Hepatocellular carcinoma requiring liver transplantation in hereditary tyrosinemia type 1 despite nitisinone therapy and α1-fetoprotein normalization
Abstract
Background
Hereditary tyrosinemia type 1 is a rare metabolic condition associated with an increased risk of hepatocellular carcinoma. Nitisinone (2-[2-nitro-4-trifluoromethylbenzoyl]-1,3-cyclohexanedione, NTBC) treatment has reduced but not eliminated the risk. The delayed initiation of nitisinone treatment, and persistently abnormal α1-fetoprotein (AFP) levels are recognized to be risk factors for late-onset hepatocellular carcinoma. We report three children diagnosed and treated with nitisinone since infancy who developed hepatocellular carcinoma despite long-term normalization of AFP.
Methods
A retrospective review of all patients with tyrosinemia on nitisinone managed at our center was undertaken. Patient demographics, age at diagnosis, duration of therapy, timing of AFP normalization, and radiographic imaging findings were noted.
Results
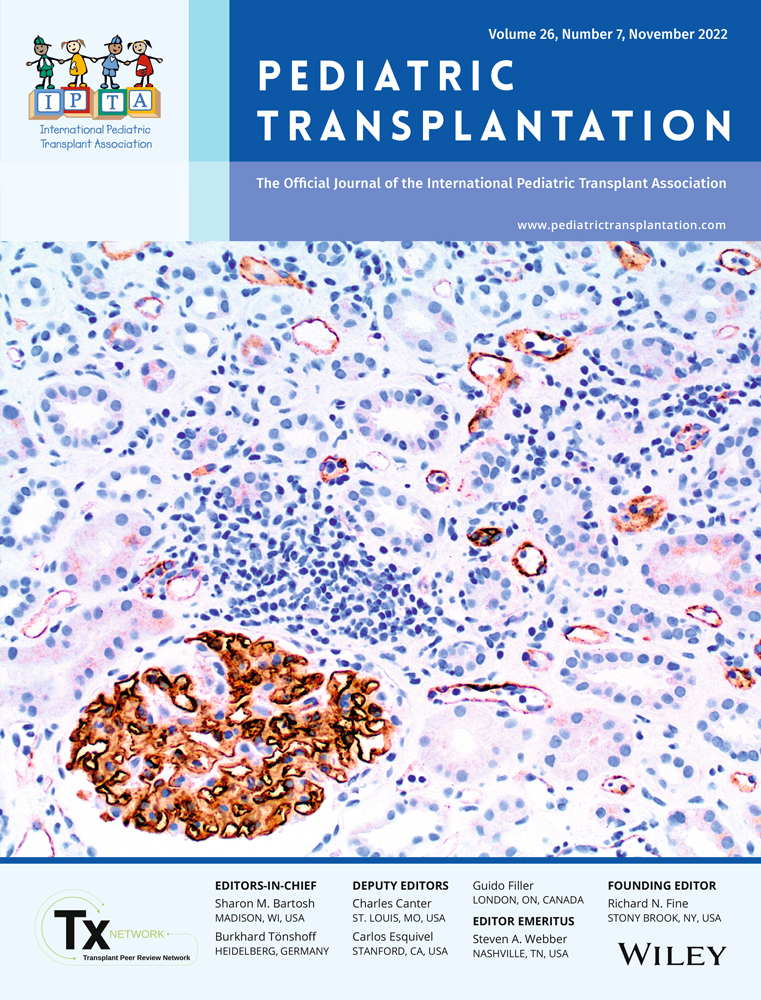
Three patients at our center with tyrosinemia type 1 developed hepatocellular carcinoma 9–13 years after diagnosis despite long-term nitisinone therapy and normalization of AFP. Two patients developed new nodules on imaging with an elevation of AFP leading to the diagnosis and subsequent liver transplant. The third patient proceeded with liver transplant because of a very nodular liver and increasing splenomegaly despite normal AFP and no change in surveillance gadoxetate magnetic resonance imaging. Early hepatocellular carcinoma was found in her liver explant. All three patients were cirrhotic at diagnosis.
Conclusions
Patients with hereditary tyrosinemia type 1, especially those already cirrhotic at diagnosis, remain at high risk of developing hepatocellular carcinoma despite long-term nitisinone therapy and AFP normalization, and warrant close monitoring and surveillance.
CONFLICT OF INTEREST
The authors do not have any conflicts of interest to declare.
Open Research
DATA AVAILABILITY STATEMENT
The data that support the findings of this study are available from the corresponding author upon reasonable request.