Late acute rejection: Incidence, risk factors, and effect on graft survival and function
Loai Eid
Department of Nephrology, Children's National Medical Center, Washington, DC, USA
Search for more papers by this authorShamir Tuchman
Department of Nephrology, Children's National Medical Center, Washington, DC, USA
Search for more papers by this authorCorresponding Author
Asha Moudgil
Department of Nephrology, Children's National Medical Center, Washington, DC, USA
Asha Moudgil, Department of Nephrology, Children's National Medical Center, 1.5 -100, West Wing, 111, Michigan Avenue, NW, Washington, DC 20010, USA
Tel.: 202 476 5058
Fax: 202 467 3475
E-mail: [email protected]
Search for more papers by this authorLoai Eid
Department of Nephrology, Children's National Medical Center, Washington, DC, USA
Search for more papers by this authorShamir Tuchman
Department of Nephrology, Children's National Medical Center, Washington, DC, USA
Search for more papers by this authorCorresponding Author
Asha Moudgil
Department of Nephrology, Children's National Medical Center, Washington, DC, USA
Asha Moudgil, Department of Nephrology, Children's National Medical Center, 1.5 -100, West Wing, 111, Michigan Avenue, NW, Washington, DC 20010, USA
Tel.: 202 476 5058
Fax: 202 467 3475
E-mail: [email protected]
Search for more papers by this authorAbstract
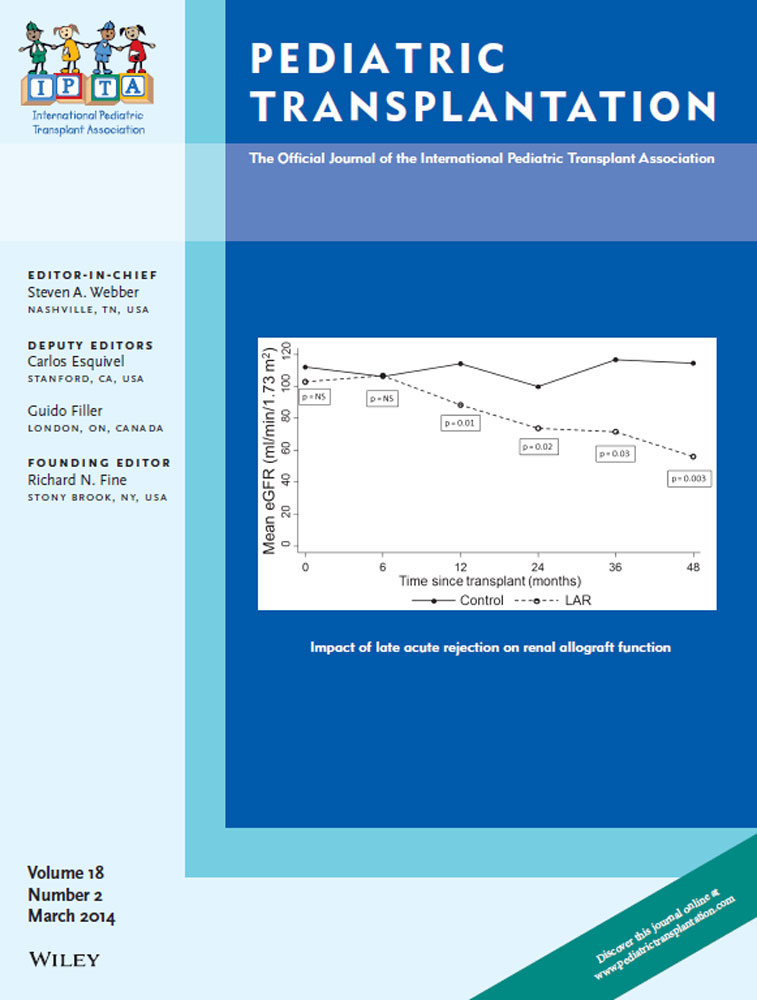
Long-term graft survival and function has not kept pace with short-term success in kidney transplant (Tx) recipients. LAR ≥6 months post-Tx may contribute to lack of improvement; risk factors for LAR are not well known. Of 64 Tx recipients followed over six yr, 23 (35.9%) had LAR (LAR group) and 41 had no LAR (no LAR group). Of all variables, significant risk factors for LAR included DGF, (43.4% LAR vs. 14.6% in no LAR group, p = 0.0096); de novo DSA (65.2% vs. 26.8%, p = 0.003); mean COV% of TAC (41.8% vs. 34.6%, p = 0.03); and non-adherence (34.8% vs. 7.3%, p = 0.0043). DGF and DSA remained statistically significant (p = 0.002 and 0.003, respectively); COV% TAC had borderline significance (p = 0.057), and non-adherence was not significant on multivariate regression analysis. Patients with LAR had inferior graft survival and function, whereas graft function was stable in the no LAR group over a mean follow-up of 31.2 months. Patients with de novo DSA and DGF should be considered at risk of LAR; an early diagnosis and treatment of LAR may improve graft survival and function.
