Kidney Transplantation in ≤15 kg Children: Outcomes and Prognostic Indicators—A Review of the Organ Procurement and Transplantation Database
ABSTRACT
Background
Approximately 2500 pediatric patients are awaiting kidney transplantation in the United States, with <5% comprising those ≤15 kg. Transplant in this cohort is often delayed by center-based growth parameters, often necessitating transplantation after the initiation of dialysis. Furthermore, prognostication remains somewhat ambiguous. In this report, we scrutinize the Organ Procurement and Transplantation Network (OPTN) data from 2001 to 2021 to help better understand specific variables impacting graft and patient outcomes in these children.
Methods
The OPTN kidney transplant dataset from 2001 to 2021 was analyzed. Inclusion criteria included age <18 years, weight ≤15 kg, and recipient of primary living donor kidney transplantation (LDKT) or deceased donor kidney transplantation (DDKT). Patient and graft survival probabilities were calculated using the Kaplan–Meier method. The Cox proportional hazards model was used to calculate hazard ratio (HR) and identify variables significantly associated with patient and graft survival.
Results
Two thousand one hundred sixty-eight pediatric transplant recipients met inclusion criteria. Patient survival at 1 and 3 years was 98% and 97%, respectively. Graft survival at 1 and 3 years was 95% and 92%, respectively. Dialysis was the sole significant variable impacting both patient and graft survival. Graft survival was further impacted by transplant era, recipient gender and ethnicity, and donor type. Infants transplanted at Age 1 had better graft survival compared with older children, and nephrotic syndrome was likewise associated with a better prognosis.
Conclusion
Pediatric kidney transplantation is highly successful. The balance between preemptive transplantation, medical optimization, and satisfactory technical parameters seems to suggest a “Goldilocks zone” for many children, favoring transplantation between 1 and 2 years of age.
Abbreviations
-
- CI
-
- confidence interval
-
- DDKT
-
- deceased donor kidney transplantation
-
- FSGS
-
- focal segmental glomerulosclerosis
-
- HR
-
- hazard ratio
-
- KDPI
-
- kidney donor profile index
-
- LDKT
-
- living donor kidney transplantation
-
- NAPRTCS
-
- North American Pediatric Renal Trials and Collaborative Studies
-
- OPTN
-
- Organ Procurement and Transplantation Network
-
- SD
-
- standard deviation
-
- SE
-
- standard error
1 Introduction
In the United States, approximately 700–800 pediatric kidney transplant procedures are performed each year, whereas an additional 2500 pediatric patients are on the waitlist. The majority of these waitlist patients are between 12 and 17 years old, and roughly 20% are under the age of 6 [1]. The most common indications relate to congenital anomalies of the kidney and genitourinary tract, including aplasia/hypoplasia/dysplasia and defects of the genitourinary tract [1]. Transplantation affords a massive benefit in life expectancy in pediatric patients, upward of 25 to 30 years when compared to remaining dialysis [2]. Additional advantages include augmented physical growth, neurocognitive development, and enhanced quality of life for both patients and their families [3].
Small children represent a small proportion of the pediatric transplant population, with those under 1 year of age comprising <5% of the total [4]. These patients often pose specific challenges to transplantation, including the necessity to repair underlying urologic anomalies, coping with donor-recipient size disparities, nutrition, neurologic, and metabolic comorbidities. Despite these challenges, the patient and graft survival for recipients ≤15 kg has been excellent in the modern era. Multiple studies comparing kidney transplants in recipients ≤15 kg versus those >15 kg found no difference in outcomes related to patient and graft survival [5-8]. Other studies have shown that it is possible to achieve >80% graft survival up to 10 years posttransplant even in this high-risk populace [9].
Prior studies commonly consolidated pediatric patients into a single category when looking at outcomes and associated risk factors, including donor and recipient parameters. Variables implicated in worse outcomes include transplantation after the initiation of dialysis, deceased donation, prolonged graft ischemia, increasing donor age, decreasing recipient age/weight, era of transplantation, race, and socioeconomic status [9-19]. Overall outcomes for children weighing ≤15 kg have been encouraging, reporting 73%–92% graft survival at 5 years and >80% graft survival at 10 years [6, 20-25]. The aim of this study was the retrospective analysis of the outcomes and prognostic indicators for patients in the ≤15 kg weight range.
2 Materials and Methods
After obtaining approval from the University of Southern California Biomedical Institutional Review Board, primary pediatric kidney transplant procedures were identified from the Organ Procurement and Transplantation Network (OPTN) database during the period January 2001 through March 2021. Inclusion criteria included age <18 years of age, weight ≤15 kg, and recipient of primary kidney transplant from a living donor or a deceased after brain death donor. Exclusion criteria included recipient of other organs, re-transplant procedure, and recipient of a decreased after cardiac death donor organ.
The following data were collected for all recipients: age, sex, race, height, weight, date of transplant, dialysis status, and patient and graft outcomes. Indications for kidney transplant were scrutinized and categorized as hypoplasia/dysplasia, hypoperfusion injury, reflux nephropathy, nephrotic syndrome, glomerulonephritis, cystic/tubular kidney disease, and “other.” Donor data were collected including demographics, donor kidney donor profile index (KDPI), donor height and weight, cigarette use, donor type (live donor kidney transplantation [LDKT] vs. deceased donor kidney transplantation [DDKT]), and terminal creatinine. Table 1 includes the baseline data collected for each of the variables to be analyzed.
