Physical activity and aerobic fitness in children after liver transplantation
Abstract
To determine physical activity (PA), aerobic fitness, muscle strength, health-related quality of life (HRQOL), fatigue, and participation in children after liver transplantation. Children, 6-12 years, at least one year after liver transplantation, participated in this cross-sectional study. Measurements: Time spent in moderate to vigorous PA (MVPA) was measured using an accelerometer, and aerobic fitness (VO2 peak) was measured by cardiopulmonary exercise testing. Muscle strength was measured by hand-held dynamometry. Fatigue was measured using the multidimensional fatigue scale, and HRQOL with the Pediatric Quality of life Core scales and leisure activities was measured using the Children's Assessment of Participation and Enjoyment. Outcomes (medians and interquartile range (IQR)) were compared to norm values. Twenty-six children participated in this study (14 boys, age 9.7 years, IQR 7.7;11.4). Children spent 0.8 hours/d (IQR 0.6;1.1) on MVPA. One child met the recommendation of at least 1 hour of MVPA every day of the week. Aerobic fitness was similar to norms (VO2 peak 1.4 L/min, IQR 1.1;1.7, Z-score −0.3). Z-scores of muscle strength ranged between −1.4 and −0.4 and HRQOL and fatigue between −2.3 and −0.4. Participation was similar to published norms (Z-scores between −0.6 and 0.6). Young children after liver transplantation have similar MVPA patterns and aerobic fitness compared to published norms. Despite lower HRQOL, more fatigue, and less muscle strength, these children have similar participation in daily activities. Although children do well, it remains important to stimulate PA in children after liver transplantation in the context of long-term management.
Abbreviations
-
- AT
-
- anaerobic threshold
-
- CAPE
-
- children’s assessment of participation and enjoyment
-
- CPET
-
- cardiopulmonary exercise testing
-
- HRQOL
-
- health-related quality of life
-
- IQR
-
- interquartile range
-
- MELD
-
- model for end-stage liver disease
-
- MVPA
-
- moderate to vigorous physical activity
-
- PA
-
- physical activity
-
- PedsQl
-
- pediatric quality of life inventory
-
- PELD
-
- pediatric end-stage liver disease
-
- RER
-
- respiratory exchange ratio
-
- UMCG
-
- university medical center of Groningen
-
- VCO2
-
- carbon dioxide output
-
- VE
-
- breath-by-breath minute ventilation
-
- VO2 peak
-
- peak oxygen uptake
-
- VO2
-
- oxygen uptake
-
- W max
-
- highest workload
1 INTRODUCTION
New surgical techniques and immune-suppressive medication have improved treatment and survival of children after liver transplantation.1 One-year survival of children undergoing liver transplantation is 93% and 5-year survival 88%.2 In the Netherlands, 5-year survival has increased in the last 20 years from 71% to 83%. Living-related transplantation has a 5-year survival of 95%.3
Unfortunately, these high survival rates come at the cost of considerable co-morbidities including hypertension, atherosclerosis, reduced growth, obesity, lowered bone density, osteoporosis, delayed motor development, increased cardiovascular risk factors, and a reduced aerobic exercise capacity.4-12 Most of these co-morbidities are associated with lowered PA.13, 14 Low PA levels and aerobic fitness in childhood are associated with the presence of metabolic syndrome in adolescents after liver transplantation.15
Several studies were performed to establish that children after liver transplantation have lower PA and aerobic fitness compared to healthy children.4, 5, 11, 16, 17 However, most of these studies have analyzed children in a wider age range or analyzed only adolescents.4, 16 Limited data are available on the PA of young children after liver transplantation. In this study, the focus was put specifically on young children after liver transplantation, since children with a low activity pattern at a young age have a greater chance of a low activity pattern in later life. It is known that children are more active before puberty than after puberty18; we therefore studied levels of PA and inactivity in children after liver transplantation before puberty.
Children with a chronic disease are often restricted in their participation in physical activities which may lead to hypoactivity and deconditioning.19 Therefore, we also studied aerobic fitness, body composition, muscle strength, HRQOL, and fatigue in children after liver transplantation.
The aim of this study was to determine the level of PA and aerobic fitness in children, with an age range of 6–12 years, who underwent a liver transplantation at least one year prior to participating in this study, and compared outcomes to norm data. Additionally, muscle strength, HRQOL, fatigue, body composition, and participation were determined.
2 PATIENTS AND METHODS
Children in the age of 6–12 years who underwent a liver transplantation at the UMCG, the Netherlands, were eligible for this cross-sectional study. The main immunosuppression regimen for these patients consisted of tacrolimus and prednisolone. One year after transplantation, blood through levels of tacrolimus was aimed at 3-6 μg/L, and all patients continued with a low dose of prednisolone of 0.1 mg/kg/d on alternate days.
