Review of the impact of donor characteristics on pediatric heart transplant outcomes
Correction(s) for this article
-
Erratum
- Volume 25Issue 7Pediatric Transplantation
- First Published online: July 3, 2021
Corresponding Author
Jennifer Conway
Division of Pediatric Cardiology, Department of Pediatrics, Stollery Children’s Hospital, University of Alberta, Edmonton, AB, Canada
Correspondence
Jennifer Conway, 8440 112 Street, WMC 4C2, Edmonton, AB T6G2B7, Canada.
Email: [email protected]
Search for more papers by this authorJean A. Ballweg
Division of Pediatric Cardiology, Department of Pediatrics, Children’s Hospital and Medical Center, University of Nebraska Medical Center, Omaha, Nebraska
Search for more papers by this authorMatthew Fenton
Great Ormond Street Hospital for Children Foundation Trust, London, UK
Search for more papers by this authorSteve Kindel
Division of Pediatric Cardiology, Department of Pediatrics, Medical College of Wisconsin and Herma Heart Institute and Children's Hospital of Wisconsin, Milwaukee, Wisconsin
Search for more papers by this authorMaryanne Chrisant
The Heart Institute, Joe Dimaggio Children’s Hospital, Hollywood, Florida
Search for more papers by this authorRobert G. Weintraub
Department of Paediatrics, The University of Melbourne, Melbourne, Vic, Australia
Department of Cardiology, The Royal Children's Hospital, Melbourne Heart Research Group, Murdoch Children’s Research Institute, Melbourne, Vic, Australia
Search for more papers by this authorLara Danziger-Isakov
Pediatric Infectious Diseases, Cincinnati Children's Hospital Medical Center & University of Cincinnati, Cincinnati, Ohio
Search for more papers by this authorRichard Kirk
Division of Pediatric Cardiology, University of Texas Southwestern Medical Center, Children's Medical Center, Dallas, Texas
Search for more papers by this authorOliver Miera
Department of Congenital Heart Disease/Pediatric Cardiology, Berlin, Germany
Search for more papers by this authorRyan R. Davies
Department of Cardiovascular and Thoracic Surgery, University of Texas Southwestern Medical Center, Children's Medical Center, Dallas, Texas
Search for more papers by this authorAnne I. Dipchand
Labatt Family Heart Centre, Hospital for Sick Children, University of Toronto, Toronto, ON, Canada
Search for more papers by this authorCorresponding Author
Jennifer Conway
Division of Pediatric Cardiology, Department of Pediatrics, Stollery Children’s Hospital, University of Alberta, Edmonton, AB, Canada
Correspondence
Jennifer Conway, 8440 112 Street, WMC 4C2, Edmonton, AB T6G2B7, Canada.
Email: [email protected]
Search for more papers by this authorJean A. Ballweg
Division of Pediatric Cardiology, Department of Pediatrics, Children’s Hospital and Medical Center, University of Nebraska Medical Center, Omaha, Nebraska
Search for more papers by this authorMatthew Fenton
Great Ormond Street Hospital for Children Foundation Trust, London, UK
Search for more papers by this authorSteve Kindel
Division of Pediatric Cardiology, Department of Pediatrics, Medical College of Wisconsin and Herma Heart Institute and Children's Hospital of Wisconsin, Milwaukee, Wisconsin
Search for more papers by this authorMaryanne Chrisant
The Heart Institute, Joe Dimaggio Children’s Hospital, Hollywood, Florida
Search for more papers by this authorRobert G. Weintraub
Department of Paediatrics, The University of Melbourne, Melbourne, Vic, Australia
Department of Cardiology, The Royal Children's Hospital, Melbourne Heart Research Group, Murdoch Children’s Research Institute, Melbourne, Vic, Australia
Search for more papers by this authorLara Danziger-Isakov
Pediatric Infectious Diseases, Cincinnati Children's Hospital Medical Center & University of Cincinnati, Cincinnati, Ohio
Search for more papers by this authorRichard Kirk
Division of Pediatric Cardiology, University of Texas Southwestern Medical Center, Children's Medical Center, Dallas, Texas
Search for more papers by this authorOliver Miera
Department of Congenital Heart Disease/Pediatric Cardiology, Berlin, Germany
Search for more papers by this authorRyan R. Davies
Department of Cardiovascular and Thoracic Surgery, University of Texas Southwestern Medical Center, Children's Medical Center, Dallas, Texas
Search for more papers by this authorAnne I. Dipchand
Labatt Family Heart Centre, Hospital for Sick Children, University of Toronto, Toronto, ON, Canada
Search for more papers by this author[Correction added on June 28, 2021 after first online publication: the name of the ninth author was changed from “Oliver Meira” to “Oliver Miera”.]