| Variables | n (%) |
|---|---|
| Recipient age, years, mean (SD) | 2.3 (1.4) |
| Recipient age, years | |
| 0 | 32 (1.5) |
| 1 | 641 (29.6) |
| 2 | 715 (33.0) |
| 3–10 | 780 (36.0) |
| Recipient height, cm, mean (SD) | 83.2 (8.6) |
| Recipient height, cm | |
| <80 | 726 (33.9) |
| 80–89 | 930 (43.4) |
| ≥90 | 485 (22.7) |
| Recipient weight, kg, mean (SD) | 11.9 (1.9) |
| Recipient weight, kg | |
| <9 | 126 (5.8) |
| 9–10 | 539 (24.9) |
| ≥11 | 1503 (69.3) |
| Recipient sex | |
| Male | 1454 (67.1) |
| Female | 714 (32.9) |
| Recipient race/ethnicity | |
| White | 1289 (59.5) |
| Black | 309 (14.3) |
| Hispanic | 427 (19.7) |
| Other | 143 (6.6) |
| Recipient dialysis | |
| No | 540 (25.2) |
| Yes | 1601 (74.8) |
| Time on dialysis | |
| <1 year | 532 (34.7) |
| ≥1 year | 1000 (65.3) |
| Transplant indication | |
| Hypoplasia/dysplasia | 612 (28.4) |
| Hypoperfusion injury | 130 (6.0) |
| Reflux nephropathy | 712 (33.0) |
| Glomerulonephritis | 81 (3.8) |
| Cystic/tubular kidney disease | 187 (8.7) |
| Nephrotic syndrome | 276 (12.8) |
| Other | 160 (7.4) |
| Donor age, years, mean (SD) | 28.1 (10.1) |
| Donor age, years | |
| ≤5 | 41 (1.9) |
| 6–10 | 57 (2.6) |
| 11–17 | 210 (9.7) |
| 18–39 | 1601 (73.9) |
| ≥40 | 259 (12.0) |
| Donor sex | |
| Male | 1153 (53.2) |
| Female | 1015 (46.8) |
| Donor race/ethnicity | |
| White | 1454 (67.1) |
| Black | 267 (12.3) |
| Hispanic | 371 (17.1) |
| Other | 76 (3.5) |
| Donor height, cm, mean (SD) | 168.1 (16.6) |
| Donor height, cm | |
| <170 | 999 (47.6) |
| 170–179 | 642 (30.6) |
| ≥180 | 458 (21.8) |
| Donor weight, kg, mean (SD) | 73.1 (19.7) |
| Donor weight, kg | |
| 0–29 | 68 (3.2) |
| 30–69 | 858 (40.4) |
| ≥70 | 1196 (56.4) |
| Donor terminal creatinine | |
| <1 | 614 (66.2) |
| ≥1 | 313 (33.8) |
| Donor cigarette use | |
| No | 1581 (85.6) |
| Yes | 267 (14.5) |
| KDPI | |
| 0–10 | 421 (45.5) |
| 11–20 | 257 (27.8) |
| ≥21 | 248 (26.8) |
| Donor type | |
| Deceased donor | 929 (42.9) |
| Living donor | 1239 (57.2) |
| Transplant era | |
| 2001–2010 | 1048 (48.3) |
| 2011–2021 | 1120 (51.7) |
- Abbreviations: KDPI, kidney donor profile index; SD, standard deviation.
Patient and graft survival probabilities were calculated using the Kaplan–Meier method. Patient survival was defined as the time between transplant and death. Graft survival was defined as the time between transplant and graft loss or death. Patients who were alive without experiencing an event were censored at the last date of follow-up.
The Cox proportional hazards model was used to calculate hazard ratio (HR) and to identify variables significantly associated with patient and graft survival. The multivariate models were adjusted for the recipient variables age, height, and weight, and variables univariately significant with a p value < 0.2 were included. The interaction between recipient and donor variables was then assessed by examining the effect of recipient age, height, and weight on patient and graft survival at different levels of donor age, height, and weight. p values ≤ 0.05 were considered statistically significant. Statistical analyses were performed using the SAS 9.4 (SAS Institute Inc., Cary, NC) and R 4.1.2 [26].
3 Results
In total, 2168 pediatric recipients meeting these criteria were identified. All patients were aged 10 or less with the majority between 1 and 4 years. The mean age was 2.3 years. The majority were male (67.1%), white (59.5%), and greater than or equal to 11 kg (69.3%). Most had been on dialysis (74.8%) with 65.3% on dialysis greater than or equal to 1 year. The two most common indication categories included reflux nephropathy (33%) and renal hypoplasia/dysplasia (28.4%). Mean donor age was 28.1 years with the majority aged 18 to 39 years (73.9%). This included 53.2% male, 67.1% white, and 57.2% living donors. Two transplant eras were examined including 2001 through 2010 (48.3%) and 2011 through March 2021 (51.7%). Of note, in our analysis we combined small categories of familial focal segmental glomerulosclerosis (FSGS) and other nephrotic subtypes into the larger category of nephrotic syndrome. The number of cases in each subtype was too small to be kept in separate groups in the analysis.
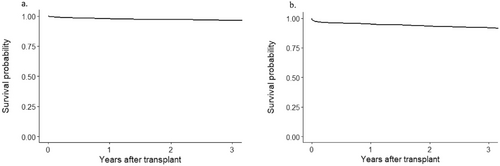
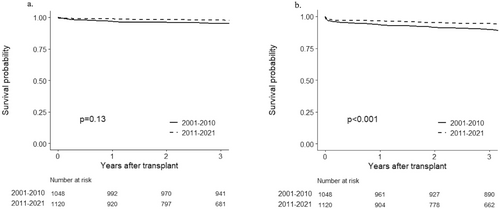
Overall patient survival at 1 and 3 years was 98% and 97%, respectively (Figure 1a). Graft survival at 1 and 3 years was 95% and 92%, respectively (Figure 1b). There were 108 patients who died with causes of death outlined in Table 2. In regard to graft loss, we have outlined the causes of graft failure in Table 3. Please note that in the database, there are an extremely large number of overlapping causes of graft loss and many reporters do not provide precise categories, but only include “other,” “unknown,” or multiple causes. These data have been collated as best as possible but has limitations as above. Analyzing the patient and graft survival according to era demonstrated the improvement in graft survival for the modern era of 2011 through March 2021 (Figure 2a,b). 3-year patient survival was 95% in the early transplant era and 98% in the modern transplant era. 3-year graft survival was 90% in the early transplant era compared with 94% in the modern transplant era (p < 0.001).
