Liver transplant for primary biliary tract neuroendocrine tumor in a nine-year-old girl
Corresponding Author
Anjali Rai
Division of Pediatric Gastroenterology, Hepatology and Nutrition, Department of Pediatrics, Johns Hopkins University School of Medicine, Baltimore, Maryland, USA
Correspondence
Anjali Rai, Division of Pediatric Gastroenterology, Hepatology and Nutrition, Johns Hopkins Children's Center, 1800 Orleans Street, Baltimore, MD 21287, USA.
Email: [email protected]
Kathryn Lemberg, Division of Pediatric Oncology, Sidney Kimmel Comprehensive Cancer Center, 1650 Orleans Street, Baltimore, MD 21231, USA.
Email: [email protected]
Search for more papers by this authorLauren Sproule
Department of Oncology, Johns Hopkins University School of Medicine, Baltimore, Maryland, USA
Department of Biochemistry, McGill University, Montreal, Canada
Search for more papers by this authorTatianna Larman
Department of Pathology, Johns Hopkins University School of Medicine, Baltimore, Maryland, USA
Search for more papers by this authorKiyoko Oshima
Department of Pathology, Johns Hopkins University School of Medicine, Baltimore, Maryland, USA
Search for more papers by this authorDaniel Rhee
Division of General Pediatric Surgery, Department of Surgery, Johns Hopkins University School of Medicine, Baltimore, Maryland, USA
Search for more papers by this authorKenneth Ng
Division of Pediatric Gastroenterology, Hepatology and Nutrition, Department of Pediatrics, Johns Hopkins University School of Medicine, Baltimore, Maryland, USA
Search for more papers by this authorElizabeth King
Division of Transplant Surgery, Department of Surgery, Johns Hopkins University School of Medicine, Baltimore, Maryland, USA
Search for more papers by this authorDouglas Mogul
Division of Pediatric Gastroenterology, Hepatology and Nutrition, Department of Pediatrics, Johns Hopkins University School of Medicine, Baltimore, Maryland, USA
Search for more papers by this authorCorresponding Author
Kathryn Lemberg
Department of Oncology, Johns Hopkins University School of Medicine, Baltimore, Maryland, USA
Correspondence
Anjali Rai, Division of Pediatric Gastroenterology, Hepatology and Nutrition, Johns Hopkins Children's Center, 1800 Orleans Street, Baltimore, MD 21287, USA.
Email: [email protected]
Kathryn Lemberg, Division of Pediatric Oncology, Sidney Kimmel Comprehensive Cancer Center, 1650 Orleans Street, Baltimore, MD 21231, USA.
Email: [email protected]
Search for more papers by this authorCorresponding Author
Anjali Rai
Division of Pediatric Gastroenterology, Hepatology and Nutrition, Department of Pediatrics, Johns Hopkins University School of Medicine, Baltimore, Maryland, USA
Correspondence
Anjali Rai, Division of Pediatric Gastroenterology, Hepatology and Nutrition, Johns Hopkins Children's Center, 1800 Orleans Street, Baltimore, MD 21287, USA.
Email: [email protected]
Kathryn Lemberg, Division of Pediatric Oncology, Sidney Kimmel Comprehensive Cancer Center, 1650 Orleans Street, Baltimore, MD 21231, USA.
Email: [email protected]
Search for more papers by this authorLauren Sproule
Department of Oncology, Johns Hopkins University School of Medicine, Baltimore, Maryland, USA
Department of Biochemistry, McGill University, Montreal, Canada
Search for more papers by this authorTatianna Larman
Department of Pathology, Johns Hopkins University School of Medicine, Baltimore, Maryland, USA
Search for more papers by this authorKiyoko Oshima
Department of Pathology, Johns Hopkins University School of Medicine, Baltimore, Maryland, USA
Search for more papers by this authorDaniel Rhee
Division of General Pediatric Surgery, Department of Surgery, Johns Hopkins University School of Medicine, Baltimore, Maryland, USA
Search for more papers by this authorKenneth Ng
Division of Pediatric Gastroenterology, Hepatology and Nutrition, Department of Pediatrics, Johns Hopkins University School of Medicine, Baltimore, Maryland, USA
Search for more papers by this authorElizabeth King
Division of Transplant Surgery, Department of Surgery, Johns Hopkins University School of Medicine, Baltimore, Maryland, USA
Search for more papers by this authorDouglas Mogul
Division of Pediatric Gastroenterology, Hepatology and Nutrition, Department of Pediatrics, Johns Hopkins University School of Medicine, Baltimore, Maryland, USA
Search for more papers by this authorCorresponding Author
Kathryn Lemberg
Department of Oncology, Johns Hopkins University School of Medicine, Baltimore, Maryland, USA
Correspondence
Anjali Rai, Division of Pediatric Gastroenterology, Hepatology and Nutrition, Johns Hopkins Children's Center, 1800 Orleans Street, Baltimore, MD 21287, USA.