Abstract
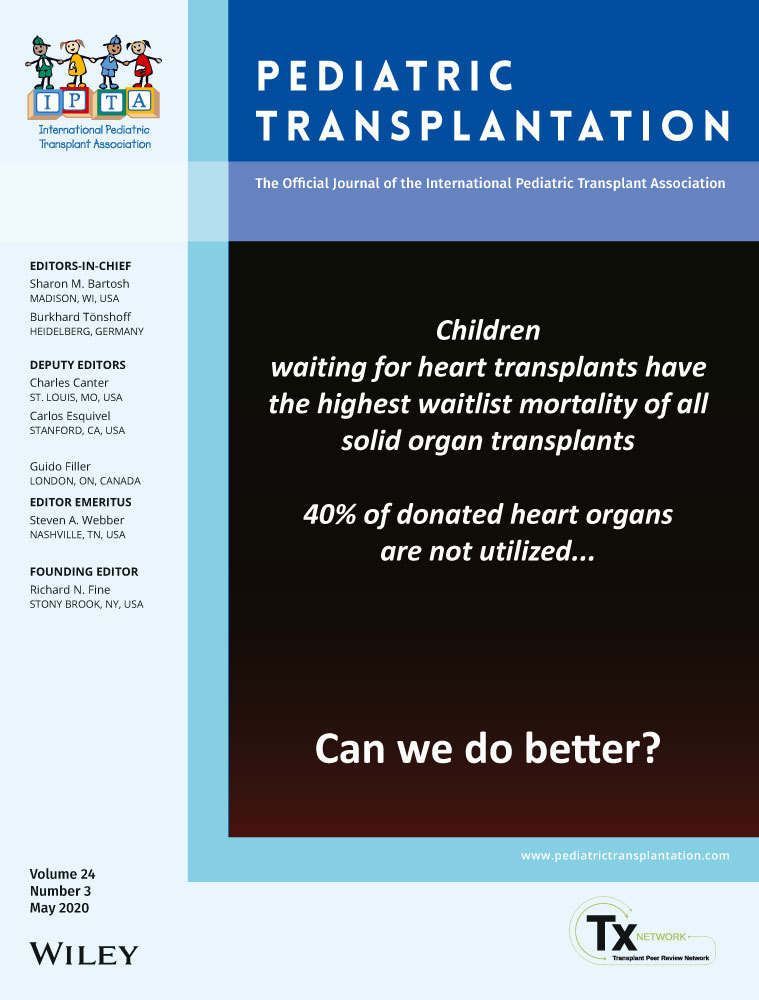
Heart transplantation (HTx) is a treatment option for end-stage heart failure in children. HTx is limited by the availability and acceptability of donor hearts. Refusal of donor hearts has been reported to be common with reasons for refusal including preexisting donor characteristics. This review will focus on the impact of donor characteristics and comorbidities on outcomes following pediatric HTx. A literature review was performed to identify articles on donor characteristics and comorbidities and pediatric HTx outcomes. There are many donor characteristics to consider when accepting a donor heart. Weight-based matching is the most common form of matching in pediatric HTx with a donor-recipient weight ratio between 0.7 and 3 having limited impact on outcomes. From an age perspective, donors <50 years can be carefully considered, but the impact of ischemic time needs to be understood. To increase the donor pool, with minimal impact on outcomes, ABO-incompatible donors should be considered in patients that are eligible. Other factors to be considered when accepting an organ is donor comorbidities. Little is known about donor comorbidities in pediatric HTx, with most of the data available focusing on infections. Being aware of the potential infections in the donor, understanding the testing available and risks of transmission, and treatment options for the recipient is essential. There are a number of donor characteristics that potentially impact outcomes following pediatric HTx, but these need to be taken into consideration along with their interactions with recipient factors when interpreting the outcomes following HTx.