| Causes of death | N = 108 (%) |
|---|---|
| Cardiovascular | 8 (7) |
| Cerebrovascular | 3 (3) |
| Graft failure | 2 (2) |
| Hemorrhage | 1 (1) |
| Infection | 17 (16) |
| Malignancy | 7 (6) |
| Multisystem organ failure ± infection | 5 (5) |
| Respiratory failure (various causes) | 25 (23) |
| Trauma | 2 (2) |
| Other | 16 (15) |
| Unknown | 22 (20) |
| Causes of graft loss | N = 382 (%) |
|---|---|
| Acute rejection | 42 (11) |
| BK (Polyoma) virus | 5 (1) |
| Chronic allograft nephropathy | 32 (8) |
| Chronic rejection | 186 (49) |
| Death | 7 (2) |
| Graft thrombosis | 35 (9) |
| Infection | 11 (3) |
| Other/unknown | 22 (6) |
| Primary nonfunction | 17 (4) |
| Recurrent disease | 15 (4) |
| Surgical complications | 4 (1) |
| Urologic complications | 6 (2) |
Univariate analysis revealed the following factors for selection into a multivariate model for patient survival: recipient height, weight, gender, dialysis status, donor weight, donor cigarette use, and transplant era (Table 4). Multivariable analysis demonstrated that recipient dialysis status was associated with a higher risk of death (HR = 2.05; 95% confidence interval [CI], 1.11–3.79; p = 0.021) (Table 5).
| Variables | n | Number of events | 1 Year | 3 Years | HR (95% CI) | p |
|---|---|---|---|---|---|---|
| Patient survival ± SE (%) | Patient survival ± SE (%) | |||||
| Recipient age, years | ||||||
| 0 | 32 | 5 | 91 ± 5.2 | 91 ± 5.2 | 2.29 (0.90–5.82) | 0.46 |
| 1 | 641 | 37 | 98 ± 0.6 | 96 ± 0.8 | 1.00 (0.63–1.56) | |
| 2 | 715 | 36 | 98 ± 0.5 | 97 ± 0.7 | 1.00 (0.63–1.55) | |
| 3–10 | 780 | 39 | 98 ± 0.5 | 97 ± 0.6 | 1.0 | |
| Recipient height, cm | ||||||
| <80 | 726 | 51 | 97 ± 0.7 | 95 ± 0.8 | 1.62 (0.93–2.81) | 0.18 |
| 80–89 | 930 | 44 | 98 ± 0.4 | 97 ± 0.6 | 1.27 (0.73–2.23) | |
| ≥90 | 485 | 17 | 99 ± 0.5 | 98 ± 0.7 | 1.0 | |
| Recipient weight, kg | ||||||
| <9 | 126 | 9 | 94 ± 2.1 | 93 ± 2.2 | 1.28 (0.64–2.57) | 0.18 |
| 9–10 | 539 | 40 | 98 ± 0.6 | 96 ± 0.9 | 1.45 (0.98–2.14) | |
| ≥11 | 1503 | 68 | 98 ± 0.4 | 97 ± 0.5 | 1.0 | |
| Recipient sex | ||||||
| Male | 1454 | 70 | 98 ± 0.4 | 97 ± 0.5 | 1.0 | 0.11 |
| Female | 714 | 47 | 97 ± 0.6 | 96 ± 0.7 | 1.36 (0.94–1.97) | |
| Recipient race/ethnicity | ||||||
| White | 1289 | 70 | 98 ± 0.4 | 97 ± 0.5 | 1.0 | 0.39 |
| Black | 309 | 22 | 97 ± 1.0 | 95 ± 1.3 | 1.32 (0.82–2.14) | |
| Hispanic | 427 | 21 | 98 ± 0.8 | 97 ± 0.9 | 0.94 (0.58–1.53) | |
| Other | 143 | 4 | 99 ± 0.7 | 98 ± 1.1 | 0.59 (0.21–1.61) | |
| Recipient dialysis | ||||||
| No | 540 | 21 | 97 ± 0.4 | 96 ± 0.5 | 1.0 | 0.069 |
| Yes | 1601 | 94 | 99 ± 0.5 | 98 ± 0.7 | 1.52 (0.95–2.44) | |
| Time on dialysis | ||||||
| <1 year | 532 | 27 | 98 ± 0.6 | 97 ± 0.8 | 1.0 | 0.31 |
| ≥1 year | 1000 | 57 | 97 ± 0.5 | 96 ± 0.6 | 1.26 (0.80–2.00) | |
| Transplant indication | ||||||
| Hypoplasia/dysplasia | 612 | 34 | 97 ± 0.7 | 96 ± 0.9 | 1.0 | 0.73 |
| Hypoperfusion injury | 130 | 9 | 97 ± 1.5 | 96 ± 1.8 | 1.11 (0.53–2.31) | |
| Reflux nephropathy | 712 | 30 | 98 ± 0.6 | 97 ± 0.6 | 0.72 (0.44–1.18) | |
| Glomerulonephritis | 81 | 5 | 100 | 99 ± 1.4 | 0.85 (0.33–2.18) | |
| Cystic/tubular kidney disease | 187 | 14 | 98 ± 1.1 | 96 ± 1.5 | 1.23 (0.66–2.29) | |