Email: [email protected]
Kathryn Lemberg, Division of Pediatric Oncology, Sidney Kimmel Comprehensive Cancer Center, 1650 Orleans Street, Baltimore, MD 21231, USA.
Email: [email protected]
Search for more papers by this authorAbstract
Background
Neuroendocrine tumors (NETs) are rare epithelial neoplasms that arise most commonly from the gastrointestinal tract. In pediatrics, the most common site of origin is in the appendix, with the liver being the most common site of metastasis. Neuroendocrine tumors arising from the biliary tract are extremely rare.
Methods
We describe a case of a nine-year-old girl who presented with obstructive cholestasis and was found to have multiple liver masses identified on biopsy as well-differentiated neuroendocrine tumor with an unknown primary tumor site.
Result
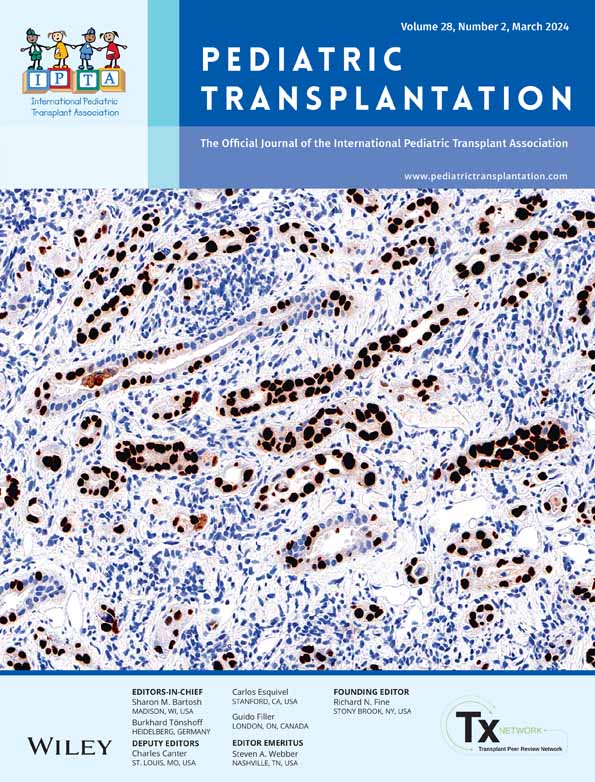
The patient underwent extensive investigation to identify a primary tumor site, including endoscopy, endoscopic ultrasound, and capsule endoscopy. The patient ultimately underwent definitive management with liver transplant, and on explant was discovered to have multiple well-differentiated neuroendocrine tumors, WHO Grade 1, with extensive infiltration into the submucosa of bile duct, consistent with primary biliary tract neuroendocrine tumor.
Conclusion
Identifying the site of the primary tumor in NETs found within the liver can be challenging. To determine if an extrahepatic primary tumor exists, workup should include endoscopy, EUS, and capsule endoscopy. Children with well-differentiated hepatic NETs, with no identifiable primary tumor, and an unresectable tumor, are considered favorable candidates for liver transplantation.
Open Research
DATA AVAILABILITY STATEMENT
The data that support the findings of this study are available on request from the corresponding author. The data are not publicly available due to privacy or ethical restrictions.