REFERENCES
- 1Rizwan R, Zafar F, Bryant R, et al. The number of refusals for donor organ quality does not impact heart transplant outcomes in children. Ann Thorac Surg. 2018; 105(4): 1223-1230. https://doi.org/10.1016/j.athoracsur.2017.10.006
- 2Zafar F, Rizwan R, Lorts A, Bryant R 3rd, Tweddell JS, Chin CMD. Implications and outcomes of cardiac grafts refused by pediatric centers but transplanted by adult centers. J Thorac Cardiovasc Surg. 2017; 154(2): 528-536.
- 3Costanzo MR, Dipchand A, Starling R, et al. The international society of heart and lung transplantation guidelines for the care of heart transplant recipients. J Hear Lung Transplant. 2010; 29(8): 914-956. https://doi.org/10.1016/j.healun.2010.05.034
- 4Kanani M, Hoskote A, Carter C, Burch M, Tsang V, Kostolny M. Increasing donor-recipient weight mismatch in pediatric orthotopic heart transplantation does not adversely affect outcome. Eur J Cardio-thoracic Surg. 2012; 41(2): 427-434. https://doi.org/10.1016/j.ejcts.2011.04.042
- 5Tang L, Du W, Delius RE, L’Ecuyer TJ, Zilberman MV. Low donor-to-recipient weight ratio does not negatively impact survival of pediatric heart transplant patients. Pediatr Transpl. 2010; 14(6): 741-745. https://doi.org/10.1111/j.1399-3046.2010.01300.x
- 6Delmo Walter EM, Huebler M, Schubert S, et al. Influence of size disparity of transplanted hearts on cardiac growth in infants and children. J Thorac Cardiovasc Surg. 2012; 143(1): 168-177. https://doi.org/10.1016/j.jtcvs.2011.09.041
- 7Taghavi S, Jayarajan SN, Wilson LM, Komaroff E, Testani JMMA. Cardiac transplantation can be safely performed using selected diabetic donors. J Thorac Cardiovasc Surg 2014; 146(2): 1-12. https://doi.org/10.1016/j.jtcvs.2013.02.047.Cardiac
- 8Menting AT, de Castro BO, Wijngaards-de Meij LDNV, Matthys W. A trial of parent training for mothers being released from incarceration and their children. J Clin Child Adolesc. 2014; 43(3): 381-396.
- 9Zafar F, Khan MS, Bryant R, Castleberry CD, Chin CMD. Does oversizing the donors have any benefit for Pediatric Heart Transplant recipients with elevated pulmonary vascular resistance? J Hear Lung Transplant. 2015; 34(1): S36.
- 10Patel A, Bock MJ, Wollstein A, Nguyen K, Malerba S, Lytrivi ID. Donor-recipient height ratio and outcomes in pediatric heart transplantation. Pediatr Transplant. 2016; 20(5): 652-657.
- 11Hahn E, Zucherman WA, Chen JM, Singh RK, Addonizio LJRM. An echocardiographic measurement of superior vena cava to inferior vena cava distance in patients <20 years of age with idiopathic dilated cardiomyopathy. Am J Cardiol. 2014; 113(8): 1405-1408.
- 12Zucherman WA, Richmond ME, Singh RK, Chen JMAL. Use of height and a novel echocardiographic measurement to improve size-matching for pediatric heart transplantation. J Heart Lung Transplant. 2012; 31(8): 896-902.
- 13Gong TA, Joseph SM, Lima B, et al. Donor predicted heart mass as predictor of primary graft dysfunction. J Hear Lung Transplant. 2018; 37(7): 826-835.
- 14Sabatino M, Vitale G, Masetti M, et al. Donor-recipient size mismatch and risk of early graft dysfunction in patients with pulmonary hypertension: potential role of matching based on predicted heart mass. In Transplant International. Hoboken, NJ: Wiley-Blackwell; 2016; 29: 13-13.
- 15Szugye NA, Lorts A, Zafar F, Taylor M, Morales DLSMR. Can virtual heart transplantation via 3D imaging increase the maximum acceptable donor size? J Hear Lung Transplant. 2018; 38: 331-333.