| Nephrotic syndrome | 276 | 16 | 99 ± 0.7 | 96 ± 1.2 | 0.97 (0.53–1.75) | |
| Other | 160 | 9 | 97 ± 1.4 | 96 ± 1.6 | 0.97 (0.47–2.02) | |
| Donor age, years | ||||||
| ≤5 | 41 | 6 | 95 ± 3.4 | 95 ± 3.4 | 2.49 (0.96–6.50) | 0.33 |
| 6–10 | 57 | 2 | 98 ± 1.8 | 98 ± 1.8 | 0.61 (0.14–2.67) | |
| 11–17 | 210 | 9 | 99 ± 0.7 | 97 ± 1.2 | 0.85 (0.37–1.97) | |
| 18–39 | 1601 | 86 | 98 ± 0.4 | 97 ± 0.5 | 1.05 (0.60–1.85) | |
| ≥40 | 259 | 14 | 97 ± 1.0 | 96 ± 1.3 | 1.0 | |
| Donor sex | ||||||
| Male | 1153 | 56 | 98 ± 0.4 | 97 ± 0.5 | 1.0 | 0.26 |
| Female | 1015 | 61 | 97 ± 0.5 | 96 ± 0.6 | 1.23 (0.86–1.77) | |
| Donor race/ethnicity | ||||||
| White | 1454 | 81 | 98 ± 0.4 | 96 ± 0.5 | 1.0 | 0.40 |
| Black | 267 | 16 | 97 ± 1.0 | 96 ± 1.2 | 1.07 (0.63–1.83) | |
| Hispanic | 371 | 19 | 99 ± 0.6 | 97 ± 1.0 | 0.98 (0.60–1.62) | |
| Other | 76 | 1 | 99 ± 1.4 | 99 ± 1.4 | 0.27 (0.04–1.90) | |
| Donor height, cm | ||||||
| <170 | 999 | 51 | 98 ± 0.5 | 97 ± 0.6 | 0.98 (0.60–1.59) | 0.67 |
| 170–179 | 642 | 38 | 98 ± 0.6 | 97 ± 0.8 | 1.18 (0.71–1.97) | |
| ≥180 | 458 | 24 | 97 ± 0.8 | 97 ± 0.9 | 1.0 | |
| Donor weight, kg | ||||||
| 0–29 | 68 | 5 | 98 ± 1.5 | 97 ± 2.1 | 0.98 (0.40–2.42) | 0.066 |
| 30–69 | 858 | 34 | 98 ± 0.5 | 97 ± 0.6 | 0.63 (0.42–0.94) | |
| ≥70 | 1196 | 74 | 98 ± 0.4 | 96 ± 0.6 | 1.0 | |
| Donor terminal creatinine | ||||||
| <1 | 614 | 29 | 98 ± 0.5 | 97 ± 0.7 | 1.0 | 0.29 |
| ≥1 | 313 | 20 | 97 ± 1.0 | 95 ± 1.2 | 1.36 (0.78–2.37) | |
| Donor cigarette use | ||||||
| No | 1581 | 83 | 98 ± 0.8 | 97 ± 1.1 | 1.0 | 0.10 |
| Yes | 267 | 9 | 98 ± 0.4 | 97 ± 0.5 | 0.59 (0.29–1.17) | |
| KDPI | ||||||
| 0–10 | 421 | 26 | 98 ± 0.7 | 97 ± 1.0 | 1.0 | 0.42 |
| 11–20 | 257 | 10 | 98 ± 0.9 | 97 ± 1.0 | 0.62 (0.30–1.29) | |
| ≥20 | 248 | 15 | 98 ± 0.9 | 96 ± 1.3 | 0.83 (0.44–1.57) | |
| Donor type | ||||||
| Deceased donor | 929 | 51 | 98 ± 0.5 | 97 ± 0.6 | 1.0 | 0.38 |
| Living donor | 1239 | 66 | 98 ± 0.4 | 96 ± 0.5 | 0.85 (0.59–1.22) | |
| Transplant era | ||||||
| 2001–2010 | 1048 | 82 | 97 ± 0.6 | 95 ± 0.7 | 1.0 | 0.13 |
| 2011–2021 | 1120 | 35 | 99 ± 0.3 | 98 ± 0.5 | 0.73 (0.48–1.11) | |
- Abbreviations: CI, confidence interval; HR, hazard ratio; KDPI, kidney donor profile index; SE, standard error.
| Variables | HR (95% CI) | p |
|---|---|---|
| Recipient age, years | ||
| 0 | 0.82 (0.17–3.88) | 0.8 |
| 1 | 0.58 (0.30–1.12) | 0.1 |
| 2 | 0.70 (0.40–1.23) | 0.21 |
| 3–10 | 1.0 | |
| Recipient height, cm | ||
| <80 | 2.24 (0.99–5.03) | 0.052 |
| 80–89 | 1.58 (0.81–3.08) | 0.18 |
| ≥90 | 1.0 | |
| Recipient weight, kg | ||
| <9 | 1.16 (0.44–3.07) | 0.77 |
| 9–10 | 1.18 (0.69–2.01) | 0.55 |
| ≥11 | 1.0 | |
| Recipient sex | ||
| Male | 1.0 | |
| Female | 1.43 (0.93–2.19) | 0.1 |
| Recipient dialysis | ||
| No | 1.0 | |
| Yes | 2.05 (1.11–3.79) | 0.021 |
| Donor weight, kg | ||
| 0–29 | 0.77 (0.30–1.96) | 0.58 |
| 30–69 | 0.64 (0.41–1.01) | 0.054 |
| ≥70 | 1.0 | |
| Donor cigarette use | ||
| No | 1.0 | |
| Yes | 0.59 (0.29–1.18) | 0.13 |
| Transplant era | ||
| 2001–2010 | 1.0 | |
| 2011–2021 | 0.77 (0.48–1.23) | 0.27 |
- Note: Boldface values indicate statistical significance.
- Abbreviations: CI, confidence interval; HR, hazard ratio.
