Brain tuberculoma in pediatric heart transplant recipient
Abstract
Introduction
Heart transplantation is the standard treatment for end-stage heart disease. Despite advances in the field, patients remain under risk of developing complications, including opportunistic infections, such as tuberculosis. We present the unprecedented case of cerebral tuberculoma in a 9-year-old heart transplant recipient.
Case Scenario
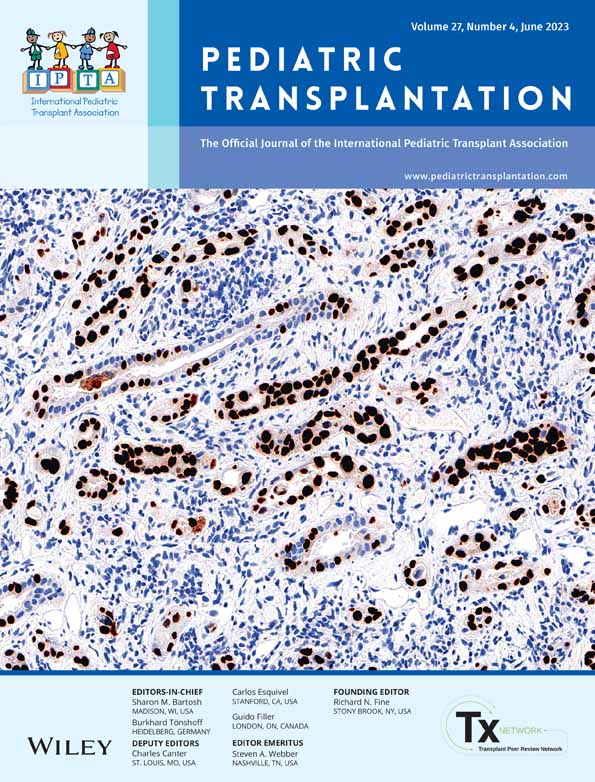
A 9-year-old female child, who underwent heart transplantation in December 2020, was admitted to the emergency department in September 2021 due to headache and vomiting. She had normal vital signs and a mild left hemiparesis. Laboratory findings included lymphopenia and a low C Reactive Protein and brain images showed expansive lesions. A biopsy of the intracranial lesion was performed and anatomopathological analysis was compatible with tuberculoma. After the diagnosis was established, treatment protocol for neurotuberculosis was initiated, the patient had a satisfactory clinical evolution and was discharged 22 days after admission.
Discussion
Clinical manifestation of tuberculosis usually occurs up to 6 months after transplantation, the findings are commonly atypical and symptoms may be mild. We could not find in medical literature any description of the disease in a heart transplant recipient as young as the one presented in this case report. We documented great response to treatment, even though conventional antituberculosis therapy may interfere with immunosuppression.
Conclusion
Patients in the postoperative period following heart transplantation are at high risk for developing opportunistic infections such as tuberculosis, which may present with atypical symptoms. Therefore the clinician must have a high index of suspicion in order to make the correct diagnosis and promptly start treatment.
CONFLICT OF INTEREST STATEMENT
The authors have no conflicts of interest to declare. All co-authors have seen and agree with the contents of the manuscript and there is no financial interest to report. We certify that the submission is original work and is not under review at any other publication.
Open Research
DATA AVAILABILITY STATEMENT
Data sharing is not applicable to this article as no new data were created or analyzed in this study.