- 16Plasencia JD, Kamarianakis Y, Ryan JR, et al. Alternative methods for virtual heart transplant-Size matching for pediatric heart transplantation with and without donor medical images available. Pediatr Transpl. 2018; 22(8):e13290. https://doi.org/10.1111/petr.13290
- 17Rossano JW, Cherikh WS, Chambers DC, et al. The Registry of the International Society for Heart and Lung Transplantation: Twentieth Pediatric Heart Transplantation Report — 2017; focus theme : allograft ischemic time. J Hear Lung Transplant. 2017; 36(10): 1060-1069. https://doi.org/10.1016/j.healun.2017.07.018
- 18Reich HJ, Kobashigawa JA, Aintablian T, Ramzy D, Kittleson MMEF. Effects of older donor age and cold ischemic time on long-term outcomes of heart transplantation. Texas Hear Inst J. 2018; 45(1): 17-22.
- 19Westbrook TC, Morales DLS, Khan MS, et al. Interaction of older donor age and survival after weight-matched pediatric heart transplantation. J Hear Lung Transplant. 2017; 36(5): 554-558. https://doi.org/10.1016/j.healun.2016.11.009
- 20Weber DJ, Wang I-W, Gracon ASA, et al. Impact of donor age on survival after heart transplantation: an analysis of the United Network for Organ Sharing (UNOS) registry. J Card Surg United States. 2014; 29(5): 723-728.
- 21Eskandary FA, Kohl M, Dunkler D, et al. Lack of donor and recipient age interaction in cardiac transplantation. J Hear Lung Transplant. 2014; 33(6): 629-635.
- 22Bruschi G, Colombo T, Oliva F, et al. Orthotopic heart transplantation with donors greater than or equal to 60 years of age: a single-center experience. Eur J Cardiothorac Surg Ger. 2011; 40(1): e55-e61. https://doi.org/10.1016/j.ejcts.2011.02.013
- 23West LJ, Pollock-Barziv SM, Dipchand AI, et al. ABO-incompatible heart transplantation in infants. N Engl J Med. 2001; 344: 793-800.
- 24Foreman C, Gruenwald C, West L. ABO-incompatible heart transplantation: a perfusion strategy. Perfusion. 2004; 19(1): 69-72. https://doi.org/10.1191/0267659104pf708oa
- 25Bennett NJ, Tabarani CM, Bartholoma NM, et al. Unrecognized viral respiratory tract infections in premature infants during their birth hospitalization: a prospective surveillance study in two neonatal intensive care units. J Pediatr. 2012; 161(5): 814-818.e3. https://doi.org/10.1016/j.jpeds.2012.05.001
- 26Dipchand AI, West LJ, McCrindle BW, Manlhiot C, Pollock BarZiv SM, VanderVliet M. Equivalent outcomes for pediatric heart transplantation recipients: ABO-blood group incompatible versus ABO-compatible. Am J Transplant. 2010; 10(2): 389-397. https://doi.org/10.1111/j.1600-6143.2009.02934.x
- 27Urschel S, Larsen IM, Kirk R, et al. ABO-incompatible heart transplantation in early childhood: an international multicenter study of clinical experiences and limits. J Hear Lung Transplant. 2013; 32(3): 285-292. https://doi.org/10.1016/j.healun.2012.11.022
- 28Guihaire J, Noly PE, Martin A, et al. Impact of donor comorbidities on heart transplant outcomes in the modern era. Inter CardioVasc Thoracic Surg. 2017; 24(6): 898-904. https://doi.org/10.1093/icvts/ivx014
- 29Laur O, Brisco MA, Kula AJ, et al. The impact of donor and recipient renal dysfunction on cardiac allograft survival: insights into reno-cardiac interactions. J Card Fail 2016; 22(5): 368-375. https://doi.org/10.1016/j.cardfail.2015.11.009.Author
- 30Neugut AI, Ghatak ATMR. Anaphylaxis in the United States: an investigation into its epidemiology. Arch Intern Med. 2001; 161: 15-21. https://doi.org/10.1001/archinte.161.1.15
- 31Odish A, Chen M, Kim AFT. Acquired donor peanut allergy from lung transplantation resulting in respiratory failure: a case report. Transpl Proc. 2018; 50(10): 4085-4086. https://doi.org/10.1016/j.transproceed.2018.08.001
- 32Word C, Klaffky E, Ortiz C, et al. Management of acquired peanut allergy following solid-organ transplant. J Allergy Clin Immunol Pr. 2015; 3(4): 612-614.