The same analysis was performed to identify factors for selection into a multivariate model for graft survival. Recipient variables included age, height, weight, gender, ethnicity, dialysis status, transplant indication, and transplant era. Donor variables were age, gender, ethnicity, height, weight, terminal creatinine, KDPI, type (living/deceased), and cigarette use (Table 6).
| Variables | n | Number of events | 1 Year | 3 Years | HR (95% CI) | p |
|---|---|---|---|---|---|---|
| Graft survival ± SE (%) | Graft survival ± SE (%) | |||||
| Recipient age, years | ||||||
| 0 | 32 | 12 | 84 ± 6.4 | 84 ± 6.4 | 0.90 (0.50–1.61) | 0.15 |
| 1 | 641 | 152 | 94 ± 0.9 | 90 ± 1.2 | 0.78 (0.63–0.97) | |
| 2 | 715 | 152 | 95 ± 0.8 | 93 ± 1.0 | 0.86 (0.69–1.06) | |
| 3–10 | 780 | 181 | 96 ± 0.7 | 93 ± 1.0 | 1.0 | |
| Recipient height, cm | ||||||
| <80 | 726 | 197 | 94 ± 0.9 | 90 ± 1.1 | 1.02 (0.79–1.31) | 0.98 |
| 80–89 | 930 | 196 | 96 ± 0.7 | 92 ± 0.9 | 1.02 (0.80–1.31) | |
| ≥90 | 485 | 91 | 97 ± 0.8 | 95 ± 1.1 | 1.0 | |
| Recipient weight, kg | ||||||
| <9 | 126 | 42 | 92 ± 2.4 | 88 ± 3.0 | 1.10 (0.80–1.52) | 0.59 |
| 9–10 | 539 | 149 | 95 ± 1.0 | 90 ± 1.3 | 1.10 (0.91–1.34) | |
| ≥11 | 1503 | 306 | 95 ± 0.6 | 93 ± 0.7 | 1.0 | |
| Recipient sex | ||||||
| Male | 1454 | 313 | 96 ± 0.5 | 93 ± 0.7 | 1.0 | 0.028 |
| Female | 714 | 184 | 94 ± 0.9 | 91 ± 1.1 | 1.23 (1.03–1.48) | |
| Recipient race/ethnicity | ||||||
| White | 1289 | 262 | 95 ± 0.6 | 93 ± 0.8 | 1.0 | <0.001 |
| Black | 309 | 97 | 95 ± 1.3 | 90 ± 1.7 | 1.74 (1.38–2.20) | |
| Hispanic | 427 | 105 | 94 ± 1.1 | 92 ± 1.4 | 1.33 (1.06–1.66) | |
| Other | 143 | 33 | 94 ± 2.1 | 89 ± 2.7 | 1.60 (1.11–2.30) | |
| Recipient dialysis | ||||||
| No | 540 | 106 | 94 ± 0.6 | 91 ± 0.7 | 1.0 | 0.029 |
| Yes | 1601 | 386 | 97 ± 0.8 | 95 ± 1.0 | 1.26 (1.02–1.57) | |
| Time on dialysis | ||||||
| <1 year | 532 | 134 | 96 ± 0.9 | 91 ± 1.3 | 1.0 | 0.35 |
| ≥1 year | 1000 | 227 | 94 ± 0.8 | 91 ± 0.9 | 1.11 (0.89–1.37) | |
| Transplant indication | ||||||
| Hypoplasia/dysplasia | 612 | 147 | 94 ± 1.0 | 91 ± 1.2 | 1.0 | 0.072 |
| Hypoperfusion injury | 130 | 34 | 93 ± 2.3 | 92 ± 2.4 | 0.87 (0.60–1.27) | |
| Reflux nephropathy | 712 | 162 | 95 ± 0.8 | 92 ± 1.0 | 0.86 (0.69–1.08) | |
| Glomerulonephritis | 81 | 20 | 95 ± 2.5 | 88 ± 3.7 | 0.66 (0.42–1.06) | |
| Cystic/tubular kidney disease | 187 | 50 | 97 ± 1.2 | 91 ± 2.2 | 0.98 (0.71–1.35) | |
| Nephrotic syndrome | 276 | 52 | 96 ± 1.1 | 94 ± 1.4 | 0.65 (0.47–0.89) | |
| Other | 160 | 32 | 95 ± 1.8 | 93 ± 2.1 | 0.70 (0.48–1.02) | |
| Donor age, years | ||||||
| ≤5 | 41 | 20 | 85 ± 5.5 | 75 ± 6.9 | 2.07 (1.26–3.42) | 0.003 |
| 6–10 | 57 | 17 | 96 ± 2.5 | 95 ± 3.1 | 1.09 (0.64–1.86) | |
| 11–17 | 210 | 56 | 94 ± 1.6 | 86 ± 2.5 | 1.30 (0.91–1.86) | |
| 18–39 | 1601 | 339 | 95 ± 0.5 | 93 ± 0.7 | 0.91 (0.70–1.19) | |
| ≥40 | 259 | 65 | 96 ± 1.3 | 93 ± 1.7 | 1.0 | |
| Donor sex | ||||||
| Male | 1153 | 253 | 95 ± 0.6 | 93 ± 0.8 | 1.0 | 0.17 |
| Female | 1015 | 244 | 95 ± 0.7 | 91 ± 0.9 | 1.13 (0.95–1.35) | |
| Donor race/ethnicity | ||||||
| White | 1454 | 318 | 96 ± 0.5 | 92 ± 0.7 | 1.0 | 0.030 |
| Black | 267 | 73 | 95 ± 1.4 | 92 ± 1.7 | 1.37 (1.06–1.77) | |
| Hispanic | 371 | 93 | 93 ± 1.3 | 90 ± 1.6 | 1.32 (1.04–1.66) | |
| Other | 76 | 13 | 96 ± 2.3 | 93 ± 3.0 | 1.07 (0.61–1.86) | |
| Donor height, cm | ||||||
| <170 | 999 | 247 | 95 ± 0.7 | 91 ± 1.0 | 1.44 (1.13–1.84) | 0.003 |
| 170–179 | 642 | 137 | 94 ± 0.9 | 92 ± 1.1 | 1.23 (0.94–1.61) | |
| ≥180 | 458 | 88 | 96 ± 0.9 | 94 ± 1.1 | 1.0 | |
| Donor weight, kg | ||||||
| 0–29 | 68 | 28 | 91 ± 3.5 | 83 ± 4.6 | 1.62 (1.10–2.39) | 0.070 |
| 30–69 | 858 | 187 | 95 ± 0.8 | 92 ± 1.0 | 1.00 (0.83–1.21) | |
| ≥70 | 1196 | 261 | 95 ± 0.6 | 93 ± 0.8 | 1.0 | |
| Donor terminal creatinine | ||||||
| <1 | 614 | 152 | 95 ± 0.9 | 90 ± 1.3 | 1.0 | 0.79 |