Since most complications related to the transplantation occur in the first year,1, 20 children were included one year after transplantation, whereby we assumed that children settle in a stable pattern of PA after one year. Other inclusion criteria for this study were a normal graft function, defined as total bilirubin below 10 mmol/L, INR below 1.2, and albumin more than 38 g/L, and being able to follow test instructions. Exclusion criteria for this study were complications that prevented children from performing a maximal exercise test, for example, fractures, or a medical condition that does not allow maximal testing, such as a heart condition. Other exclusion criteria were related to an inability to participate due to cognitive and motor limitations.
The Medical Ethical Committee of the UMCG approved the study (NL48571.042.14). Testing was combined with the regular annual control visit to the outpatient clinic of the UMCG. Children were tested between February 2015 and January 2016.
2.1 Physical activity
PA was measured with an Actical accelerometer (Philips Respironics), during a week in which children went to school. We measured from Saturday to Friday. PA was expressed as time spent in MVPA (mean hours/d), sedentary time (mean hours/d), and mean days meeting recommendations for normal PA, at least one hour of MVPA every day of the week.21
Children were asked to wear a belt with the accelerometer around the waist at the right side for 7 days. The epoch of the accelerometer was set at one minute. The accelerometer was taken off during sleep and wet activities (like taking a shower or swimming). In case of non-wear during wet activities, the child was asked to write down the time and activity. Data were corrected for non-wear if this influenced the total time spent in MVPA or if it affected sedentary time. Scoring of time spent in rest, MVPA, and days meeting recommendations for normal PA was done according to the cutoff points described previously.22
In case of non-wear because of gymnastics at school, 37% of the reported time was recorded as time spent in MVPA because study showed that during gymnastics children spent 37% of the total MVPA time reported on actual MVPA.23 The remaining time was corrected for sedentary time by subtracting this time from time spent in rest, as was also done in case of non-wear because of taking a shower. Correction for other moderate to vigorous sport activities was made by adding the total reported time to the time spent in MVPA, as no observations were available for these sport activities. Sleep time was not included in sedentary time.
In case of non-wear, when children forgot to wear the accelerometer, that day was excluded from the analysis, and totals were divided by the number of valid days. Data had to capture at least one weekend day and 3 weekdays to be included in this study. The wear time on weekdays and weekend days had to be at least 8 and 10 hours, respectively, to be included for analysis. The accelerometer has been validated for children aged 7-18 years,22 and 7-day monitoring provides reliable estimates of PA in children.24 Only data of children who reported PA for 7 days were included in the analysis for meeting recommendations for normal PA.
2.2 Aerobic fitness
Children performed CPET on a cycle ergometer (GE Healthcare) to determine VO2 peak. The Godfrey protocol was used, in which resistance increased every minute depending on height of the child (<120 cm, 10 Watt, 120-150 cm, 15 Watt and >150 cm, 20 Watt).25 The test ended when the patient had to stop because of exhaustion. Heart rate was monitored continuously during the maximal exercise test. Wmax and maximal heart rate were recorded.
VE, VO2, VCO2, and the RER = VCO2/VO2 were calculated through gas analysis (Jaeger, Care Fusion). Maximal effort was achieved if the heart rate was above 180 beats per minute and/or RER ≥ 1.0. Peak (VO2 peak (L/min)) was operationalized as the average value of the last 3 measurements during the test. VO2 peak (ml/kg/min) was determined by dividing the VO2 peak by body weight in kilogram. The ventilatory AT was determined by visual inspection of the Wasserman plots (by GB and OL in consensus). An AT above 40% of predicted VO2 peak (L/min) was considered normal.
For children below the age of 8 years, VO2 peak and Z-scores norm values were calculated by regression analysis from data of children above 8 years,26 since no reference data in children below the age of 8 years were available. CPET up to maximal exertion is considered the gold standard for assessing aerobic fitness. Although during CPET the response is measured objectively, the performance of the test is depending on the motivation to reach maximal effort. Young children can validly perform a CPET if the right equipment is available (pediatric cycle ergometer) and the child is able to understand the instructions.27
2.3 Muscle strength
To determine maximal muscle strength (in newton) in 4 muscle groups (elbow flexors, elbow extensors, hip flexors, and knee extensors) on the left and right side, a hand-held dynamometer was used (Citec dynamometer CT 3001; CIT Technics). Maximal muscle strength was tested with the break method. In the break method, the child delivers maximal power to the hand-held dynamometer until movement of the joint (eccentric contraction of the muscle). Each muscle group was measured three times, and the highest score was recorded. Reliability and validity of measuring muscle strength in children by hand-held dynamometry vary in the previously conducted studies.28, 29 Hand-held dynamometry was chosen as it is easily applicable clinically and Dutch reference values are available.30 We therefore used the described method of that study.