- 33Hosakoppal SSBP. Transplant acquired food allergy: current perspectives. J Asthma Allergy. 2017; 10: 307-315.
- 34Huang S, Tang Y, Zhu Z, et al. outcomes of organ transplantation from donors with a cancer history. Med Sci Monit. 2018; 18(24): 997-1007. https://doi.org/10.12659/MSM.909059
- 35Nalesnik MA, Woodle ES, Dimaio JM, et al. Donor-transmitted malignancies in organ transplantation: assessment of clinical risk. Am J Transplant. 2011; 11(6): 1140-1147. https://doi.org/10.1111/j.1600-6143.2011.03565.x
- 36Gambino A, Torregrossa G, Feltrin G, Toscano GGG. Heart donors with underlying genetic syndromes. J Hear Lung Transplant. 2010; 29(5): 588-589.
- 37Ison MG and Nalesnik MA. An update on donor-derived disease transmission in organ transplantation. Am J Transpl. 2011; 11: 1123-1130.
- 38Ison MG, Llatac ECC, Conover CS, et al. Transmission of human immunodeficiency virus and hepatitis C virus from an organ donor to four transplant recipients. Am J Transplant. 2011; 11: 1218-1225.
- 39Green M, Covington S, Taranto S, Michaels MG, Wolfe C, Kaul DR. Pediatrics and donor-derived disease transmission: the US OPTN experience. Pediatr Transplant. 2018; 22(1): 1-5. https://doi.org/10.1111/petr.13115
- 40Seem DL, Lee I, Umscheid CAKM. Excerpt from PHS guideline for reducing HIV, HBV and HCV transmission through organ transplantation. Am J Transplant. 2013; 13: 1953-1962.
- 41Seem DL, Lee I, Umscheid CA, et al. United States public health service: PHS guideline for reducing human immunodeficiency virus, hepatitis B virus, and hepatitis C virus transmission through organ transplantation. Public Heal Rep. 2013; 128: 247-343.
- 42Humar A, Morris M, Blumberg E. Nucleic acid testing (NAT) of organ donors: is the ‘best’ test the right test? A consensus conference report. Am J Transplant J. 2010; 10: 889-899. https://doi.org/10.1111/j.1600-6143.2009.02992.x
- 43Ison MG. Nucleic acid testing of organ donors: is the glass half empty or half full? Am J Transpl. 2015; 15(3): 1743-1745. https://doi.org/10.1111/ajt.13289
- 44Huprikar S, Danziger-Isakov L, Ahn J, et al. Solid organ transplantation from hepatitis B virus-positive donors: consensus guidelines for recipient management. Am J Transplant. 2015; 15: 1162-1172.
- 45Dhillon GS, Levitt J, Mallidi H,, et al. Impact of hepatitis B core antibody positive donors in lung and heart-lung transplantation: an analysis of the united network for organ sharing database. Transplantation. 2009; 88: 842-846.
- 46Schlendorf KH, Zalawadiya S, Shah AS, et al. Early outcomes using hepatitis C-positive donors for cardiac transplantation in the era of effective direct-acting anti-viral therapies. J Heart Lung Transplant. 2018; 37(6): 763-769.
- 47Strabelli TM, Siciliano RF, Vidal Campos S, et al. Toxoplasma gondii myocarditis after adult heart transplantation: successful prophylaxis with pyrimethamine. J Trop Med. 2012. https://doi.org/10.1155/2012/853562
- 48Dávila V, Roncancio-Villamil G, Correa LA, Restrepo C, Madrid CA, González JM. Disseminated toxoplasmosis in a heart transplant patient despite co-trimoxazole prophylaxis: a case report. Biomedica. 2017; 37(3): 303-307.