References
- 1 NAPRTCS Annual Report. [database on the Internet]. [cited August 20, 2013]. Available at: http://web.emmes.com/study/ped/annlrept/2010_Report.pdf.
- 2Matas AJ, Smith JM, Skeans MA, et al. OPTN/SRTR 2011 annual data report: Kidney. Am J Transplant 2013: 13(Suppl 1): 11–46.
- 3Hwang AH, Cho YW, Cicciarelli J, Mentser M, Iwaki Y, Hardy BE. Risk factors for short- and long-term survival of primary cadaveric renal allografts in pediatric recipients: A UNOS analysis. Transplantation 2005: 80: 466–470.
- 4Meier-Kriesche HU, Schold JD, Srinivas TR, Kaplan B. Lack of improvement in renal allograft survival despite a marked decrease in acute rejection rates over the most recent era. Am J Transplant 2004: 4: 378–383.
- 5Fletcher JT, Nankivell BJ, Alexander SI. Chronic allograft nephropathy. Pediatr Nephrol 2009: 24: 1465–1471.
- 6Leggat JE Jr, Ojo AO, Leichtman AB, et al. Long-term renal allograft survival: Prognostic implication of the timing of acute rejection episodes. Transplantation 1997: 63: 1268–1272.
- 7Opelz G, Dohler B. Influence of time of rejection on long-term graft survival in renal transplantation. Transplantation 2008: 85: 661–666.
- 8Sijpkens YW, Doxiadis II, Mallat MJ, et al. Early versus late acute rejection episodes in renal transplantation. Transplantation 2003: 75: 204–208.
- 9Morrissey PE, Reinert S, Yango A, Gautam A, Monaco A, Gohh R. Factors contributing to acute rejection in renal transplantation: The role of noncompliance. Transpl Proc 2005: 37: 2044–2047.
- 10Alexopoulos E, Papadimitriou M. Late-acute renal allograft rejection and symptomless cytomegalovirus infection. Lancet 1995: 345: 794.
- 11Babel N, Schwarzmann F, Prang N, et al. Association between Epstein-Barr virus infection and late acute transplant rejection in long-term transplant patients. Transplantation 2001: 72: 736–739.
- 12Tan JY, Zhao N, Wu TX, et al. Steroid withdrawal increases risk of acute rejection but reduces infection: A meta-analysis of 1681 cases in renal transplantation. Transpl Proc 2006: 38: 2054–2056.
- 13Hall BM, Bishop GA, Duggin GG, Horvath JS, Philips J, Tiller DJ. Increased expression of HLA-DR antigens on renal tubular cells in renal transplants: Relevance to the rejection response. Lancet 1984: 2: 247–251.
- 14Hardinger KL. Rabbit antithymocyte globulin induction therapy in adult renal transplantation. Pharmacotherapy 2006: 26: 1771–1783.
- 15Yarlagadda SG, Coca SG, Garg AX, et al. Marked variation in the definition and diagnosis of delayed graft function: A systematic review. Nephrol Dial Transplant 2008: 23: 2995–3003.
- 16Schwartz GJ, Haycock GB, Edelmann CM Jr, Spitzer A. A simple estimate of glomerular filtration rate in children derived from body length and plasma creatinine. Pediatrics 1976: 58: 259–263.
- 17Levey AS, Bosch JP, Lewis JB, Greene T, Rogers N, Roth D. A more accurate method to estimate glomerular filtration rate from serum creatinine: A new prediction equation. Modification of Diet in Renal Disease Study Group. Ann Intern Med 1999: 130: 461–470.