2.4 Health-related quality of life and fatigue
HRQOL was measured by the Paediatric Quality of Life Inventory (PedsQl) Core scales, a 4 subscale (physical, emotional, social, and school functioning) modular instrument.31
Fatigue was measured by the PedsQl multidimensional Fatigue Scale.32 The 18 items were divided over the scales: general fatigue, sleep/rest fatigue, and cognitive fatigue. Feasibility, reliability, and validity were found to be good on both the HRQOL31 and fatigue32 scales of the Dutch version of the PedsQl.
Both parent and child versions of the HRQOL and fatigue questionnaires were completed. Higher scores indicate higher HRQOL and less fatigue. For this study, we made two comparisons, namely child and/or parent report compared to norm data and child report compared to parent report.
2.5 Participation in daily activities
Participation in after-school activities was measured by the CAPE, a child's self-report measure of participation in recreation and leisure activities.33, 34 This questionnaire assesses different domains of participation, namely diversity (which activities does the child do, with a maximum of 55 items), intensity (how often a child does activities, using a 7-point scale ranging from “once in the last 4 months” to “once a day”), and enjoyment (how much does the child enjoy the activity, using a 5-point scale ranging from “not at all” to “love it”). Furthermore, children had to fill in with whom (5-point scale ranging from “alone” to “with others”) and where (6-point scale ranging from “at home” to “outside of town”) the activities were undertaken. The Dutch version of the CAPE is a reliable and valid instrument for measuring participation in daily activity in children with and without physical disabilities aged 6 through 18 years.35 A distinction was made in “formal” (15 items) and “informal” (40 items) activities. Formal activities are structured activities with rules and goals, and a coach or instructor is present (like organized sports or music lessons). Informal activities are mostly initiated by the child, whereby no planning of the activities in advance is required (like reading and play). The activities can be further categorized as recreational (12 items), active physical (13 items), social (10 items), skill-based (10 items), and self-improvement (10 items) activities.
2.6 Participant characteristics
Age, gender, original liver disease, date of transplantation (for calculation of the time since liver transplantation), type and number of liver transplantations, medication, laboratory values (PT, INR, Bilirubin, Albumin, AST, ALT, gamma GT, cholesterol), MELD score, PELD score, type of education, school absenteeism, sport participation, participation in gymnastics at school, and physical therapy were asked or retrieved from the medical files.
Weight (kilogram) and height (centimeters) were measured using an electronic scale and a stadiometer (SECA, Germany). Body mass index was calculated as body weight (kilogram)/height squared (meters). Skinfold measurement was performed at the right-hand side with a caliper (Holtain T/W). Two to three measurements were taken for the biceps, triceps, subscapular, and suprailiac skinfold, averaging those within 1 millimeter of one another. Skinfold was scored as the sum of the 4 recorded skinfolds to express the percentage of body fat.
Data of aerobic fitness,26 muscle strength,30 HRQOL,36 fatigue,32 and participation35, 37 in this study were compared with published norm data of Dutch children. Data of PA were compared with data from a European study because data from the Netherlands were not available.38
2.7 Statistical analysis
2.7.1 Sample size calculation
All pediatric liver transplantations in the Netherlands are performed in our hospital (UMCG). At the time of the design of our study, about 40 children after liver transplantation in the age of 6 to 12 years were seen in the outpatient clinic. In general, Dutch children are on average active for 40.03 minutes per day (SD 16.78).39
The following formula was used for sample size calculation40: n = (u + v)2 *s2/(m−m0),2 where n is the number of participants, u = 0.84, v = 1.96, s is the standard deviation of the norm group, m is the mean PA of the children after liver transplantation, and m0 is the mean PA of the norm group. We assumed it would be feasible to include 26 children after liver transplantation for this study, taking into account possible dropout and non-participation of 35%. With this sample size, we would be able to detect a difference of 9.2 minutes/day or more with the available norm data.39
Data were checked for normal distribution, and Z-scores were calculated as (valuepatient − mean norm)/ Standard deviation(SD) norm.
Wilcoxon signed rank test was performed for differences in child and parent report of the HRQOL and fatigue questionnaire outcome. Wilcoxon signed rank test was also performed for differences in weekdays and weekend days in PA. Mann-Whitney U test was performed for differences in Z-scores of muscle strength between boys and girls. Kruskal-Wallis test was performed for difference between included and excluded children and children who declined. For differences in gender, the chi square test was performed. Spearman's rho test was performed to analyze the association of age with predicted VO2 peak and age with VO2 peak Z-scores. IBM SPSS statistics version 23 was used.