- 49Chehrazi-Raffle A, Luu M, Yu Z, Liou F, Kittleson M, Hamilton MKJ Toxoplasma gondii serology and outcomes after heart transplantation: contention in the literature. Transpl Proc. 2015; 47(6): 1949-1953.
- 50Barge-Caballero E, Almenar-Bonet L, Crespo-Leiro MG, et al. Preoperative Toxoplasma gondii serostatus does not affect long-term survival of cardiac transplant recipients. Analysis of the Spanish Heart Transplantation Registry. Int J Cardiol. 2018; 250: 183-187.
- 51van Hellemond JJ, van Domburg RT, Caliskan K, Birim OBA Toxoplasma gondii serostatus is not associated with impaired long-term survival after heart transplantation. Transplantation. 2013; 96(12): 1052-1058.
- 52Brügemann J, Kampinga GA, Riezebos-Brilman A, et al. Two donor-related infections in a heart transplant recipient: one common, the other a tropical surprise. J Heart Lung Transplant. 2010; 29(12): 1433-1437. https://doi.org/10.1016/j.healun.2010.08.002
- 53Muñoz J, Gómez-Junyent J, de las Parras ER, et al. Real-time polymerase chain reaction in stool detects transmission of strongyloides stercoralis from an infected donor to solid organ transplant recipients. Am J Trop Med Hyg. 2016; 94(4): 897-899.
- 54Le M, Ravin K, Hasan A, et al. Single donor-derived strongyloidiasis in three solid organ transplant recipients: case series and review of the literature. Am J Transpl. 2014; 14(5): 1199-1206.
- 55Abanyie FA, Gray EB, Delli Carpini KW, et al. Donor-derived strongyloides stercoralis infection in solid organ transplant recipients in the United States, 2009–2013. Am J Transpl. 2015; 15(5): 1369-1375.
- 56Abanyie FA, Valice E, Delli Carpini KW, et al. Organ donor screening practices for Strongyloides stercoralis infection among US organ procurement organizations. Transpl Infect Dis. 2018; 20(3): 4-7. https://doi.org/10.1111/tid.12865
- 57Gómez-Junyent J, Paredes D, Hurtado JC, et al. High seroprevalence of Strongyloides stercoralis among individuals from endemic areas considered for solid organ transplant donation: a retrospective serum-bank based study. PLoS Negl Trop Dis. 2018; 12(11): 1-6. https://doi.org/10.1371/journal.pntd.0007010
- 58Chin-Hong PV, Schwartz BS, Bern C, et al. Screening and treatment of Chagas disease in organ transplant recipients in the United States: Recommendations from the Chagas in transplant working group. Am J Transplant. 2011; 11(4): 672-680. https://doi.org/10.1111/j.1600-6143.2011.03444.x
- 59Montgomery S, Pinney S, Steurer F, et al. Donor-derived Trypanosoma cruzi infection in solid organ recipients in the United States, 2001–2011. Am J Transplant. 2013; 13(9): 2418-2425. https://doi.org/10.1111/ajt.12340
- 60Pinazo M-J, Tendero DT, Ussetti P, et al. Recommendations for management of Chagas disease in organ and hematopoietic tissue transplantation programs in nonendemic areas. Transplant Rev. 2011; 25(3): 91-101. https://doi.org/10.1016/j.trre.2010.12.002
- 61Sabé N, González-Costello J, Oriol I, et al. Donor-transmitted malaria after heart transplant managed successfully with artesunate. Transpl Infect Dis. 2014; 16(6): 999-1002.
- 62Lagunes L, Len O, Sandiumenge A, et al. Successful multiple organ donation after donor brain death due to Actinomyces israelii meningitis. Transpl Infect Dis. 2017; 19(4). https://doi.org/10.1111/tid.12711
- 63Forest SJ, Friedmann P, Bello R, Goldstein DJ, DA Muggia VD. Cardiac transplantation from infected donors: is it safe. J Card Surg. 2015; 30(3): 288-295.