REFERENCES
- 1Johnson PR. Gastroenteropancreatic neuroendocrine (carcinoid) tumors in children. Semin Pediatr Surg. 2014; 23(2): 91-95. doi:10.1053/j.sempedsurg.2014.03.007
- 2Oberg K, Knigge U, Kwekkeboom D, Perren A, Group EGW. Neuroendocrine gastro-entero-pancreatic tumors: ESMO clinical practice guidelines for diagnosis, treatment and follow-up. Ann Oncol. 2012; 23(Suppl 7): vii124-30. doi:10.1093/annonc/mds295
- 3Allan B, Davis J, Perez E, Lew J, Sola J. Malignant neuroendocrine tumors: incidence and outcomes in pediatric patients. Eur J Pediatr Surg. 2013; 23(5): 394-399. doi:10.1055/s-0033-1333643
- 4Diets IJ, Nagtegaal ID, Loeffen J, et al. Childhood neuroendocrine tumours: a descriptive study revealing clues for genetic predisposition. Br J Cancer. 2017; 116(2): 163-168. doi:10.1038/bjc.2016.408
- 5Farooqui ZA, Chauhan A. Neuroendocrine tumors in pediatrics. Glob Pediatr Health. 2019; 6: 2333794X19862712. doi:10.1177/2333794X19862712
- 6Tran CG, Sherman SK, Chandrasekharan C, Howe JR. Surgical Management of Neuroendocrine Tumor Liver Metastases. Surg Oncol Clin N Am. 2021; 30(1): 39-55. doi:10.1016/j.soc.2020.08.001
- 7Gedaly R, Daily MF, Davenport D, et al. Liver transplantation for the treatment of liver metastases from neuroendocrine tumors: an analysis of the UNOS database. Arch Surg. 2011; 146(8): 953-958. doi:10.1001/archsurg.2011.186
- 8Chatziioannou A, Georgopoulou V, Katsiki E, Sinakos E. Primary hepatic neuroendocrine tumor treated with liver transplantation. Dig Liver Dis. 2022; 54(10): 1441-1443. doi:10.1016/j.dld.2022.01.133
- 9Hong SM, Cho H, Moskaluk CA, Frierson HF Jr, Yu E, Ro JY. CDX2 and MUC2 protein expression in extrahepatic bile duct carcinoma. Am J Clin Pathol. 2005; 124(3): 361-370. doi:10.1309/GTU1-Y77M-VR4D-X5A2
- 10Fernandez KS, Aldrink JH, Ranalli M, Ruymann FB, Caniano DA. Carcinoid tumors in children and adolescents: risk for second malignancies. J Pediatr Hematol Oncol. 2015; 37(2): 150-153. doi:10.1097/MPH.0000000000000280
- 11Boston CH, Phan A, Munsell MF, Herzog CE, Huh WW. A comparison between Appendiceal and Nonappendiceal neuroendocrine tumors in children and young adults: a single-institution experience. J Pediatr Hematol Oncol. 2015; 37(6): 438-442. doi:10.1097/MPH.0000000000000350
- 12Navalkele P, O'Dorisio MS, O'Dorisio TM, Zamba GK, Lynch CF. Incidence, survival, and prevalence of neuroendocrine tumors versus neuroblastoma in children and young adults: nine standard SEER registries, 1975-2006. Pediatr Blood Cancer. 2011; 56(1): 50-57. doi:10.1002/pbc.22559
- 13Dasari A, Shen C, Halperin D, et al. Trends in the incidence, prevalence, and survival outcomes in patients with neuroendocrine tumors in the United States. JAMA Oncol. 2017; 3(10): 1335-1342. doi:10.1001/jamaoncol.2017.0589
- 14Tonnhofer U, Balassy C, Reck CA, Koller A, Horcher E. Neuroendocrine tumor of the common hepatic duct, mimicking a choledochal cyst in a 6-year-old child. J Pediatr Surg. 2009; 44(6): E23-E25. doi:10.1016/j.jpedsurg.2009.03.030
- 15Broaddus RR, Herzog CE, Hicks MJ. Neuroendocrine tumors (carcinoid and neuroendocrine carcinoma) presenting at extra-appendiceal sites in childhood and adolescence. Arch Pathol Lab Med. 2003; 127(9): 1200-1203. doi:10.5858/2003-127-1200-NTCANC