3 RESULTS
We identified 47 children after liver transplantation in the age of 6-12 years who received a liver transplant at least one year earlier (Figure 1). Thirty-six children were eligible for this study. In total, 11 children were excluded from the study, 9 boys (82%), median age of 11.5 years (IQR: 9.2; 12.6), and median 7.9 years (IQR: 5.9; 10.0) post-liver transplantation. Ten children, 5 boys (50%), median age of 11.0 years (IQR: 9.1; 12.8), and median 6.0 years (IQR 2.7; 8.9) post-liver transplantation declined to participate. Not all of the declining participants gave a reason for declining to participate in the study but some indicated it would be an extra burden as the visit takes longer, or too stressful. No significant differences were found in gender (P = 0.24), age (P = 0.20), and time since liver transplantation (P = 0.40) between included and excluded children and children who declined. In total, 26 children (72%) participated in this study (Table 1) of whom 7 children (27%) were below the age of 8 years. All patients had a good graft function. Laboratory values are presented in the Appendix (Table A1).

| Patient characteristics (n = 26) | Median (IQR) | Z-score |
|---|---|---|
| Age, years | 9.7 (7.7; 11.4) | |
| Gender, boys, n (%) | 14 (54%) | |
| Height, centimeters | 138.7 (125.7; 153.1) | −0.4 (−1.2; 0,2) |
| Weight, kilogram | 31.9 (27.2; 40.2) | 0.2 (−0.6; 0.9) |
| Body mass index, kg/m2 | 16.7 (15.8; 18.4) | 0.4 (−0.3; 1.1) |
| Skinfold (sum 4 skinfolds in millimeter) | 31.1 (26.0; 52.9) | Percentile |
| Fat% | 18.2 (14.9; 25.3) | 18.2 (14.9; 24.3) |
| Blood pressure, systolic, mm Hg† | 111.0 (102.5; 114.0) | 72.0 (52.0; 88.0) |
| Blood pressure, diastolic, mm Hg† | 63.0 (56.5; 70.5) | 63.0 (46.5; 75.5) |
| Type of liver disease, n (%) | ||
| Acute liver failure | 5 (19%) | |
| Biliary atresia | 14 (54%) | |
| Alpha 1-antitrypsin deficiency | 3 (12%) | |
| Glycogen storages disorders | 1 (4%) | |
| Hepatoblastoma | 1 (4%) | |
| Tyrosinemia | 2 (8%) | |
| Time since liver transplantation, years | 7.5 (4.2; 9.9) | |
| Type of liver transplantation, n (%) | ||
| Partial (of which 4 living related) | 23 (88%) | |
| Full size | 3 (12%) | |
| Number of transplantations, n (%) | ||
| 1 | 22 (85%) | |
| 2 or more | 4 (15%) | |
| Medication, n (%) | ||
| Tacrolimus | 24 (92%) | |
| Cyclosporine | 1 (4%) | |
| Prednisolone | 21 (81%) | |
| Antihypertensive medication | 2 (8%) | |
| PELD | 8.0 (1.5; 25.8) | |
| MELD | 18.0 (10.0; 28.5) | |
Four patients had one or more re-transplantations: two within 2 weeks because of vascular problems of the first graft, and 2 after 2 and 6 years respectively because of biliary complications of the first graft.
3.1 Physical activity and aerobic fitness
The Actical was worn by 21 children. In 6 children, corrections for non-valid days were made. In 6 other children, data were corrected for MVPA in case of non-wear (in total 5 hours for swimming activities, gymnastics at school, and horse jumping games) (Table 2). In 16 children, sedentary time was corrected for non-wear because of showering during the day (in total 26.9 hours).
| Physical activity (n = 21) | Median (IQR) | Percentile |
|---|---|---|
| Total MVPA(hours/day) | 0.8 (0.6; 1.1) | 93.0 (75.0; 96.0) |
| MVPA weekday(hours/day) | 0.9 (0.7; 1.2)* | |
| MVPA weekend day(hours/day) | 0.5 (0.3; 1.1) | |
| Total sedentary time(hours/day) | 7.9 (6.5; 9.4) | 3.0 (1.0; 25.0) |
| Sedentary time weekday(hours/day) | 8.3 (6.7; 9.4)** | |
| Sedentary time weekend day(hours/day) | 6.9 (6.3; 9.4) | |
| Meeting public health recommendations(days/week)† | 2.0 (2.0; 5.0) |
No significant differences were found in weekend days and weekdays for duration of MVPA (P = 0.17) or sedentary time (P = 0.24). One child met public health recommendations for normal PA.
3.2 Aerobic fitness
CPET was performed in 24 children (92%). One child was afraid of wearing the mask, and one child was not able to perform the test at the right speed; therefore, the VO2 peak could not be determined. Of the 24 children, 2 children did not reach maximal effort and were excluded for further analysis.