- 64Amdani SM, Du W, Aggarwal S. Outcome of pediatric heart transplantation in blood culture positive donors in the United States. Clin Transplant. 2018; 32(5):e13249. https://doi.org/10.1111/ctr.13249
- 65Galvão LM, de Oliveira APR, Ibanês AS, et al. Fatal case of donor-derived colistin-resistant carbapenemase-producing Klebsiella pneumoniae transmission in cardiac transplantation. Braz J Infect Dis. 2018; 22(3): 235-238. https://doi.org/10.1016/j.bjid.2018.04.005
- 66Ariza-Heredia EJ, Patel R, Blumberg EA, et al. Outcomes of transplantation using organs from a donor infected with Klebsiella pneumoniae carbapenemase (KPC)-producing K pneumoniae. Transpl Infect Dis. 2012; 14(3): 229-236. https://doi.org/10.1111/j.1399-3062.2012.00742.x
- 67Weile J, Eickmeyer H, Dreier J, et al. First case of Mycobacterium tuberculosis transmission by heart transplantation from donor to recipient. Int J Med Microbiol. 2013; 303(8): 449-451. https://doi.org/10.1016/j.ijmm.2013.06.005
- 68Abad CLR, Razonable RR. Donor derived Mycobacterium tuberculosis infection after solid-organ transplantation: a comprehensive review. Transpl Infect Dis. 2018; 20(5):e12971. https://doi.org/10.1111/tid.12971
- 69Nelson JK, Giraldeau G, Montoya JG, Deresinski S, Ho DY, Pham M. Donor-derived Coccidioides immitis endocarditis and disseminated infection in the setting of solid organ transplantation. Open forum Infect Dis. 2016; 3(3): ofw086. https://doi.org/10.1093/ofid/ofw086
- 70Kim S-H, Ha YE, Youn J-C, et al. Fatal scedosporiosis in multiple solid organ allografts transmitted from a nearly-drowned donor. Am J Transplant. 2015; 15(3): 833-840. https://doi.org/10.1111/ajt.13008
- 71Sun H-Y, Alexander BD, Lortholary O, et al. Unrecognized pretransplant and donor-derived cryptococcal disease in organ transplant recipients. Clin Infect Dis. 2010; 51(9): 1062-1069. https://doi.org/10.1086/656584
- 72Blodget E, Geiseler PJ, Larsen RA, Stapfer M, Qazi Y, Petrovic LM. Donor-derived Coccidioides immitis fungemia in solid organ transplant recipients. Transpl Infect Dis. 2012; 14(3): 305-310. https://doi.org/10.1111/j.1399-3062.2011.00698.x
- 73Dierberg KL, Marr KA, Subramanian A, et al. Donor-derived organ transplant transmission of coccidioidomycosis. Transpl Infect Dis. 2012; 14(3): 300-304. https://doi.org/10.1111/j.1399-3062.2011.00696.x
- 74Kusne S, Taranto S, Covington S, et al. Coccidioidomycosis transmission through organ transplantation: a report of the OPTN Ad Hoc Disease Transmission Advisory Committee. Am J Transplant. 2016; 16(12): 3562-3567. https://doi.org/10.1111/ajt.13950
- 75Rosso F, Pineda JC, Sanz AM, Cedano JA, Caicedo LA. Transmission of dengue virus from deceased donors to solid organ transplant recipients: case report and literature review. Brazilian J Infect Dis. 2018; 22(1): 63-69.
- 76Winston DJ, Vikram HR, Rabe IB, et al. Donor-derived West Nile virus infection in solid organ transplant recipients: report of four additional cases and review of clinical, diagnostic, and therapeutic features. Transplantation. 2014; 97(9): 881-889. https://doi.org/10.1097/TP.0000000000000024
- 77Simkins J, Anjan S, Morillas-Rodriguez JA, et al. Screening for Zika virus in deceased organ donors in Florida. Am J Transplant. 2018; 18(3): 731-736. https://doi.org/10.1111/ajt.14582
- 78Farnon EC, Kokko KE, Budge PJ, et al. Transmission of Balamuthia mandrillaris by organ transplantation. Clin Infect Dis. 2016; 63(7): 878-888. https://doi.org/10.1093/cid/ciw422
- 79Kaul DR, Covington S, Taranto S, et al. Solid organ transplant donors with central nervous system infection. Transplantation. 2014; 98(6): 666-670. https://doi.org/10.1097/TP.0000000000000117