- 16 National Comprehensive Cancer Network. Neuroendocrine and Adrenal Tumors (Version 2.2018). Accessed March 26, 2020 http://www.nccn.org/professionals/physician_gls/pdf/bone.pdf
- 17Oberg K, Kvols L, Caplin M, et al. Consensus report on the use of somatostatin analogs for the management of neuroendocrine tumors of the gastroenteropancreatic system. Ann Oncol. 2004; 15(6): 966-973. doi:10.1093/annonc/mdh216
- 18Rinke A, Muller HH, Schade-Brittinger C, et al. Placebo-controlled, double-blind, prospective, randomized study on the effect of octreotide LAR in the control of tumor growth in patients with metastatic neuroendocrine midgut tumors: a report from the PROMID study group. J Clin Oncol. 2009; 27(28): 4656-4663. doi:10.1200/JCO.2009.22.8510
- 19Singh S, Carnaghi C, Buzzoni R, et al. Everolimus in neuroendocrine tumors of the gastrointestinal tract and unknown primary. Neuroendocrinology. 2018; 106(3): 211-220. doi:10.1159/000477585
- 20Fine RL, Gulati AP, Krantz BA, et al. Capecitabine and temozolomide (CAPTEM) for metastatic, well-differentiated neuroendocrine cancers: the pancreas Center at Columbia University experience. Cancer Chemother Pharmacol. 2013; 71(3): 663-670. doi:10.1007/s00280-012-2055-z
- 21Chauhan A, Farooqui Z, Murray LA, et al. Capecitabine and Temozolomide in neuroendocrine tumor of unknown primary. J Oncol. 2018; 2018:3519247. doi:10.1155/2018/3519247
- 22Strosberg J, El-Haddad G, Wolin E, et al. Phase 3 trial of (177)Lu-Dotatate for Midgut neuroendocrine tumors. N Engl J Med. 2017; 376(2): 125-135. doi:10.1056/NEJMoa1607427
- 23Foster JH, Sher A, Seghers V, et al. Peptide receptor radionuclide therapy for treatment of metastatic neuroendocrine tumors in children. Pediatr Blood Cancer. 2021; 68(7):e29056. doi:10.1002/pbc.29056
- 24Pavel ME, Hainsworth JD, Baudin E, et al. Everolimus plus octreotide long-acting repeatable for the treatment of advanced neuroendocrine tumours associated with carcinoid syndrome (RADIANT-2): a randomised, placebo-controlled, phase 3 study. Lancet. 2011; 378(9808): 2005-2012. doi:10.1016/S0140-6736(11)61742-X
- 25Le Treut YP, Gregoire E, Klempnauer J, et al. Liver transplantation for neuroendocrine tumors in Europe-results and trends in patient selection: a 213-case European liver transplant registry study. Ann Surg. 2013; 257(5): 807-815. doi:10.1097/SLA.0b013e31828ee17c
- 26Yao JC, Hassan M, Phan A, et al. One hundred years after "carcinoid": epidemiology of and prognostic factors for neuroendocrine tumors in 35,825 cases in the United States. J Clin Oncol. 2008; 26(18): 3063-3072. doi:10.1200/JCO.2007.15.4377
- 27Kim J, Zimmerman MA, Hong JC. Liver transplantation in the treatment of unresectable hepatic metastasis from neuroendocrine tumors. J Gastrointest Oncol. 2020; 11(3): 601-608. doi:10.21037/jgo.2019.11.03
- 28Mazzaferro V, Pulvirenti A, Coppa J. Neuroendocrine tumors metastatic to the liver: how to select patients for liver transplantation? J Hepatol. 2007; 47(4): 460-466. doi:10.1016/j.jhep.2007.07.004
- 29Kwong AJ, Kim WR, Lake JR, et al. OPTN/SRTR 2019 annual data report: liver. Am J Transplant. 2021; 21(Suppl 2): 208-315. doi:10.1111/ajt.16494
- 30Laurence JM, Sapisochin G, DeAngelis M, et al. Biliary complications in pediatric liver transplantation: incidence and management over a decade. Liver Transpl. 2015; 21(8): 1082-1090. doi:10.1002/lt.24180