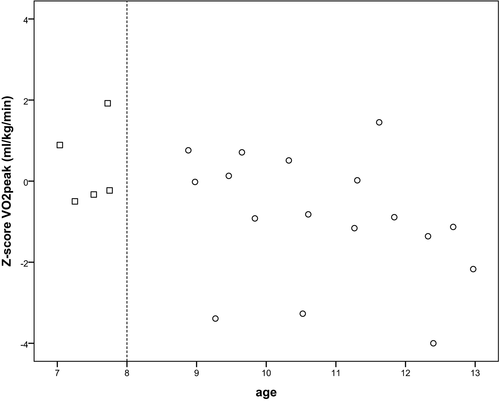
Five children were below the age of 8 years (3 girls and 2 boys). For these children, extrapolated data from norm values26 were used to calculate Z-scores. Both results of aerobic fitness without extrapolated data and with extrapolated data are shown in Table 3. This is also shown in the appendix (Figure A1) as we plotted VO2 peak ml/kg/min Z-scores against age. The correlation coefficient of predicted VO2 peakl/min with age was −0.48 (P = 0.02), and that of age and Z-score of VO2 peakl/min was −0.43 (P = 0.05). The correlation coefficient of predicted VO2 peak ml/kg/min with age was −0.53 (P = 0.01), and that of age and Z-score of VO2 peak ml/kg/min was −0.52 (P = 0.01).
| Aerobic fitness | Median (IQR) | % predicted | Z-score |
|---|---|---|---|
| VO2 peak (L/min) | 1.4 (1.1; 1.7)† | 93 (77; 98)‡ | −0.5 (−1.6; −0.14)‡ |
| Extrapolated | 96 (79; 101)¶ | −0.3 (−1.5; 0.1)¶ | |
| VO2 peak (ml/kg/min) | 41.6 (36.2; 44.3)† | 89 (77; 104)‡ | −0.9 (−1.8; 0.3)‡ |
| Extrapolated | 95 (85; 107)¶ | −0.4 (−1.2; 0.6)¶ | |
| Anaerobic threshold | 0.84 (0.72; 0.99)§ | ||
| Anaerobic threshold of predicted VO2 peak, % | 52 (46; 67)§ | ||
| Extrapolated | 55 (48; 67)† |
Note
- Z-scores calculated as (VO2 peak − VO2 peak norm)/standard deviation norm. Norm by Bongers26. For children younger than 8 years, regression equations were used as described by Bongers26 and standard deviations were extrapolated by regression analysis.
- † n = 20,
- ‡ n = 17,
- § n = 16,
- ¶ n = 22 valid observations.
3.3 Muscle strength
Muscle strength was tested in all 26 children (Table 4). Z-scores of muscle strength ranged between −1.4 and −0.4. No significant differences were found in Z-scores between boys and girls, with the exception of elbow flexion for both sides (P = 0.03).
| Muscle strength (n = 26) |
Right side Median (IQR) |
Z-score Median (IQR) |
Left Side Median (IQR) |
Z-score Median (IQR) |
|---|---|---|---|---|
| Elbow flexors (N) | 103 (76; 132) | −1.3 (−2.3; −0.5) | 109 (78; 132) | −1.4 (−2.2; −0.5) |
| Elbow extensors (N) | 68 (57; 77) | −1.3 ( −1.7; −0.8) | 72 (56; 81) | −1.0 (−1.7; −0.7) |
| Knee extensors (N) | 160 (129; 187) | −0.9 (−1.3; −0.4) | 160 (117; 182) | −1.2 (−1.5; −0.6) |
| Hip flexors (N) | 179 (138; 226) | −0.4 (−1.4; 0.2) | 167 (116; 219) | −0.8 (−1.6; −0.2) |
Note
- Z-scores calculated as (muscle strength in N – muscle strength norm in N)/standard deviation norm. Norm by Beenakker et al.30
- Abbreviation: N, newton.
3.4 Health-related quality of life and fatigue
HRQOL and fatigue questionnaires were absent for 1 child. All parents filled in both questionnaires. Z-scores of HRQOL could only be calculated for parent report in children aged 5-7 years and for child report in children 8-12 years (Table 5). Z-scores of HRQOL and fatigue ranged between −2.3 and 0.4.