| ≥1 | 313 | 76 | 92 ± 1.5 | 90 ± 1.8 | 0.96 (0.73–1.27) | |
| Donor cigarette use | ||||||
| No | 1581 | 314 | 96 ± 1.2 | 94 ± 1.5 | 1.0 | 0.076 |
| Yes | 267 | 45 | 95 ± 0.6 | 92 ± 0.7 | 0.76 (0.56–1.04) | |
| KDPI | ||||||
| 0–10 | 421 | 94 | 94 ± 1.2 | 89 ± 1.6 | 1.0 | 0.75 |
| 11–20 | 257 | 59 | 94 ± 1.5 | 91 ± 1.8 | 1.05 (0.76–1.46) | |
| ≥21 | 248 | 74 | 94 ± 1.5 | 89 ± 2.1 | 1.13 (0.83–1.53) | |
| Donor type | ||||||
| Deceased donor | 929 | 228 | 94 ± 0.8 | 90 ± 1.0 | 1.0 | <0.001 |
| Living donor | 1239 | 269 | 96 ± 0.6 | 93 ± 0.7 | 0.65 (0.54–0.77) | |
| Transplant era | ||||||
| 2001–2010 | 1048 | 399 | 93 ± 0.8 | 90 ± 0.9 | 1.0 | <0.001 |
| 2011–2021 | 1120 | 98 | 97 ± 0.5 | 94 ± 0.7 | 0.66 (0.52–0.84) | |
- Note: Boldface values indicate statistical significance.
- Abbreviations: CI, confidence interval; HR, hazard ratio; KDPI, kidney donor profile index; SE, standard error.
Recipient female sex (HR = 1.34; 95% CI, 1.05–1.70; p = 0.019) and recipient dialysis (HR = 1.63; 95% CI, 1.23–2.17; p < 0.001) were associated with decreased graft survival. LDKT (HR = 0.63; 95% CI, 0.48–0.83; p = 0.001) and the modern transplant era (HR = 0.61; 95% CI, 0.47–0.79; p < 0.001) were associated with improved graft survival. Transplant indication significantly impacted graft survival, with nephrotic syndrome associated with better graft survival compared with hypoplasia/dysplasia (HR = 0.52; 95% CI, 0.35 to 0.77; p = 0.001). Non-White recipients had lower rates of graft survival at 3 years compared with White recipients, with statistically significant lower survival among Black recipients (HR = 1.42; 95% CI, 1.04–1.93; p = 0.029). 1-year-old transplant recipients had better graft survival compared with 3 to 10-year-old patients (Table 7).
| Variables | HR (95% CI) | p |
|---|---|---|
| Recipient age, years | ||
| 0 | 0.77 (0.32–1.89) | 0.57 |
| 1 | 0.69 (0.49–0.97) | 0.032 |
| 2 | 0.79 (0.59–1.05) | 0.10 |
| 3–10 | 1.0 | |
| Recipient height, cm | ||
| <80 | 1.04 (0.69–1.58) | 0.85 |
| 80–89 | 1.15 (0.83–1.59) | 0.40 |
| ≥90 | 1.0 | |
| Recipient weight, kg | ||
| <9 | 1.31 (0.77–2.20) | 0.32 |
| 9–10 | 1.38 (1.04–1.83) | 0.027 |
| ≥11 | 1.0 | |
| Recipient sex | ||
| Male | 1.0 | |
| Female | 1.34 (1.05–1.70) | 0.019 |
| Recipient race/ethnicity | ||
| White | 1 | |
| Black | 1.42 (1.04–1.93) | 0.029 |
| Hispanic | 1.06 (0.78–1.44) | 0.71 |
| Other | 1.45 (0.94–2.22) | 0.09 |
| Recipient dialysis | ||
| No | 1.0 | |
| Yes | 1.63 (1.23–2.17) | <0.001 |
| Transplant indication | ||
| Hypoplasia/dysplasia | 1.0 | |
| Hypoperfusion injury | 0.83 (0.52–1.31) | 0.41 |
| Reflux nephropathy | 1.11 (0.84–1.47) | 0.48 |
| Glomerulonephritis | 0.72 (0.41–1.27) | 0.26 |
| Cystic/tubular kidney disease | 1.19 (0.81–1.75) | 0.38 |
| Nephrotic syndrome | 0.52 (0.35–0.77) | 0.001 |
| Other | 0.70 (0.44–1.12) | 0.14 |
| Donor age, years | ||
| ≤5 | 1.01 (0.32–3.19) | 0.98 |
| 6–10 | 0.59 (0.26–1.33) | 0.20 |
| 11–17 | 0.70 (0.44–1.12) | 0.14 |
| 18–39 | 0.71 (0.50–1.02) | 0.06 |
| ≥40 | 1.0 | |
| Donor sex | ||
| Male | 1.0 | |
| Female | 1.13 (0.86–1.49) | 0.39 |
| Donor race/ethnicity | ||
| White | 1.0 | |
| Black | 0.86 (0.61–1.21) | 0.38 |
| Hispanic | 1.08 (0.79–1.48) | 0.64 |
| Other | 0.74 (0.39–1.42) | 0.37 |
| Donor height, cm | ||
| <170 | 1.38 (0.94–2.00) | 0.10 |
| 170–179 | 1.28 (0.92–1.79) | 0.14 |
| ≥ 180 | 1.0 | |
| Donor weight, kg | ||
| 0–29 | 0.91 (0.34–2.44) | 0.86 |
| 30–69 | 0.87 (0.67–1.12) | 0.28 |
| ≥70 | 1.0 | |
| Donor cigarette use | ||
| No | 1.0 | |
| Yes | 0.74 (0.53–1.04) | 0.08 |
| Donor type | ||
| Deceased donor | 1.0 | |
| Living donor | 0.63 (0.48–0.83) | 0.001 |
| Transplant era | ||
| 2001–2010 | 1.0 | |
| 2011–2021 | 0.61 (0.47–0.79) | <0.001 |
- Note: Boldface values indicate statistical significance.
