Research Short Form for use in Crises (PSAS-FR-RSF-C15) as well as developing a French short form, would be welcome to improve the use of the PSAS-FR in the clinical field.
5 CONCLUSION
The PSAS-FR appears to be a valid and reliable tool to measure and screen for postpartum anxieties in the French population, meeting both research and clinical field purposes. Future research is needed to assess the performance of this instrument with other francophone samples and clinical populations. It is also recommended to evaluate the predictive validity of the PSAS-FR in diverse contexts of maternal and infant perinatal issues as well as developing a French brief form.
6 IMPLICATIONS FOR NURSING PRACTICE
Health care professionals could benefit from using the PSAS-FR to screen for maternal and infant-related anxieties during the first 6 months postpartum, which allows early detection and treatment, leading to better maternal and infant outcomes.
ACKNOWLEDGMENTS
The authors gratefully acknowledge the help of Aude Demanche and Céline Schaming during data collection and the assistance of Lise Michel with back-translation. This study did not receive any funding. Sergio A. Silverio (King's College London) is supported by the National Institute for Health Research Applied Research Collaboration South London (NIHR ARC South London) at King's College Hospital NHS Foundation Trust. The views expressed are those of the authors and not necessarily those of the NIHR or the Department of Health and Social Care. All other authors have no conflicts of interest to declare.
CONFLICT OF INTERESTS
The authors declare that there are no conflict of interests.
Open Research
DATA AVAILABILITY STATEMENT
The data set used and analyzed during the current study is available from the corresponding author on reasonable request.