| HRQOL and Fatigue |
Child report Median (IQR) |
Child Z-score Median (IQR) |
Parent report Median (IQR) |
Parent Z-score Median (IQR) |
P |
|---|---|---|---|---|---|
| HRQOL | (n = 25) | (n = 18)† | (n = 26) | (n = 7) ‡ | |
| Total score | 75.0 (64.1; 80.4) | −1.0 (−2.3; −0.5) | 71.2 (57.6; 84.2) | −2.3 (−3.1; −0.2) | 0.87 |
| Physical functioning | 81.3 (67.2; 92.2) | −0.8 (−2.2; 0.6) | 84.4 (58.6; 91.4) | −1.5 (−3.5; 0.2) | 0.99 |
| Psychosocial functioning | 70.0 (60.0; 80.0) | −1.0 (−2.2; −0.1) | 64.8 (55.0; 81.7) | −1.8 (−2.4; −0.2) | 0.57 |
| Emotional functioning | 65.0 (57.5; 82.5) | −0.9 (−1.6; 0.3) | 66.9 (50.0; 80.0) | −0.6 (−1.9; 0.6) | 0.37 |
| Social functioning | 80.0 (65.0; 92.5) | −0.7 (−1.8; 0.7) | 70.0 (63.8; 90.0) | −1.1 (−2.8; −0.2) | 0.25 |
| School functioning | 70.0 (50.0; 72.5) | −1.2 (−2.4; −0.3) | 65.0 (48.8; 75.0) | −2.0 (−2.9; −1.5) | 0.71 |
| Fatigue | (n = 25) | (n = 25) | (n = 26) | (n = 26) | |
| General fatigue | 70.8 (58.3; 85.4) | −0.9 (−1.8; 0.2) | 62.5 (47.9; 87.5) | −1.4 (−2.8; 0.4) | 0.64 |
| Sleep/rest fatigue | 70.8 (60.4; 77.1) | −0.4 (−0.9; 0.1) | 75.0 (68.8; 95.8) | −0.8 (−1.5; 0.8) | 0.03 |
| Cognitive fatigue | 75.0 (47.9; 77.1) | −0.4 (−1.5; 0.2) | 58.3 (41.7; 75.0) | −1.0 (−1.8; −0.1) | 0.48 |
| Total fatigue | 66.7 (62.5; 81.3) | −0.9 (−1.3; 0.3) | 64.6 (51.0; 83.7) | −1.4 (−2.4; 0.2) | 0.61 |
A significant difference in child and parent report was only found in sleep/rest fatigue (P = 0.03), children reported lower scores of sleep/rest fatigue compared to the parents.
3.5 Participation
The CAPE questionnaire was missing for one child. Not all subscores could be calculated of all children because of missing values (Table 6). Diversity Z-scores and intensity Z-scores ranged from −0.6 to 0.6. No differences were found in children after liver transplantation and norm values in formal an informal participation in daily activities. If participation was divided into different categories, the biggest difference between children after liver transplantation and the published norms was found in social participation, and both diversity and intensity Z-scores were negative, −0.6 and −0.4, respectively.
| Participation |
Diversity Median (IQR) |
Intensity Median (IQR) |
With whom Median (IQR) |
Where Median (IQR) |
Enjoyment Median (IQR) |
Z-scores Diversity Median (IQR) |
Z-score Intensity Median (IQR) |
|---|---|---|---|---|---|---|---|
| Overall | 28.0 (25.0; 33.5)† | 2.4 (2.0; 2.7)‡ | 2.4 (2.25; 2.8)‡ | 2.5 (2.3; 2.9)> | 4.3 (4.1; 4.4)¶ | ||
| Formal | 4.0 (3.0; 5.5)† | 1.1 (0.8; 1.5)† | 4.0 (3.0; 4.3)¶ | 4.0 (3.3; 4.6)§ | 4.5 (4.0; 4.8)¶ | 0.3 (−0.2; 1.1)† | |
| Informal | 25.0 (21.0; 28.0)† | 2.9 (2.4; 3.2)‡ | 2.3 (2.0; 2.5)‡ | 2.3 (2.1; 2.7)> | 4.3 (3.9; 4.4)§ | 0.2 (0.2; 0.8)† | |
| Recreational | 9.0 (8.0; 11.0)† | 4.0 (3.3; 5.1)§ | 2.1 (1.7; 2.4)¶ | 1.8 (1.5; 2.0)¶ | 4.2 (4.0; 4.5)§ | 0.5 (0.0; 1.4)† | 0.5 (0.0; 1.5)§ |
| Active physical | 4.0 (2.0; 6.0)† | 1.5 (0.9; 2.0)† | 3.3 (2.7; 3.9)§ | 3.3 (3.0; 4.3)§ | 4.3 (3.6; 4.8)§ | −0.2 (−1.2; 0.8)† | −0.2 (−0.9; 0.5)† |
| Social | 6.0 (5.0; 8.0)† | 2.5 (1.9; 2.9)§ | 2.5 (2.4; 2.8)§ | 2.7 (2.4; 3.1)§ | 4.7 (4.5; 4.8)§ | −0.6 (−1.1; 0.4)† | −0.4 (−0.9; 0.3)§ |
| Skill-based | 3.0 (2.0; 5.0)† | 1.5 (0.7; 1.9)§ | 3.5 (2.8; 4.3)§ | 3.0 (2.8; 4.2)‡ | 4.6 (4.3; 4.9)§ | 0.3 (−0.4; 1.5)† | 0.5 (−0.5; 1.0)§ |
| Self-improvement | 6.0 (5.0; 6.0)† | 2.5 (1.9; 3.3)¶ | 1.9 (1.4; 2.4)¶ | 2.8 (2.2; 3.4)¶ | 3.5 (2.9; 4.0)† | 0.6 (0.1; 0.6)† | 0.1 (−0.4; 0.9)¶ |
Note
- Range of diversity scores: overall 0-55, formal 0-15, informal 0-40, recreational 0-12, active physical 0-13, social 0-10, skill-based 0-10, self-improvement 0-10. Range of intensity scores: 1 = once in four months, 2 = twice in 4 months, 3 = once a month, 4 = 2-3 times per month, 5 = once a week, 6 = 2-3 times per week, 7 = once a day. Range of with whom scores: 1 = alone, 2 = with family members, 3 = with family, 4 = with friends, 5 = with others. Range of where scores: 1 = at home, 2 = at family, 3 = in the neighborhood, 4 = at school (but not during school), 5 = in the village of town, 6 = outside the village or town.