- Abbreviations: CI, confidence interval; HR, hazard ratio.
In the multivariate analysis, a significant interaction was found between recipient age and donor age for both patient (p = 0.009) and graft survival (p = 0.012) and between recipient age and donor weight for graft survival (p = 0.017) (Table 8). Among recipients with adult donors, younger recipients had better graft outcomes compared with older recipients 3–10 years of age. This was statistically significant for recipients 1 year of age (HR = 0.75; 95% CI, 0.59–0.96). Among recipients with pediatric donors, younger recipients were associated with worse patient and graft outcomes compared with recipients 3–10 years of age and were statistically significant for recipients <1 year of age. Compared with recipients 3–10 years old, 1-year-old transplant recipients with donors weighing <70 kg had better graft survival (HR = 0.65; 95% CI, 0.46–0.91).
| N | Number of events | 3-Year survival (%) | HR (95% CI) | p | N | Number of events | 3-Year survival (%) | HR (95% CI) | p | Test for interactiona | |
|---|---|---|---|---|---|---|---|---|---|---|---|
| Patient survival | |||||||||||
| Donor age < 18 years (n = 308) | Donor age ≥ 18 years (n = 1860) | ||||||||||
| Recipient age, years | |||||||||||
| 0 | 4 | 2 | 75 ± 21.7 | 33.81 (5.42–211.03) | 0.017 | 28 | 3 | 93 ± 4.9 | 1.42 (0.44–4.63) | 0.80 | 0.009 |
| 1 | 72 | 4 | 97 ± 2.1 | 1.90 (0.42–8.48) | 569 | 33 | 96 ± 0.9 | 0.93 (0.58–1.49) | |||
| 2 | 107 | 8 | 95 ± 2.1 | 2.94 (0.78–11.08) | 608 | 28 | 97 ± 0.7 | 0.84 (0.51–1.37) | |||
| 3–10 | 125 | 3 | 99 ± 1.1 | 1.00 | 655 | 36 | 97 ± 0.7 | 1.00 | |||
| Graft survival | |||||||||||
| Donor age < 18 years (n = 308) | Donor age ≥ 18 years (n = 1860) | ||||||||||
| Recipient age, years | |||||||||||
| 0 | 4 | 3 | 50 ± 25 | 4.06 (1.24–13.30) | 0.27 | 28 | 9 | 89 ± 5.8 | 0.72 (0.37–1.41) | 0.12 | 0.012 |
| 1 | 72 | 23 | 81 ± 4.8 | 1.03 (0.61–1.75) | 569 | 129 | 91 ± 1.2 | 0.75 (0.59–0.96) | |||
| 2 | 107 | 32 | 89 ± 3.0 | 0.97 (0.60–1.56) | 608 | 120 | 94 ± 1.0 | 0.83 (0.65–1.06) | |||
| 3–10 | 125 | 35 | 88 ± 3.1 | 1.00 | 655 | 146 | 93 ± 1.0 | 1.00 | |||
| Donor weight < 70 kg (n = 926) | Donor weight ≥ 70 kg (n = 1196) | ||||||||||
| Recipient age, years | |||||||||||
| 0 | 11 | 4 | 91 ± 8.7 | 0.93 (0.34–2.53) | 0.08 | 18 | 6 | 89 ± 7.4 | 0.81 (0.35–1.86) | 0.87 | 0.017 |
| 1 | 250 | 53 | 90 ± 1.9 | 0.65 (0.46–0.91) | 375 | 91 | 90 ± 1.6 | 0.90 (0.66–1.21) | |||
| 2 | 308 | 65 | 93 ± 1.5 | 0.77 (0.56–1.06) | 393 | 82 | 94 ± 1.3 | 0.97 (0.72–1.32) | |||
| 3–10 | 357 | 93 | 91 ± 1.6 | 1.00 | 419 | 82 | 95 ± 1.2 | 1.00 | |||
- Note: Boldface values indicate statistical significance.
- Abbreviations: CI, confidence interval; HR, hazard ratio.
- a p value testing interaction between recipient age and donor age in a multivariable model.
4 Discussion
To the best of our knowledge, this retrospective study is one of the largest conducted focusing on the smallest subset of the pediatric kidney transplant cohort. The results are in congruence with other publications in noting excellent outcomes despite the complexities posed in transplanting such small infants, such as underlying urologic anomalies, donor-recipient size mismatch, nutrition, neurologic, and metabolic comorbidities. Modern era 3-year graft and patient survival were 94% and 98%, respectively [9, 12, 14]. A combination of factors is culprit, including advances in surgical technique, immunosuppressive regiments, as well as optimized posttransplant monitoring.