- 18Tait BD, Susal C, Gebel HM, et al. Consensus guidelines on the testing and clinical management issues associated with HLA and non-HLA antibodies in transplantation. Transplantation 2013: 95: 19–47.
- 19Sis B, Mengel M, Haas M, et al. Banff ‘09 meeting report: Antibody mediated graft deterioration and implementation of Banff working groups. Am J Transplant 2010: 10: 464–471.
- 20Bock HA. Steroid-resistant kidney transplant rejection: Diagnosis and treatment. J Am Soc Nephrol 2001: 12(Suppl 17): S48–S52.
- 21Hsiau M, Fernandez HE, Gjertson D, Ettenger RB, Tsai EW. Monitoring nonadherence and acute rejection with variation in blood immunosuppressant levels in pediatric renal transplantation. Transplantation 2011: 92: 918–922.
- 22Wood KJ, Goto R. Mechanisms of rejection: Current perspectives. Transplantation 2012: 93: 1–10.
- 23Narayanan R, Cardella CJ, Cattran DC, et al. Delayed graft function and the risk of death with graft function in living donor kidney transplant recipients. Am J Kidney Dis 2010: 56: 961–970.
- 24Yarlagadda SG, Klein CL, Jani A. Long-term renal outcomes after delayed graft function. Adv Chronic Kidney Dis 2008: 15: 248–256.
- 25Wever KE, Wagener FA, Frielink C, et al. Diannexin protects against renal ischemia reperfusion injury and targets phosphatidylserines in ischemic tissue. PLoS ONE 2011: 6: e24276.
- 26Hidalgo LG, Campbell PM, Sis B, et al. De novo donor-specific antibody at the time of kidney transplant biopsy associates with microvascular pathology and late graft failure. Am J Transplant 2009: 9: 2532–2541.
- 27Lederer SR, Kluth-Pepper B, Schneeberger H, Albert E, Land W, Feucht HE. Impact of humoral alloreactivity early after transplantation on the long-term survival of renal allografts. Kidney Int 2001: 59: 334–341.
- 28Wiebe C, Gibson IW, Blydt-Hansen TD, et al. Evolution and clinical pathologic correlations of de novo donor-specific HLA antibody post kidney transplant. Am J Transplant 2012: 12: 1157–1167.
- 29Lee PC, Terasaki PI, Takemoto SK, et al. All chronic rejection failures of kidney transplants were preceded by the development of HLA antibodies. Transplantation 2002: 74: 1192–1194.
- 30Chaudhuri A, Ozawa M, Everly MJ, et al. The clinical impact of humoral immunity in pediatric renal transplantation. J Am Soc Nephrol 2013: 24: 655–664.
- 31Staples B, Bravender T. Drug compliance in adolescents: Assessing and managing modifiable risk factors. Paediatr Drugs 2002: 4: 503–513.
- 32Cecka JM, Gjertson DW, Terasaki PI. Pediatric renal transplantation: A review of the UNOS data. United Network for Organ Sharing. Pediatr Transplant 1997: 1: 55–64.
- 33Jarzembowski T, John E, Panaro F, et al. Impact of non-compliance on outcome after pediatric kidney transplantation: An analysis in racial subgroups. Pediatr Transplant 2004: 8: 367–371.
- 34Falkenstein K, Flynn L, Kirkpatrick B, Casa-Melley A, Dunn S. Non-compliance in children post-liver transplant. Who are the culprits? Pediatr Transplant 2004: 8: 233–236.
- 35Cleemput I, Kesteloot K, Vanrenterghem Y, de Geest S. The economic implications of non-adherence after renal transplantation. PharmacoEconomics 2004: 22: 1217–1234.
- 36Chisholm-Burns MA, Spivey CA, Rehfeld R, Zawaideh M, Roe DJ, Gruessner R. Immunosuppressant therapy adherence and graft failure among pediatric renal transplant recipients. Am J Transplant 2009: 9: 2497–2504.
- 37Pollock-Barziv SM, Finkelstein Y, Manlhiot C, et al. Variability in tacrolimus blood levels increases the risk of late rejection and graft loss after solid organ transplantation in older children. Pediatr Transplant 2010: 14: 968–975.