- Range of enjoyment: 1 = not at all, 2 = somewhat, 3 = pretty much, 4 = very much, 5 = love it.
- Z-score calculated as for diversity: (diversity score/ diversity score by Bult et al37)/standard deviation by Bult et al37 and for intensity: (intensity score/ intensity score by Bult et al35)/standard deviation by Bult et al.35
- † n = 25.
- ‡ n = 22.
- § n = 24.
- ¶ n = 23.
- > n = 21 valid observations.
3.6 Education and participation
Nineteen of 26 children (61%) followed regular education, and 7 children (27%) followed special education. None of the children missed school related to the liver transplantation. In total, 17 out of 25 children participated in organized sports, of which 9 for more than 3 times a week. Twenty-three out of 25 children participated in gymnastics at school, and 3 children out of 25 had physical therapy.
4 DISCUSSION
This study showed that, at least one year after liver transplantation, children aged 6 to 12 year are similarly physically active compared to published European norms, spend less time on sedentary activities, and have a normal aerobic fitness, but they do not reach the recommendation of one hour of MVPA each day.21 Parents underestimated the children's experience of sleep/rest fatigue. The participation of children with a liver transplant in out-of-school activities was similar to Dutch norm values, and they enjoyed these activities highly.
The PA levels (time spent in MVPA) of our children are similar to healthy European published norms,38 but are somewhat less active compared to healthy Canadian children (about 1 hour/d).41 After liver transplantation, our children spent less time in sedentary time compared to healthy European published norms.38
Compared to Canadian children after liver transplantation, our group spent more time in MVPA.16 In that study, only 0.5 hour/d was spent in MVPA and none of the children met the PA recommendations,16 children were on average 14 years old, and PA levels decline with an increasing age.18, 42
In a Dutch questionnaire study in healthy children in the age of 4 to 11 years, 21% met PA recommendations.18 In the European study, the adherence to the PA recommendations of 1 hour of MVPA each day differed between countries from 2% in Cyprian girls to 34% in Belgian boys.38
Sedentary time is given increasing attention considering the long-term negative effects on health.19 In our study, we found that children after liver transplantation spent less time on sedentary activities than European published norms.38 We found no significant differences in weekdays/schooldays (median 8.3 hours/d) compared to weekend days (median 6.9 hours/d), whereas in the previously mentioned questionnaire study, sedentary time for weekdays was on average 7.3 hours/d and for weekend days 4.1 hours/d.18 It is known that PA questionnaires have limited reliability and validaty.43
Aerobic fitness in this study was similar to that of the healthy population. Other studies in children after liver transplantation found lower predicted values for VO2 peak, 90.5%11 and 77%.16 These studies were done in children with a mean age of 11.6 and 14.0 years. We found that there was an inverse relation between percentage of predicted VO2 peak and age and Z-scores of VO2 peak and age. This might explain the difference between our results and the results of previous studies11, 16; our children were younger. As shown in the appendix (Figure A1) Z-scores seem to decrease with age.
Muscle strength in our children was overall lower than that of Dutch norm values. This difference was also found in previous studies.4, 5 We have chosen to measure muscle strength with a hand-held dynamometer, because it is easy clinically applicable and Dutch norm values for children are available. In one study in children after liver transplantation, quadriceps muscle strength was measured with a Biodex (peak torque).4 In that study, a difference between boys and girls was found: Girls had 50% lower scores compared to age and sex-predicted norm values for the Biodex measurements and boys achieved 78% of the norm.4 In our study, we did not find differences in boys and girls in Z-scores of quadriceps muscle strength.
Similar to previous studies, we found both child report (only age 8-12 years) and parent report (only age 5-7 years) on HRQOL were lower in this study compared to published healthy norms.11, 44-46 School functioning showed the largest difference between children after liver transplantation and healthy norms, probably based on frequent school absenteeism. In our study, there was hardly any school absenteeism, but we found the largest difference with healthy published norms in school functioning as in another study.44
Fatigue is one of the most common complaints in adult liver transplantation patients.47 Both parent report and child report showed a higher level of fatigue compared to published healthy norms, and these findings are similar to other children after liver transplantation.16, 17 Children in our study reported more sleep/rest fatigue compared to their parents, meaning parents underestimate the children's experience of sleep/rest fatigue. No differences were found between child and parent report on HRQOL in our study, other studies report a moderate ability of caregivers to report on behalf of their children, and it is suggested to gain insight in both the perspective of the child and the parents.44, 46 In a study interviewing both children after liver transplantation and their parents, it was found that children's perspective tended to relate to the present whereas parents reflected more to a future perspective.48 In the context of long-term management of health benefits, children need to learn about the importance of a lifelong need for immunosuppression and about the benefits of PA. For health benefits, it is important to be physically active on all days of the week for at least one hour of MVPA.