Several other findings corroborate previously published studies. These include improved graft survival in male vs. female patients [27-29]. Although the exact mechanism remains unknown, we suspect differences in immune physiology, drug metabolism, anatomical considerations, and transplant indication to be responsible (Table 9). We also confirmed diminished graft survival among non-White patients [9, 10, 12, 17]. Disparity in access to health care is thought to play critical roles here, and further prospective investigations are required. Prior studies have shown delayed access to transplant listing, higher mortality while on dialysis, as well as delayed transplantation in minority pediatric patients [30, 31]. After implantation of Share 35, the probability of transplantation increased in minorities; however, longer wait times to transplantation persist when compared to White patients [32]. Likewise, LDKT was associated with superior graft survival, as reported elsewhere [9, 10, 13, 18].
| Transplant indication | Males (n = 1450) | Females (n = 708) | ||
|---|---|---|---|---|
| n | 3 Year graft survival ± SE (%) | n | 3 Year graft survival ± SE (%) | |
| Hypoplasia/dysplasia | 390 | 93 ± 1.4 | 222 | 87 ± 2.3 |
| Hypoperfusion injury | 65 | 95 ± 2.9 | 65 | 89 ± 3.9 |
| Reflux nephropathy | 639 | 92 ± 1.1 | 73 | 92 ± 3.3 |
| Glomerulonephritis | 38 | 88 ± 5.5 | 43 | 88 ± 5.1 |
| Cystic/tubular kidney disease | 110 | 92 ± 2.8 | 77 | 89 ± 3.7 |
| Nephrotic syndrome | 130 | 93 ± 2.4 | 146 | 96 ± 1.7 |
| Other | 78 | 93 ± 3.0 | 82 | 93 ± 3.0 |
- Abbreviation: SE, standard error.
With regard to the indication for transplantation, the two most common entities were renal hypoplasia/dysplasia (28.4%) and reflux nephropathy (33%), with nephrotic syndrome being the second most common indication in females. Nephrotic syndrome was correlated with better graft survival than hypoplasia/dysplasia. Classically, patients with nephrotic syndrome, including FSGS, have a worse prognosis [16]. One explanation is the increased likelihood of genetic etiology of nephrotic syndrome in very young children, whereby recurrence is extremely rare [33, 34]. Among all other indications, there were no significant variances by etiology.
Critically, the recipient dialysis status was the sole significant variable influencing both graft and patient survival in multivariate analysis. This too has been well documented in prior studies [10-13]. Amaral et al. [10] demonstrated a 52% higher risk of graft failure in children with more than 1 year and 89% higher risk in those with greater than 18 months of dialysis at the time of transplantation.
In an interesting trend, 1-year-old patients had better graft survival compared with 3 to10-year-old patients. This result validates findings from the 2018 North American Pediatric Renal Trials and Collaborative Studies (NAPRTCS) report, which illustrated a trend toward lower HRs for graft loss among <24-month transplant recipients, in a similar era [35]. Although we cannot conclusively delineate the reasons herein, contributing factors are apt to include an increased proportion of LDKT, diminished times on dialysis, and an increase percentage of White male patients [10-13]. These factors are thought to select for advanced disease burden and immunogenicity at the time of transplant in the older patients. Furthermore, given our study design, the morbidity burden of children meeting the inclusion criteria of ≤15 kg is likely to increase with age. This conclusion is contrary to earlier reports observing better outcomes in older patients [10, 14, 16].
Integrated, the data support the notion of a “Goldilocks zone” for many children to undergo kidney transplantation at around 1–2 years of age, ideally in a preemptive fashion and prior to establishment of the long-lasting sequelae of dialysis. Nevertheless, and despite the clear advantages of early transplantation, most patients are not preemptively transplanted. 74.8% of patients were already on dialysis at the time of transplant, with 65.3% of those on dialysis for longer than 1 year. Only 31% were transplanted at ≤1 years of age and 30% at ≤10 kg. This underlines a long-standing trend of awaiting transplantation until children are older and have attained a minimum weight threshold, the exact criteria for which is nebulous and generally center-driven. Though historical outcomes tend to support these policies, more recent data show that pediatric kidney transplantation can be successful in even the smallest infants [36]. One key hurdle is appropriating size matched grafts and recipients. Historically, and as also presented here, this combination is thought to impose worse graft and patient outcomes. Others have found equivalent outcomes when matching young donor kidneys and pediatric recipients [37]. In the meantime, advances in surgical acumen enable adult to low weight pediatric transplantation with excellent results [8].
This study was performed in a retrospective manner with the aid of a registry, serving as both a strength and constraint. Thus, although limited by design, it helps further highlight certain key concepts in pediatric transplantation. This operation can be performed in the youngest and most complicated patients with excellent outcomes. There should be an urgency placed on preemptive transplantation even in the smallest individuals that otherwise qualify for the operation, without delay to meet arbitrary thresholds. To do so, heightened surgical techniques need to be applied to broaden the consumption of both size matched and mismatched organs from adult and pediatric donors alike, and living donation remains the gold standard when available. Finally, better equity for access to and care of transplants needs to be established among diverse racial populations and gender distributions.
Author Contributions
K.E., R.L., and L.S. were involved in the conception or design of the work. M.L. and L.S. contributed to data acquisition. K.E., Y.K., R.L., L.S., M.L., R.M., and J.E. contributed to the analysis and interpretation of data. K.E., R.M., Y.K., M.L., N.K., L.S., and S.Z. drafted the article. All authors critically revised the article and approved the version to be published.
Conflicts of Interest
The authors declare no conflicts of interest.
Open Research
Data Availability Statement
The data that support the findings of this study are available on request from the corresponding author. The data are not publicly available due to privacy or ethical restrictions.