Participation in recreation and leisure activities is important for children, because they learn new skills and competencies. In this study, participation is similar to healthy published norms regarding diversity and intensity scores. Children after liver transplantation scored high on enjoyment. In this study, 68% (n = 17) of the children participate in organized sports.
Our study has some limitations. Studying a control group particularly with younger children would have strengthened our results. Unfortunately, no reference data of Dutch children were available for PA in the age of 6 to 12 years measured with the Actical accelerometer; therefore, we used European reference values.38 In that study, a different accelerometer was used, and although we compared our data with the scores of the same cutoff points as in our study, there might be differences. When designing the study, we intended to use the reference data of Dutch children, but in that study, children were on average 13.4 years.39 Reference data of the European children became available while performing the study. Although we made corrections for non-wear to do justice to the time spent in MVPA, there might be an overestimation of the real time spent in MVPA as we corrected for the full reported time, knowing that studies in gymnastics at school show that only 37% of the reported time is spent in MVPA.23 One can imagine the same applies for activities reported during non-wear, but since no studies were available for other activities, we have chosen to correct these activities for the reported time. The same applies for sedentary time. If we did not make the corrections by subtracting the reported activities during non-wear from the total sedentary time, we would have overestimated sedentary time, considering that we did not actually know the real intensity of the reported activity. Correction for non-wear was negligible on the total PA time.
No norm values for aerobic fitness were available in children below the age of 8 years. We wanted to get more insight in especially young children and chose to extrapolate available data with all the known limitations of this method.
The last limitation of this study is the small sample. Since our center is the only pediatric liver transplant center in the Netherlands and we wanted to focus on the young children, we were not able to increase the sample, but we had 72% participation. In total, 10 children declined to participate in this study (no significant differences in age, gender, and time since liver transplantation) which might cause potential bias. The small group especially applied for calculating Z-scores on HRQOL, since these calculations could not be made for HRQOL child report in the age of 5-7 years and HRQOL parent report in the age of 8-12 year as no norm data were available. The small sample also makes the population somewhat heterogeneous; several participants were well prior to transplantation, while others were chronically ill, which could influence the outcome of the measures.
Despite the limitations of the study and the sample, this study provides insight in PA, aerobic fitness, muscle strength, HRQOL, fatigue, and participation in young children after liver transplantation.
In conclusion, young children after liver transplantation have similar MVPA patterns, spend less time on sedentary activities compared to published healthy norms, and have normal levels of aerobic fitness. Both HRQOL and muscle strength are overall lower and children experience more fatigue compared with published norms, but this does not limit these children in participation of daily activities. Participation levels are similar to published healthy norms and are rated highly on enjoyment. Although children do well, in the context of long-term management, it remains important to stimulate PA in children after liver transplantation.
ACKNOWLEDGMENTS
Human movement scientist students for helping collecting data or checking data Froukje Dijkstra, Laura Golenia, and Evelien Brakelé. Funding: Stichting Vrienden Beatrix Kinderziekenhuis.
CONFLICT OF INTEREST
The authors declare no conflicts of interest.
AUTHOR CONTRIBUTION
GJF Joyce Bos: Participated in research design, conducted testing (data collection), data analysis, and writing the paper. Otto THM Lelieveld: Participated in research design, conducted testing (data collection), and writing the paper. Rene Scheenstra: Recruited the subjects, participated in research design, and reviewed the paper critically. Pieter JJ Sauer: Participated in research design and writing the paper. Jan HB Geertzen: Participated in research design and writing the paper. Pieter U. Dijkstra: Participated in research design, data analysis, writing the paper, and supervised the project.
Appendix A
| Laboratory value (n = 26) | Mean (SD) | |
|---|---|---|
| PT sec (9-12) | 11.71 (0.69) | |
| INR | 1.13 (0.08) | |
| Total bilirubin (μmol/L) | 9.31 (6.93) | |
| Albumin (g/L) | 44.73 (2.30) | |
| AST (U/L) | 35.27 (9.76) | |
| ALT (U/L) | 23.31 (8.29) | |
| Gamma GT (U/L) | 56.08 (109.14) | |
| Cholesterol mmol/L | 3.36 (0.58) | |
| Percentile 5 | 9 (35%) | |
| Percentile 75 | 16 (62%) | |
| Percentile 95 | 1 (4%) |
- n, valid observations.
- †n = 24. Norm value cholesterol by Kliegman et al.52




